Alifus 250 Accuhaler
Out of date information, search another1. What Seretide is and what it is used for

PACKAGE LEAFLET: ^ INFORMATION FOR THE USER SERETIDE ® 250 ACCUHALER®
(salmeterol xinafoate / fluticasone propionate)
The name of your medicine is Seretide 250 Accuhaler but throughout the remainder of this leaflet it will be referred to as Seretide.
This product is available in multiple strengths and all strengths will be referred to throughout this leaflet.
Outer Case
Mouthpiece

Lever
Counter Full Empty
(60 (0
Thumbgrip
Read all of this leaflet carefully before you start taking this
medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms and signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist . This includes any possible side effects not listed in this leaflet. See section 4.
In this leaflet:
1. What Seretide is and what it is used for
2. What you need to know before you use Seretide
3. How to use Seretide
4. Possible side effects
5. How to store Seretide
6. Contents of the pack and other information
Seretide contains two medicines, salmeterol and fluticasone propionate:
• Salmeterol is a long-acting bronchodilator. Bronchodilators help the airways in the lungs to stay open. This makes it easier for air to get in and out. The effects last for at least 12 hours.
• Fluticasone propionate is a corticosteroid which reduces swelling and irritation in the lungs.
The doctor has prescribed this medicine to help prevent breathing
problems such as:
• Asthma
• Chronic Obstructive Pulmonary Disease (COPD). Seretide Accuhaler, at a dose of 50/500 micrograms, reduces the number of flare ups of COPD symptoms.
You must use Seretide every day as directed by your doctor. This will make sure that it works properly in controlling your asthma or COPD.
Seretide helps to stop breathlessness and wheeziness coming on. However Seretide should not be used to relieve a sudden attack of breathlessness or wheezing. If this happens you need to use a fast -acting ‘reliever' (‘rescue') inhaler, such as salbutamol. You should always have your fast-acting ‘rescue' inhaler with you.
2. What you need to know before you use Seretide
Do not take Seretide if:
You are allergic (hypersensitive) to salmeterol, fluticasone propionate or to the other ingredient lactose monohydrate.
Warnings and precautions
Your doctor will supervise your treatment more closely if you have medical conditions such as:
• Heart disease, including an irregular or fast heart beat
• Overactive thyroid gland
• High blood pressure
• Diabetes mellitus (Seretide may increase your blood sugar)
• Low potassium in your blood
• Tuberculosis (TB) now or in the past, or other lung infections
If you have ever had any of these conditions, tell your doctor before you use Seretide.
Other medicines and Seretide
Tell your doctor or pharmacist if you are taking or have recently taken any other medicines. This includes medicines for asthma or any medicines obtained without a prescription. This is because Seretide may not be suitable to be taken with some other medicines.
Tell your doctor if you are taking the following medicines, before starting to use Seretide:
• p blockers (such as atenolol, propranolol and sotalol). p blockers are mostly used for high blood pressure or other heart conditions.
• Medicines to treat infections (such as ritonavir, ketoconazole, itraconazole and erythromycin). Some of these medicines may increase the amount of fluticasone propionate or salmeterol in your body. This can increase your risk of experiencing side effects with Seretide, including irregular heart beats, or may make side effects worse.
• Corticosteroids (by mouth or by injection). If you have had these medicines recently, this might increase the risk of this medicine affecting your adrenal gland.
• Diuretics, also known as 'water tablets' used to treat high blood pressure.
• Other bronchodilators (such as salbutamol).
• Xanthine medicines. These are often used to treat asthma.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
Seretide is not likely to affect your ability to drive or use machines.
Important information about some of the ingredients of Seretide
Seretide Accuhaler contains up to 12.5 milligrams of lactose in each dose. The amount of lactose in this medicine does not normally cause problems in people who are lactose intolerant.
3. How to use Seretide
Always use this medicine exactly as your doctor or pharmacist has told
you. Check with your doctor or pharmacist if you are not sure.
