Atrovent 20 Micrograms Cfc-Free Inhaler
Out of date information, search another

Package leaflet: Information for the user
Atrovent® 20 micrograms CFC-Free Inhaler
(ipratropium bromide)
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects gets troublesome or serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
The name of your medicine is Atrovent 20 micrograms CFC-Free
Inhaler but it will be referred to as Atrovent throughout this leaflet.
In this leaflet:
1. What Atrovent is and what it is used for
2. Before you use Atrovent
3. How to use Atrovent
4. Possible side effects
5. How to store Atrovent
6. Further information
1. WHAT ATROVENT IS AND WHAT IT IS USED FOR
Atrovent is an inhaler and contains a medicine called ipratropium bromide. This belongs to a group of medicines called bronchodilators. It is used to make breathing easier for people with asthma or ‘chronic obstructive pulmonary disease' (COPD), often referred to as chronic bronchitis. You may have difficulty breathing, shortness of breath, wheezing or tightness in your chest.
Atrovent works by opening up your airways.
2. BEFORE YOU USE ATROVENT Do not use Atrovent if:
• You are allergic (hypersensitive) to ipratropium or any of the other ingredients in ATROVENT. (Listed in section 6: Further information)
• You are allergic to similar medicines which contain atropine or medicines like atropine
• You are pregnant, think you are pregnant, likely to get pregnant or are breast-feeding
Do not use if any of the above apply to you. If you are not sure, talk to your doctor or pharmacist before using Atrovent.
Take special care with Atrovent
Check with your doctor or pharmacist before using this medicine if:
• You have glaucoma, or have been told that you may develop it
• You have problems passing water (urine)
• You are a man who has prostate problems
• You have cystic fibrosis
If you are not sure if any of these apply to you, talk to your doctor or pharmacist before using Atrovent.
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including any inhalers and medicines obtained without a prescription. This includes herbal medicines. This is because Atrovent can affect the way some other medicines work. Also some other medicines can affect the way Atrovent works.
In particular, tell your doctor or pharmacist if you are taking/ have taken any of the following medicines:
• Other inhalers to help you to breathe more easily such as the reliever inhaler salbutamol
• Medicines called ‘xanthines' to help your breathing such as theophylline and aminophylline
If you are not sure if any of the above apply to you, talk to your doctor or pharmacist before using Atrovent.
Pregnancy and breast-feeding
Do not use Atrovent if you are pregnant, think you are pregnant, likely to get pregnant or are breast-feeding.
Driving and using machines
You may feel dizzy, or have difficulty in focusing, or blurred vision while taking Atrovent. If this happens do not drive or use any tools or machines.
Operations
If you attend a hospital appointment or are admitted to hospital, be sure to take your inhaler(s) and any other medicines (in their packaging if possible) with you. Some gases used in operations (anaesthetic gases) may affect how your inhaler works. If you are about to have surgery, make sure you mention that you are taking Atrovent to the doctor, dentist or anaesthetist.
3. HOW TO USE ATROVENT
Always use Atrovent exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. Follow these instructions to get the best results. If anything is unclear after reading this leaflet, ask your doctor or pharmacist.
You may notice that this CFC-Free inhaler tastes slightly different from the last CFC-containing inhaler you used. This is normal.
The inhaler is still as safe and will work as well as your last one.
How much to use
Adults (including the elderly)
• One or two puffs to be inhaled three or four times daily
• Sometimes, in early treatment, up to four puffs at a time may be taken
Children 6-12 yrs
• One or two puffs to be inhaled three times daily Children under 6 yrs
• One puff to be inhaled three times daily
When children are using this medicine they must be supervised by a responsible adult.
Do not use more than your doctor has told you
See your doctor straight away if:
• You feel that your inhaler is not working as well as usual
• You need to use the inhaler more than your doctor has recommended
Your doctor may need to check how well your medicine is working. In some cases your doctor may need to change your medicine.
Testing Your Inhaler
To make sure that your inhaler is working, test fire it twice into the air before using it for the first time and whenever your inhaler has not been used for 3 days or more.
How to use your inhaler
Read through numbers 1 to 6 first, before starting to use your inhaler.
Remove the cap from the mouthpiece.
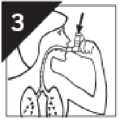
Hold the inhaler as shown in the picture (with the arrow on the label pointing upwards) and breathe out gently.
Then straight away, put the mouthpiece in your mouth.
Hold the mouthpiece with your lips. Start to breathe in slowly and deeply through your mouth.
Press the top of the inhaler firmly. This will release one puff of your medicine. Keep breathing in.
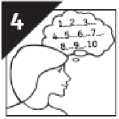
Hold your breath for as long as is comfortable.
