Amitriptyline 10Mg Tablets
Out of date information, search another|
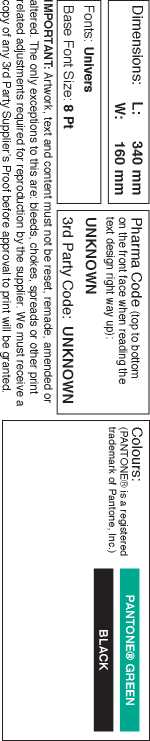
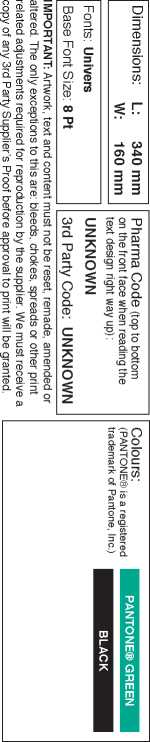
Ref: 231-30-72912-X LEA AMITRIPTYLINE A/S TAB TUK <DEB Version: 1 22 October 2012 | |
|
PL Number(s), PL 00289/0178-0180. TEVA UK Limited Licence (Responsible Regulatory Officer = TEVA Post Licence Team), MA Holder & Packer: Packed at Debrecen, Hungary. | |
|
TEVA UK LIMITED | |
|
Reason for revision: Version 1: Leaflet text updates. TEVA Post Licence Team. 09/10/12 18:46 (Trackwise: 153517). | |
3
AMITRIPTYLINE 10 mg, 25 mg AND 50 mg TABLETS
PACKAGE LEAFLET: INFORMATION FOR THE USER
Read all of this leaflet carefully before you start
taking this medicine.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
IN THIS LEAFLET:
1. What Amitriptyline is and what it is used for
2. Before you take Amitriptyline
3. How to take Amitriptyline
4. Possible side effects
5. How to store Amitriptyline
6. Further information
OWHAT AMITRIPTYLINE IS AND WHAT IT IS USED FOR
• Amitriptyline belongs to a group of drugs called tricyclic antidepressants
• Amitriptyline is used to treat depression.
BEFORE YOU TAKE AMITRIPTYLINE
DO NOT take Amitriptyline if you:
• are allergic (hypersensitive) to amitriptyline or any of the other ingredients of this medicine
• are taking monoamine oxidase inhibitors (MAOIs), or have stopped taking these medicines within the last 14 days
• have any heart problems e.g. you are recovering from a heart attack or you have an abnormal heart rhythm
• have severe liver disease
• are pregnant or breast-feeding
• suffer from mania (a mood disorder characterised by high levels of excitement and activity)
• are under 16 years (see section 3, How to take Amitriptyline).
Take special care with Amitriptyline Thoughts of suicide and worsening of your depression or anxiety disorder
If you are depressed and/or have anxiety disorders you can sometimes have thoughts of harming or killing yourself. These may be increased when first starting antidepressants, since these medicines all take time to work, usually about two weeks but sometimes longer.
You may be more likely to think like this:
• if you have previously had thoughts about killing or harming yourself
• if you are a young adult. Information from clinical trials has shown an increased risk of suicidal behaviour in adults aged less than 25 years with psychiatric conditions who were treated with an antidepressant.
If you have thoughts of harming or killing yourself at any time, contact your doctor or go to a hospital straight away.
You may find it helpful to tell a relative or close friend that you are depressed or have an anxiety disorder, and ask them to read this leaflet. You might ask them to tell you if they think your depression or anxiety is getting worse, or if they are worried about changes in your behaviour.
Tell your doctor before you start to take this
medicine if you:
• suffer from epileptic fits
• have any blood disorders (you may bruise easily, frequently suffer from infections or be anaemic)
• have schizophrenia or manic-depression
• suffer from porphyria (a deficiency of specific enzymes within the body, causing an increase of substances called porphyrins)
• have phaeochromocytoma (an adrenal gland tumour)
• have prostate trouble
• have liver problems
• suffer from narrow angle glaucoma (loss of vision due to abnormally high pressure in the eye)
• have kidney problems e.g. difficulty passing water
• have thyroid disease
• are being given electroconvulsive therapy (ECT)
• are planning to have surgery, as Amitriptyline may need to be stopped before you have a general anaesthetic.
If you are elderly, you are more likely to suffer from certain side effects (see section 4, Possible side effects).
You may not see an improvement in your depression during the first month of treatment. Your doctor may want to monitor you during this time.
Taking other medicines
DO NOT take Amitriptyline in combination with, or if you have taken in the last 14 days
• antidepressants known as MAOIs e.g. moclobemide or phenelzine.