• Use your Seretide every day until your doctor advises you to stop. Do not take more than the recommended dose. Check with your doctor or pharmacist if you are not sure.
• Do not stop taking Seretide or reduce the dose of Seretide without talking to your doctor first.
• Seretide should be inhaled through the mouth into the lungs.
For asthma
Adults and adolescents aged 12 years and over
• Seretide 100 Accuhaler - One inhalation twice a day
• Seretide 250 Accuhaler - One inhalation twice a day
• Seretide 500 Accuhaler - One inhalation twice a day
Children 4 to 12 years of age
• Seretide 100 Accuhaler - One inhalation twice a day
• Seretide is not recommended for use in children below 4 years of age.
For adults with Chronic Obstructive Pulmonary Disease (COPD)
• Seretide 500 Accuhaler - One inhalation twice a day
Your symptoms may become well controlled using Seretide twice a day. If so, your doctor may decide to reduce your dose to once a day. The dose may change to:
• once at night - if you have night-time symptoms
• once in the morning - if you have daytime symptoms.
It is very important to follow your doctor's instructions on how many inhalations to take and how often to take your medicine.
If you are using Seretide for asthma, your doctor will want to regularly check your symptoms.
If your asthma or breathing gets worse tell your doctor straight away. You may find that you feel more wheezy, your chest feels tight more often or you may need to use more of your fast-acting 'reliever' medicine. If any of these happen, you should continue to take Seretide but do not increase the number of puffs you take. Your chest condition may be getting worse and you could become seriously ill. See your doctor as you may need additional treatment.
Instructions for use
• Your doctor, nurse or pharmacist should show you how to use your inhaler. They should check how you use it from time to time. Not using the Seretide Accuhaler properly or as prescribed may mean that it will not help your asthma or COPD as it should.
• The Accuhaler device holds blisters containing Seretide as a powder.
• There is a counter on top of the Accuhaler which tells you how many doses are left. It counts down to 0. The numbers 5 to 0 will appear in red to warn you when there are only a few doses left. Once the counter shows 0, your inhaler is empty.
Using your inhaler
1. To open your Accuhaler, hold the outer case in one hand and put the thumb of your other hand on the thumbgrip. Push your thumb away from you as far as it will go. You will hear a click. This will open a small hole in the mouthpiece.
2. Hold your Accuhaler with the mouthpiece towards you. You can hold it in either your right or left hand. Slide the lever away from you as far as it will go. You will hear a click. This places a dose of your medicine in the mouthpiece.
Every time the lever is pulled back a blister is opened inside and the powder made ready for you to inhale. Do not play with the lever as this opens the blisters and wastes medicine.
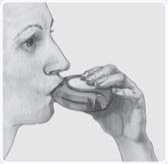
3. Hold the Accuhaler away from your mouth, breathe out as far as is comfortable. Do not breathe into your Accuhaler.
4. Put the mouthpiece to your lips; breathe in steadily and deeply through the Accuhaler, not through your nose.
Remove the Accuhaler from your mouth.
Hold your breath for about 10 seconds or for as long as is comfortable.
Breathe out slowly.
5. Afterwards, rinse your mouth with water and spit it out, and/or brush your teeth.
This may help to stop you getting thrush and becoming hoarse.
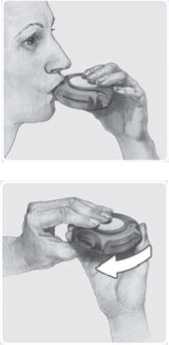
6. To close the Accuhaler, slide the thumbgrip back towards you, as far as it will go. You will hear a click.
The lever will return to its original position and is reset.
Your Accuhaler is now ready for you to use again.
As with all inhalers, caregivers should ensure that children prescribed Seretide Accuhaler use correct inhalation technique, as described above.
Cleaning your inhaler
Wipe the mouthpiece of the Accuhaler with a dry tissue to clean it.