If possible hold your breath for 10 seconds.
Then breathe out slowly.
• If you are having more than one puff, wait at least 1 minute before the next puff.
• Then repeat steps 2, 3 and 4.
After use, replace the cap on the mouthpiece.
The mouthpiece has been designed specially for use with this product only. Do not use any other mouthpiece with the product and do not use the mouthpiece provided here with any other product.
If you find breathing in and pressing the inhaler at the same time (step 3) difficult you should talk to your doctor or pharmacist, as you could use a spacer device (Aerochamber Plus™) with your inhaler. A spacer is a device designed to make step 3 easier. A spacer is generally a plastic container with a mouthpiece at one end and a hole for inserting the mouthpiece of the inhaler at the other end.
The puff of medicine from your inhaler is sprayed into the spacer and the puff of medicine stays there, inside the spacer, until you breathe in through your mouth from the spacer with the spacer mouthpiece in your mouth and with your lips closed around it. This means that you do not have to worry about breathing in and pressing the inhaler at the same time.
When using your Atrovent take care not to let any of the spray enter your eyes. If any of the spray accidentally gets into your eyes you may get painful, stinging or red eyes, dilated pupils, blurred vision, see colours or lights. If this happens, talk to your doctor for advice.
If you get problems with your eyes at any other time, talk to your doctor for advice. You may be developing glaucoma, which will need treatment straight away.
Cleaning
It is important to clean your inhaler regularly. Otherwise it may not work properly.
• Remove the canister and cap
• Wash and clean the white mouthpiece in warm soapy water
• Rinse in warm water and allow to air-dry without using any heating system
• Make sure the small hole in the mouthpiece is washed through thoroughly
• Once the white mouthpiece is dry, replace the canister and the cap
Make sure you do not run out of Atrovent
The inhaler has been designed to deliver 200 puffs of your medicine. However, it is not possible to tell when the inhaler is empty and when the 200 puffs have been used. There may still be a small amount of fluid left over in the container. Please make sure that your inhaler is replaced after you have taken 200 puffs (usually after 3-4 weeks of regular use) so that you can be certain that you are getting the right amount of your medicine in each puff.
If you use more Atrovent than you should
If you use more of this inhaler than you should, talk to a doctor or go to a hospital straight away. Take all your inhalers and any other medicines you are taking (in their packaging if possible) with you. If you take too much or too many puffs you may get a dry mouth, a rapid heart rate or blurred vision.
If you forget to take Atrovent
• If you forget a dose, inhale it as soon as you remember it.
• However, if it is time for the next dose, skip the missed dose.
• Do not take a double dose to make up for a forgotten dose.
If you have any further questions, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Atrovent can cause side effects, although not everybody gets them.
Tell your doctor straight away if you notice any the following serious side effects - you may need urgent medical treatment:
• If after taking Atrovent you are wheezy or have other difficulties in breathing, do not take any more (unless you have been told to by your doctor). You may need to take a fast-acting reliever inhaler such as salbutamol to help your breathing. Your doctor may decide that you need different medicines to help your breathing
• Allergic reactions - the signs may include skin rash and itching (affects less than 1 in 100 people). In severe cases the signs include swelling of your mouth and face, sudden difficulties in breathing and reduction of your blood pressure. Tightening of your throat (affects less than 1 in 100 people)
• Palpitations (fast or uneven heart beats) or quickening of the heart rate (affects less than 1 in 100 people)
• Increased heart rate or irregular heart rhythm such as atrial fibrillation (affects less than 1 in 1000 people)
See your doctor straight away if you have any of these side effects.
The side effects described below have been experienced by people taking Atrovent and they are listed as either common, uncommon or rare.
Common (affects less than 1 in 10 people)
• Headache, dizziness
• Dry mouth, feeling sick (nausea), stomach upset or discomfort
• Cough and throat irritation when you have just used Atrovent
Uncommon (affects less than 1 in 100 people)
• Itching, skin rash
• Unexpected tightness of the chest, swelling of the throat, dry throat
• Blurred vision, dilated pupils, glaucoma, painful, stinging, red or swelling of the eyes, see colours or lights
• Diarrhoea, constipation or being sick
• Mouth or lip sores
• Problems passing water (urine), especially if you already have problems passing urine
Rare (affects less than 1 in 1000 people)
• Difficulty focusing
• Nettle rash (urticaria)
If any of the side effects gets troublesome or serious, or if you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
If any of the spray accidentally gets into your eyes you may get painful, stinging or red eyes, dilated pupils, blurred vision, see colours or lights. If this happens, talk to your doctor for advice. If you get problems with your eyes at any other time, talk to your doctor for advice. You may be developing glaucoma, which will need treatment straight away. If your eyes are affected in any way do not drive or operate machinery.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard
By reporting side effects, you can help provide more information on the safety of this medicine.