Talk to your doctor if you are taking any of the following:
• antidepressants or drugs to treat other mental illnesses, e.g. pimozide, fluoxetine or clozapine
• sedatives e.g. diazepam
• anticholinergics e.g. atropine or hyoscine
• antiepileptics used to treat epilepsy such as carbamazepine, barbiturates e.g. amobarbital or phenobarbital
• methylphenidate (used to treat hyperactivity)
• apraclonidine and brimonidine (used to treat glaucoma)
• sympathomimetic drugs e.g. adrenaline, ephedrine, isoprenaline, noradrenaline, phenylephrine or phenylpropanolamine. These may be present in many medicines for colds and nasal stuffiness. Tell your pharmacist that you are taking Amitriptyline before buying such products
• blood pressure drugs e.g. guanethidine, debrisoquine, betanidine, clonidine, and verapamil or diltiazem (used to treat chest pain, high blood pressure or an irregular heart beat)
• drugs used to treat an irregular heartbeat e.g. amiodarone, disopyramide, procainamide, propafenone, quinidine, sotalol
• diuretics ("water tablets") e.g. amiloride, bendroflumethiazide or triamterene
• sublingual nitrates (tablets placed under the tongue to treat chest pain)
• disulfiram (used to treat alcoholism)
• cimetidine (used to reduce acid indigestion)
• altretamine (used to treat cancer of the ovary)
• nefopam or tramadol (painkillers)
• selegiline and entacapone (used to treat Parkinson's disease)
• levacetylmethadol (used to treat drug dependence)
• rifampicin (used to treat infections)
• Sibutramine (anti-obesity drug)
• baclofen (used to relieve spasms, cramping and muscle rigidity)
• antihistamines such as cetirizine, loratadine or terfenadine
• oral contraceptives (the pill)
• thyroid hormones e.g. levothyroxine
• electroconvulsive therapy (ECT)
• ritonavir (used to treat HIV infection).
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
Important information about some of the ingredients of Amitriptyline
• Patients who are intolerant to lactose should note that Amitriptyline Tablets contain a small amount of lactose. If your doctor has told you that you have an intolerance to some sugars, contact your doctor before taking this medicine.
• The 25 mg tablets contain sunset yellow (E110), which can cause an allergic-type reaction, including asthma. This reaction is more common in those people who are allergic to aspirin.
Taking Amitriptyline with food and drink
• DO NOT drink alcohol while taking this medicine as it may increase the sedative effects of these tablets.
Pregnancy and breast-feeding
• Amitriptyline tablets should not be taken in the first three months and the last three months of pregnancy. If taken in the last three months, the newborn may have withdrawal symptoms
• Amitriptyline is not recommended if you are breast-feeding
• If you are pregnant or planning to become pregnant, ask your doctor or pharmacist for advice before taking any medicine.
Driving and using machines
• Amitriptyline may cause drowsiness, if affected do not drive or operate machinery.
HOW TO TAKE AMITRIPTYLINE
Always take Amitriptyline exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
If you see another doctor or go into hospital, let them or the staff know what medicines you are taking.
The tablets should be swallowed preferably with a glass of water. The usual dose is:
|
Ref: 231-30-72912-X LEA AMITRIPTYLINE A/S TAB TUK <DEB Version: 1 22 October 2012 | |
|
lirJ=l,/il | |
|
PL Number(s), PL 00289/0178-0180. TEVA UK Limited Licence (Responsible Regulatory Officer = TEVA Post Licence Team), MA Holder & Packer: Packed at Debrecen, Hungary. | |
|
TEVA UK LIMITED | |
|
Reason for revision: Version 1: Leaflet text updates. TEVA Post Licence Team. 09/10/12 18:46 (Trackwise: 153517). | |
• Children and adolescents
Not recommended for children and adolescents under 16 years.
• Adults:
The usual starting dose is 75 mg a day in divided doses or as a single dose at night. This may then be gradually increased if necessary, with any extra doses taken in the late afternoon and/or at bedtime.
The maintenance dose is usually 50-100 mg a day given as a single dose preferably in the evening or at bedtime.
• Elderly:
The usual dose is 10-25 mg three times a day initially, which may be gradually increased if necessary. The dosage may be taken as divided doses, or as a single dose, preferably in the evening or at bedtime.
You may not notice any improvement in your condition for up to 4 weeks after starting your treatment.
If you take more Amitriptyline than you should
If you (or someone else) swallow a lot of the tablets all together, or if you think a child has swallowed any of the tablets, contact your nearest hospital casualty department or your doctor immediately.
An overdose is likely to cause heart rate irregularities, hot dry skin, dry mouth and tongue, dilated pupils, squint, problems passing water, difficulty in controlling movements, involuntary eye movement, drowsiness, low blood pressure, vomiting, agitation, muscle rigidity, fever, low body temperature, fits, breathing problems and possibly coma.
Please take this leaflet, any remaining tablets, and the container with you to the hospital or doctor so that they know which tablets were consumed.
If you forget to take Amitriptyline
If you forget to take a tablet, take one as soon as you remember, unless it is nearly time to take the next one. DO NOT take a double dose to make up for a forgotten dose. Take the remaining doses at the correct time.
If you stop taking Amitriptyline
DO NOT stop taking these tablets suddenly. You should continue to take the tablets for as long as your doctor tells you to.