4. Possible side effects

If you use more Seretide than you should
It is important to use the inhaler as instructed. If you accidentally take a larger dose than recommended, talk to your doctor or pharmacist. You may notice your heart beating faster than usual and that you feel shaky. You may also have dizziness, a headache, muscle weakness and aching joints.
If you have used larger doses for a long period of time, you should talk to your doctor or pharmacist for advice. This is because larger doses of Seretide may reduce the amount of steroid hormones produced by the adrenal gland.
If you forget to use Seretide
Do not take a double dose to make up for a missed dose. Just take your next dose at the usual time.
If you stop using Seretide
It is very important that you take your Seretide every day as directed. Keep taking it until your doctor tells you to stop. Do not stop or suddenly reduce your dose of Seretide. This could make your breathing worse.
In addition, if you suddenly stop taking Seretide or reduce your dose of Seretide this may (very rarely) cause you to have problems with your adrenal gland (adrenal insufficiency) which sometimes causes side effects.
These side effects may include any of the following:
• Stomach pain
• Tiredness and loss of appetite, feeling sick
• Sickness and diarrhoea
• Weight loss
• Headache or drowsiness
• Low levels of sugar in your blood
• Low blood pressure and seizures (fits)
When your body is under stress such as from fever, trauma (such as a car accident), infection, or surgery, adrenal insufficiency can get worse and you may have any of the side effects listed above.
If you get any side effects, talk to your doctor or pharmacist. To prevent these symptoms occurring, your doctor may prescribe extra corticosteroids in tablet form (such as prednisolone).
If you have any further questions about the use of this medicine, ask your doctor, nurse or pharmacist.
Like all medicines, this medicine can cause side effects, although not everybody gets them. To reduce the chance of side effects, your doctor will prescribe the lowest dose of Seretide to control your asthma or COPD.
- Thinning of the bones
- Glaucoma
- Weight gain
- Rounded (moon shaped) face (Cushing's Syndrome)
Your doctor will check you regularly for any of these side effects and make sure you are taking the lowest dose of Seretide to control your asthma.
• Behavioural changes, such as being unusually active and irritable (these effects mainly occur in children).
• Uneven heart beat or heart gives an extra beat (arrhythmias). Tell your doctor, but do not stop taking Seretide unless the doctor tells you to stop.
Frequency not known, but may also occur:
• Depression or aggression. These effects are more likely to occur in children.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Seretide
• Keep out of the sight and reach of children.
• Do not store above 30°C.
• Do not use Seretide after the expiry date which is stated on the label and carton. The expiry date refers to the last day of that month.
• Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. Further information
What Seretide contains
• The active substances are 50 micrograms salmeterol xinafoate and 250 micrograms fluticasone propionate.
• The other ingredient is lactose monohydrate (which contains milk proteins).
What Seretide looks like and contents of the pack
• Seretide is a two-tone purple circular device in moulded plastic, with a dose counter indicating the number of doses remaining. Seretide Accuhaler contains a foil strip with 60 blisters. The foil blisters protect the powder from the effects of the atmosphere.
• Each dose is pre-dispensed.
• The devices are packed in cartons which hold: 1 Accuhaler containing 60 inhalations.
Manufacturer
Glaxo Wellcome Production, Evreux, France.
POM
01/12/2014

Allergic reactions: you may notice your breathing suddenly gets worse immediately after using Seretide. You may be very wheezy and cough or be short of breath. You may also notice itching, a rash (hives) and swelling (usually of the face, lips, tongue, or throat), or you may suddenly feel your heart beating very fast or you feel faint and light headed (which may lead to collapse or loss of consciousness). If you get any of these effects or if they happen suddenly after using Seretide, stop using Seretide and tell your doctor straight away. Allergic reactions to Seretide are uncommon (they affect less than 1 person in 100).
Procured from within the EU.
Parallel Import Product Licence holder:
G Pharma Ltd., Salford M50 2PU.
PL 16369/1096 Seretide 250 Accuhaler
Seretide® and Accuhaler® are registered trademarks of the GlaxoSmithKline group of companies
Other side effects are listed below:
Very Common (affects more than 1 person in 10)
• Headache - this usually gets better as treatment continues.