5. HOW TO STORE ATROVENT
• Keep out of the sight and reach of children
• Do not take your medicine after the expiry date which is stated on the carton and the canister label after ‘Exp'. The expiry date refers to the last day of that month.
• Do not store above 25°C.
• Do not freeze.
• Keep pressurised container away from heat and light.
• Do not expose to temperatures higher than 50°C.
• The canister contains a pressurised liquid. Do not pierce or burn container even when empty.
6. FURTHER INFORMATION What Atrovent contains
The active ingredient is ipratropium bromide.
Each actuation contains 20 micrograms ipratropium bromide (as the monohydrate.)
Other ingredients are HFA-134a (1,1,1,2-tetrafluoroethane), citric acid anhydrous, ethanol anhydrous and purified water.
Atrovent does not contain any chlorofluorocarbon (CFC) propellants.
You may have been prescribed Atrovent inhaler CFC-Free as you were previously being treated with Atrovent inhaler. These products contain the same medicine, ipratropium bromide, but different propellants. Propellants are ingredients which enable the delivery of the medicine to the lungs. Atrovent inhaler contained chlorofluorocarbons or CFCs as propellants which are known to damage the ozone layer. Your Atrovent has been developed to include the new propellant HFA-134a which does not damage the ozone layer i.e. Atrovent does not contain any CFCs. In terms of safety and effectiveness the CFC-Free product is the same as the old CFC-containing product.
What Atrovent looks like and contents of the pack
Atrovent is an inhaler, in which a stainless steel pressurised canister with metering valve and outer clear and white body with a green cap. The canister is filled with a clear, colourless liquid.
Each canister contains 10ml solution (200 actuations).
Each carton contains one inhaler.
Manufactured by: Boehringer Ingelheim Pharma GmbH & Co. KG, Binger Strasse 173, D-55216 Ingelheim/Rhein, Germany.
Procured from within the EU and repackaged by the Product Licence holder: B&S Healthcare, Unit 4, Bradfield Road, Ruislip, Middlesex, HA40NU, UK.
Atrovent® 20 micrograms CFC-Free Inhaler |pqm|
PL No: 18799/2394
Leaflet date: 29.01.2015
Atrovent is a registered trademark of Boehringer Ingelheim.





Package leaflet: Information for the user
Ipratropium bromide 20 micrograms CFC-Free Inhaler
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects gets troublesome or serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
The name of your medicine is Ipratropium bromide 20 micrograms
CFC-Free Inhaler but it will be referred to as Ipratropium throughout
this leaflet.
In this leaflet:
1. What Ipratropium is and what it is used for
2. Before you use Ipratropium
3. How to use Ipratropium
4. Possible side effects
5. How to store Ipratropium
6. Further information
1. WHAT IPRATROPIUM IS AND WHAT IT IS USED FOR
Ipratropium is an inhaler and contains a medicine called ipratropium bromide. This belongs to a group of medicines called bronchodilators. It is used to make breathing easier for people with asthma or ‘chronic obstructive pulmonary disease' (COPD), often referred to as chronic bronchitis. You may have difficulty breathing, shortness of breath, wheezing or tightness in your chest.
Ipratropium works by opening up your airways.
2. BEFORE YOU USE IPRATROPIUM Do not use Ipratropium if:
• You are allergic (hypersensitive) to ipratropium or any of the other ingredients in Ipratropium. (Listed in section 6: Further information)
• You are allergic to similar medicines which contain atropine or medicines like atropine
• You are pregnant, think you are pregnant, likely to get pregnant or are breast-feeding
Do not use if any of the above apply to you. If you are not sure, talk to your doctor or pharmacist before using Ipratropium.
Take special care with Ipratropium
Check with your doctor or pharmacist before using this medicine if:
• You have glaucoma, or have been told that you may develop it
• You have problems passing water (urine)
• You are a man who has prostate problems
• You have cystic fibrosis
If you are not sure if any of these apply to you, talk to your doctor or pharmacist before using Ipratropium.
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including any inhalers and medicines obtained without a prescription. This includes herbal medicines. This is because Ipratropium can affect the way some other medicines work. Also some other medicines can affect the way Ipratropium works.
In particular, tell your doctor or pharmacist if you are taking/ have taken any of the following medicines:
• Other inhalers to help you to breathe more easily such as the reliever inhaler salbutamol
• Medicines called ‘xanthines' to help your breathing such as theophylline and aminophylline
If you are not sure if any of the above apply to you, talk to your doctor or pharmacist before using Ipratropium.
Pregnancy and breast-feeding
Do not use Ipratropium if you are pregnant, think you are pregnant, likely to get pregnant or are breast-feeding.