Withdrawal symptoms which may occur if you stop taking the tablets suddenly include feeling sick, headache and generally feeling unwell. Gradual withdrawal is associated with reports of symptoms including irritability, restlessness, excitement, and hyperactivity, as well as dream and sleep disturbances during the first two weeks of dosage reduction. Feeling elated or over-excited has been rarely reported when stopping long term treatment with this type of drug. These symptoms are transient and are not a sign of addiction.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
POSSIBLE SIDE EFFECTS
Like all medicines, Amitriptyline can cause side effects, although not everybody gets them.
If the following happens, stop taking the tablets and tell your doctor immediately or go to the casualty department at your nearest hospital:
• an allergic reaction (swelling of the lips, face or neck leading to severe difficulty in breathing; skin rash or hives).
This is a very serious but rare side effect. You may need urgent medical attention or hospitalisation.
The following effects have been reported with this type of drug, although not particularly with amitriptyline:
• Effects on the blood:
Blood disorders which may be characterised by fever or chills, sore throat, ulcers in your mouth or throat, unusual tiredness or weakness, unusual bleeding or unexplained bruising. Tell your doctor immediately if you notice any of these symptoms.
• Effects on the heart:
High or low blood pressure, changes in heart rhythm, heart attack, stroke.
• Effects on brain and central nervous system: Tiredness, headache, weakness, confusion, disturbed concentration, disorientation, delusions, hallucinations, elevated mood and hyperactivity, excitement, anxiety, restlessness, drowsiness, dream and sleep disturbances, numbness, pins and needles, loss of co-ordination, uncontrolled shaking, abnormal muscle movements, slurred speech, coma, and fits.
• Effects on the Ear:
Ringing in the ears.
• Effects on the anti-cholinergic system:
Dry mouth, blurred vision, eye problems, increased pressure in the eye, constipation, bowel problems, problems passing urine, increased urine production, high body temperature.
• Allergic reactions:
Swelling of the face and tongue.
• Effects on the digestive system:
Nausea (feeling sick), stomach discomfort, vomiting, loss of appetite, diarrhoea, abdominal pains, an unpleasant taste, black tongue, swelling of the area around the ear, soreness of the mouth.
• Effects on liver:
Rarely hepatitis (inflammation of the liver), jaundice characterised by yellowing of the skin and whites of the eyes.
• Effects on the hormone system:
Inappropriate secretion of the antidiuretic hormone.
• Effects on the reproductive system and breast-feeding:
Testicular swelling, breast enlargement in both men and women, milk production by women even if they are not breast-feeding, and sexual problems.
Other adverse effects include, changes in blood sugar levels and low blood sodium levels, dizziness, weakness, fatigue, headache, fluid retention, needing to pass water often, increased perspiration, hair loss, increased appetite, and weight gain (may be due to the drug or as a result of the relief of depression).
An increased risk of bone fractures has been observed in patients taking this type of medicines.
There have also been reports of breathing problems and agitation in babies whose mothers took this type of drug.
If you are elderly, you are more likely to experience effects of agitation, confusion, low blood pressure on standing causing dizziness, light-headedness or fainting, or to develop low blood levels of sodium, which can cause tiredness, confusion, muscle twitching and fits.
If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
HOW TO STORE AMITRIPTYLINE
Keep out of the reach and sight of children.
The tablets should be stored in the package or container supplied. Do not transfer them to another container.
Do not use Amitriptyline after the expiry date that is stated on the outer packaging. The expiry date refers to the last day of that month.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
FURTHER INFORMATION
What Amitriptyline Tablets contain:
• The active ingredient is amitriptyline hydrochloride
• The other ingredients are lactose monohydrate, maize starch, calcium hydrogen phosphate dihydrate, silica colloidal anhydrous, magnesium stearate, hypromellose (E464), titanium dioxide (E171)
• The 10 mg tablets also contain macrogol, dispersed blue (E131) and brilliant blue (E133); the 25 mg tablets also contain polyethylene glycol, quinoline yellow (E104) and sunset yellow (E110); the 50 mg tablets also contain polyethylene glycol and red iron oxide (E172)
• The tablets are polished with carnauba wax.
What Amitriptyline Tablets look like and contents of
the pack:
• Amitriptyline 10 mg Tablets are sky blue, biconvex, film-coated tablets, engraved "D" on one side and plain on the reverse.
• Amitriptyline 25 mg Tablets are yellow, biconvex, film-coated tablets, engraved "D" on one side and plain on the reverse.
• Amitriptyline 50 mg Tablets are red/brown, biconvex, film-coated tablets, engraved "D" on one side and plain on the reverse.
• All strengths of tablets are available in pack sizes of 7, 10, 14, 21, 28, 30, 56, 60, 84, 90, 100, 110, 112, 120, 150, 160, 168, 500, or 15000 tablets. The 25 mg tablets are also available in a pack size of 25 tablets, and the 50 mg tablets are also available in a pack size of 250 tablets.
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer
Marketing Authorisation holder and company
responsible for manufacture: TEVA UK Limited,
Eastbourne, BN22 9AG.
This leaflet was last revised: August 2012
PL 00289/0178-0180
TEVA UK LIMITED
72912-X