• Increased number of colds have been reported in patients with COPD.
Common (affects less than 1 person in 10)
• Thrush (sore, creamy-yellow, raised patches) in the mouth and throat. Also sore tongue and hoarse voice and throat irritation. Rinsing your mouth out with water and spitting it out immediately and/or brushing your teeth after taking each dose of your medicine may help. Your doctor may prescribe an anti-fungal medication to treat the thrush.
• Aching, swollen joints and muscle pain.
• Muscle cramps.
The following side effects have also been reported in patients with
Chronic Obstructive Pulmonary Disease (COPD):
• Pneumonia and bronchitis (lung infection). Tell your doctor if you notice any of the following symptoms: increase in sputum production, change in sputum colour, fever, chills, increased cough, increased breathing problems.
• Bruising and fractures.
• Inflammation of sinuses (a feeling of tension or fullness in the nose, cheeks and behind the eyes, sometimes with a throbbing ache).
• A reduction in the amount of potassium in the blood (you may get an uneven heart beat, muscle weakness, cramp).
Uncommon (affects less than 1 person in 100)
• Increases in the amount of sugar (glucose) in your blood (hyperglycaemia). If you have diabetes, more frequent blood sugar monitoring and possibly adjustment of your usual diabetic treatment may be required.
• Cataract (cloudy lens in the eye).
• Very fast heart beat (tachycardia).
• Feeling shaky (tremor) and fast or uneven heart beat (palpitations) -these are usually harmless and get less as treatment continues.
• Chest pain.
• Feeling worried (this effect mainly occurs in children).
• Disturbed sleep.
• Allergic skin rash.
Rare (affects less than 1 person in 1000)
• Breathing difficulties or wheezing that get worse straight after taking Seretide. If this happens stop using your Seretide inhaler.
Use your fast-acting 'reliever' inhaler to help your breathing and tell your doctor straight away.
• Seretide may affect the normal production of steroid hormones in the body, particularly if you have taken high doses for long periods of time. The effects include:
- Slowing of growth in children and adolescents

PACKAGE LEAFLET: ^ INFORMATION FOR THE USER ALIFLUS ® 250 ACCUHALER®
(salmeterol xinafoate / fluticasone propionate)
The name of your medicine is Aliflus 250 Accuhaler but throughout the remainder of this leaflet it will be referred to as Aliflus.
This product is available in multiple strengths and all strengths will be referred to throughout this leaflet.
Outer Case
Mouthpiece

Lever
Counter Full Empty
(60 (0
Thumbgrip
Read all of this leaflet carefully before you start taking this
medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms and signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist . This includes any possible side effects not listed in this leaflet. See section 4.
In this leaflet:
1. What Aliflus is and what it is used for
2. What you need to know before you use Aliflus
3. How to use Aliflus
4. Possible side effects
5. How to store Aliflus
6. Contents of the pack and other information
1. What Aliflus is and what it is used for
Aliflus contains two medicines, salmeterol and fluticasone propionate:
• Salmeterol is a long-acting bronchodilator. Bronchodilators help the airways in the lungs to stay open. This makes it easier for air to get in and out. The effects last for at least 12 hours.
• Fluticasone propionate is a corticosteroid which reduces swelling and irritation in the lungs.
The doctor has prescribed this medicine to help prevent breathing
problems such as:
• Asthma
• Chronic Obstructive Pulmonary Disease (COPD). Aliflus Accuhaler, at a dose of 50/500 micrograms, reduces the number of flare ups of COPD symptoms.
You must use Aliflus every day as directed by your doctor. This will make sure that it works properly in controlling your asthma or COPD.
Aliflus helps to stop breathlessness and wheeziness coming on. However Aliflus should not be used to relieve a sudden attack of breathlessness or wheezing. If this happens you need to use a fast -acting ‘reliever' (‘rescue') inhaler, such as salbutamol. You should always have your fast-acting ‘rescue' inhaler with you.
2. What you need to know before you use Aliflus
Do not take Aliflus if:
You are allergic (hypersensitive) to salmeterol, fluticasone propionate or to the other ingredient lactose monohydrate.
Warnings and precautions
Your doctor will supervise your treatment more closely if you have medical conditions such as:
• Heart disease, including an irregular or fast heart beat
• Overactive thyroid gland
• High blood pressure
• Diabetes mellitus (Aliflus may increase your blood sugar)
• Low potassium in your blood
• Tuberculosis (TB) now or in the past, or other lung infections
If you have ever had any of these conditions, tell your doctor before you use Aliflus.
Other medicines and Aliflus
Tell your doctor or pharmacist if you are taking or have recently taken any other medicines. This includes medicines for asthma or any medicines obtained without a prescription. This is because Aliflus may not be suitable to be taken with some other medicines.
Tell your doctor if you are taking the following medicines, before starting
to use Aliflus:
• p blockers (such as atenolol, propranolol and sotalol). p blockers are mostly used for high blood pressure or other heart conditions.
• Medicines to treat infections (such as ritonavir, ketoconazole, itraconazole and erythromycin). Some of these medicines may increase the amount of fluticasone propionate or salmeterol in your body. This can increase your risk of experiencing side effects with Aliflus, including irregular heart beats, or may make side effects worse.
• Corticosteroids (by mouth or by injection). If you have had these medicines recently, this might increase the risk of this medicine affecting your adrenal gland.
• Diuretics, also known as 'water tablets' used to treat high blood pressure.
• Other bronchodilators (such as salbutamol).
• Xanthine medicines. These are often used to treat asthma.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
Aliflus is not likely to affect your ability to drive or use machines.
Important information about some of the ingredients of Aliflus
Aliflus Accuhaler contains up to 12.5 milligrams of lactose in each dose. The amount of lactose in this medicine does not normally cause problems in people who are lactose intolerant.
3. How to use Aliflus
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
• Use your Aliflus every day until your doctor advises you to stop. Do not take more than the recommended dose. Check with your doctor or pharmacist if you are not sure.
• Do not stop taking Aliflus or reduce the dose of Aliflus without talking to your doctor first.
• Aliflus should be inhaled through the mouth into the lungs.
For asthma
Adults and adolescents aged 12 years and over
• Aliflus 100 Accuhaler - One inhalation twice a day
• Aliflus 250 Accuhaler - One inhalation twice a day
• Aliflus 500 Accuhaler - One inhalation twice a day
Children 4 to 12 years of age
• Aliflus 100 Accuhaler - One inhalation twice a day
• Aliflus is not recommended for use in children below 4 years of age.
For adults with Chronic Obstructive Pulmonary Disease (COPD)
• Aliflus 500 Accuhaler - One inhalation twice a day
Your symptoms may become well controlled using Aliflus twice a day. If so, your doctor may decide to reduce your dose to once a day. The dose may change to:
• once at night - if you have night-time symptoms
• once in the morning - if you have daytime symptoms.
It is very important to follow your doctor's instructions on how many inhalations to take and how often to take your medicine.
If you are using Aliflus for asthma, your doctor will want to regularly check your symptoms.
If your asthma or breathing gets worse tell your doctor straight away. You may find that you feel more wheezy, your chest feels tight more often or you may need to use more of your fast-acting 'reliever' medicine. If any of these happen, you should continue to take Aliflus but do not increase the number of puffs you take. Your chest condition may be getting worse and you could become seriously ill. See your doctor as you may need additional treatment.
Instructions for use
• Your doctor, nurse or pharmacist should show you how to use your inhaler. They should check how you use it from time to time. Not using the Aliflus Accuhaler properly or as prescribed may mean that it will not help your asthma or COPD as it should.
• The Accuhaler device holds blisters containing Aliflus as a powder.
• There is a counter on top of the Accuhaler which tells you how many doses are left. It counts down to 0. The numbers 5 to 0 will appear in red to warn you when there are only a few doses left. Once the counter shows 0, your inhaler is empty.
Using your inhaler
1. To open your Accuhaler, hold the outer case in one hand and put the thumb of your other hand on the thumbgrip. Push your thumb away from you as far as it will go. You will hear a click. This will open a small hole in the mouthpiece.
2. Hold your Accuhaler with the mouthpiece towards you. You can hold it in either your right or left hand. Slide the lever away from you as far as it will go. You will hear a click. This places a dose of your medicine in the mouthpiece.
Every time the lever is pulled back a blister is opened inside and the powder made ready for you to inhale. Do not play with the lever as this opens the blisters and wastes medicine.
3. Hold the Accuhaler away from your mouth, breathe out as far as is comfortable. Do not breathe into your Accuhaler.
4. Put the mouthpiece to your lips; breathe in steadily and deeply through the Accuhaler, not through your nose.
Remove the Accuhaler from your mouth.
Hold your breath for about 10 seconds or for as long as is comfortable.
Breathe out slowly.
5. Afterwards, rinse your mouth with water and spit it out, and/or brush your teeth.
This may help to stop you getting thrush and becoming hoarse.
6. To close the Accuhaler, slide the thumbgrip back towards you, as far as it will go. You will hear a click.
The lever will return to its original position
and is reset.
Your Accuhaler is now ready for you to use again.
As with all inhalers, caregivers should ensure that children prescribed Aliflus Accuhaler use correct inhalation technique, as described above.
Cleaning your inhaler
Wipe the mouthpiece of the Accuhaler with a dry tissue to clean it.



If you use more Aliflus than you should
It is important to use the inhaler as instructed. If you accidentally take a larger dose than recommended, talk to your doctor or pharmacist. You may notice your heart beating faster than usual and that you feel shaky. You may also have dizziness, a headache, muscle weakness and aching joints.
If you have used larger doses for a long period of time, you should talk to your doctor or pharmacist for advice. This is because larger doses of Aliflus may reduce the amount of steroid hormones produced by the adrenal gland.
If you forget to use Aliflus
Do not take a double dose to make up for a missed dose. Just take your next dose at the usual time.
- Glaucoma
- Weight gain
- Rounded (moon shaped) face (Cushing's Syndrome)
Your doctor will check you regularly for any of these side effects and make sure you are taking the lowest dose of Aliflus to control your asthma.
• Behavioural changes, such as being unusually active and irritable (these effects mainly occur in children).
• Uneven heart beat or heart gives an extra beat (arrhythmias). Tell your doctor, but do not stop taking Aliflus unless the doctor tells you to stop.
Frequency not known, but may also occur:
• Depression or aggression. These effects are more likely to occur in children.
4. Possible side effects

If you stop using Aliflus
It is very important that you take your Aliflus every day as directed. Keep taking it until your doctor tells you to stop. Do not stop or suddenly reduce your dose of Aliflus. This could make your breathing worse.
In addition, if you suddenly stop taking Aliflus or reduce your dose of Aliflus this may (very rarely) cause you to have problems with your adrenal gland (adrenal insufficiency) which sometimes causes side effects.
These side effects may include any of the following:
• Stomach pain
• Tiredness and loss of appetite, feeling sick
• Sickness and diarrhoea
• Weight loss
• Headache or drowsiness
• Low levels of sugar in your blood
• Low blood pressure and seizures (fits)
When your body is under stress such as from fever, trauma (such as a car accident), infection, or surgery, adrenal insufficiency can get worse and you may have any of the side effects listed above.
If you get any side effects, talk to your doctor or pharmacist. To prevent these symptoms occurring, your doctor may prescribe extra corticosteroids in tablet form (such as prednisolone).
If you have any further questions about the use of this medicine, ask your doctor, nurse or pharmacist.
Like all medicines, this medicine can cause side effects, although not everybody gets them. To reduce the chance of side effects, your doctor will prescribe the lowest dose of Aliflus to control your asthma or COPD.
Allergic reactions: you may notice your breathing suddenly gets worse immediately after using Aliflus. You may be very wheezy and cough or be short of breath. You may also notice itching, a rash (hives) and swelling (usually of the face, lips, tongue, or throat), or you may suddenly feel your heart beating very fast or you feel faint and light headed (which may lead to collapse or loss of consciousness). If you get any of these effects or if they happen suddenly after using Aliflus, stop using Aliflus and tell your doctor straight away. Allergic reactions to Aliflus are uncommon (they affect less than 1 person in 100).
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Aliflus
• Keep out of the sight and reach of children.
• Do not store above 30°C.
• Do not use Aliflus after the expiry date which is stated on the label and carton. The expiry date refers to the last day of that month.
• Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment
6. Further information
What Aliflus contains
• The active substances are 50 micrograms salmeterol xinafoate and 250 micrograms fluticasone propionate.
• The other ingredient is lactose monohydrate (which contains milk proteins).
What Aliflus looks like and contents of the pack
• Aliflus is a two-tone purple circular device in moulded plastic, with a dose counter indicating the number of doses remaining. Aliflus Accuhaler contains a foil strip with 60 blisters. The foil blisters protect the powder from the effects of the atmosphere.
• Each dose is pre-dispensed.
• The devices are packed in cartons which hold: 1 Accuhaler containing 60 inhalations.
Manufacturer
Glaxo Wellcome Production, Evreux, France.
Procured from within the EU.
Parallel Import Product Licence holder: G Pharma Ltd., Salford M50 2PU.
PL 16369/1096 Aliflus 250 Accuhaler
01/12/2014
Aliflus® and Accuhaler® are registered trademarks of the GlaxoSmithKline group of companies

Other side effects are listed below:
Very Common (affects more than 1 person in 10)
• Headache - this usually gets better as treatment continues.
• Increased number of colds have been reported in patients with COPD.
Common (affects less than 1 person in 10)
• Thrush (sore, creamy-yellow, raised patches) in the mouth and throat. Also sore tongue and hoarse voice and throat irritation. Rinsing your mouth out with water and spitting it out immediately and/or brushing your teeth after taking each dose of your medicine may help. Your doctor may prescribe an anti-fungal medication to treat the thrush.
• Aching, swollen joints and muscle pain.
• Muscle cramps.
The following side effects have also been reported in patients with
Chronic Obstructive Pulmonary Disease (COPD):
• Pneumonia and bronchitis (lung infection). Tell your doctor if you notice any of the following symptoms: increase in sputum production, change in sputum colour, fever, chills, increased cough, increased breathing problems.
• Bruising and fractures.
• Inflammation of sinuses (a feeling of tension or fullness in the nose, cheeks and behind the eyes, sometimes with a throbbing ache).
• A reduction in the amount of potassium in the blood (you may get an uneven heart beat, muscle weakness, cramp).
Uncommon (affects less than 1 person in 100)
• Increases in the amount of sugar (glucose) in your blood (hyperglycaemia). If you have diabetes, more frequent blood sugar monitoring and possibly adjustment of your usual diabetic treatment may be required.
• Cataract (cloudy lens in the eye).
• Very fast heart beat (tachycardia).
• Feeling shaky (tremor) and fast or uneven heart beat (palpitations) -these are usually harmless and get less as treatment continues.
• Chest pain.
• Feeling worried (this effect mainly occurs in children).
• Disturbed sleep.
• Allergic skin rash.
Rare (affects less than 1 person in 1000)
• Breathing difficulties or wheezing that get worse straight after taking Aliflus. If this happens stop using your Aliflus inhaler.
Use your fast-acting 'reliever' inhaler to help your breathing and tell your doctor straight away.
• Aliflus may affect the normal production of steroid hormones in the body, particularly if you have taken high doses for long periods of time. The effects include:
- Slowing of growth in children and adolescents
- Thinning of the bones