Driving and using machines
You may feel dizzy, or have difficulty in focusing, or blurred vision while taking Ipratropium. If this happens do not drive or use any tools or machines.
Operations
If you attend a hospital appointment or are admitted to hospital, be sure to take your inhaler(s) and any other medicines (in their packaging if possible) with you. Some gases used in operations (anaesthetic gases) may affect how your inhaler works. If you are about to have surgery, make sure you mention that you are taking Ipratropium to the doctor, dentist or anaesthetist.
3. HOW TO USE IPRATROPIUM
Always use Ipratropium exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. Follow these instructions to get the best results. If anything is unclear after reading this leaflet, ask your doctor or pharmacist.
You may notice that this CFC-Free inhaler tastes slightly different from the last CFC-containing inhaler you used. This is normal.
The inhaler is still as safe and will work as well as your last one.
How much to use
Adults (including the elderly)
• One or two puffs to be inhaled three or four times daily
• Sometimes, in early treatment, up to four puffs at a time may be taken
Children 6-12 yrs
• One or two puffs to be inhaled three times daily Children under 6 yrs
• One puff to be inhaled three times daily
When children are using this medicine they must be supervised by a responsible adult.
Do not use more than your doctor has told you
See your doctor straight away if:
• You feel that your inhaler is not working as well as usual
• You need to use the inhaler more than your doctor has recommended
Your doctor may need to check how well your medicine is working. In some cases your doctor may need to change your medicine.
Testing Your Inhaler
To make sure that your inhaler is working, test fire it twice into the air before using it for the first time and whenever your inhaler has not been used for 3 days or more.
How to use your inhaler
Read through numbers 1 to 6 first, before starting to use your inhaler.
Remove the cap from the mouthpiece.
Hold the inhaler as shown in the picture (with the arrow on the label pointing upwards) and breathe out gently.
Then straight away, put the mouthpiece in your mouth.
Hold the mouthpiece with your lips. Start to breathe in slowly and deeply through your mouth.
Press the top of the inhaler firmly. This will release one puff of your medicine. Keep breathing in.
Hold your breath for as long as is comfortable.
If possible hold your breath for 10 seconds.
Then breathe out slowly.
• If you are having more than one puff, wait at least 1 minute before the next puff.
• Then repeat steps 2, 3 and 4.
After use, replace the cap on the mouthpiece.
The mouthpiece has been designed specially for use with this product only. Do not use any other mouthpiece with the product and do not use the mouthpiece provided here with any other product.
If you find breathing in and pressing the inhaler at the same time (step 3) difficult you should talk to your doctor or pharmacist, as you could use a spacer device (Aerochamber Plus™) with your inhaler. A spacer is a device designed to make step 3 easier. A spacer is generally a plastic container with a mouthpiece at one end and a hole for inserting the mouthpiece of the inhaler at the other end.
The puff of medicine from your inhaler is sprayed into the spacer and the puff of medicine stays there, inside the spacer, until you breathe in through your mouth from the spacer with the spacer mouthpiece in your mouth and with your lips closed around it. This means that you do not have to worry about breathing in and pressing the inhaler at the same time.
When using your Ipratropium take care not to let any of the spray enter your eyes. If any of the spray accidentally gets into your eyes you may get painful, stinging or red eyes, dilated pupils, blurred vision, see colours or lights. If this happens, talk to your doctor for advice. If you get problems with your eyes at any other time, talk to your doctor for advice. You may be developing glaucoma, which will need treatment straight away.
Cleaning
It is important to clean your inhaler regularly. Otherwise it may not work properly.
• Remove the canister and cap
• Wash and clean the white mouthpiece in warm soapy water
• Rinse in warm water and allow to air-dry without using any heating system
• Make sure the small hole in the mouthpiece is washed through thoroughly
• Once the white mouthpiece is dry, replace the canister and the cap
Make sure you do not run out of Ipratropium
The inhaler has been designed to deliver 200 puffs of your medicine. However, it is not possible to tell when the inhaler is empty and when the 200 puffs have been used. There may still be a small amount of fluid left over in the container. Please make sure that your inhaler is replaced after you have taken 200 puffs (usually after 3-4 weeks of regular use) so that you can be certain that you are getting the right amount of your medicine in each puff.
If you use more Ipratropium than you should
If you use more of this inhaler than you should, talk to a doctor or go to a hospital straight away. Take all your inhalers and any other medicines you are taking (in their packaging if possible) with you. If you take too much or too many puffs you may get a dry mouth, a rapid heart rate or blurred vision.
If you forget to take Ipratropium
• If you forget a dose, inhale it as soon as you remember it.
• However, if it is time for the next dose, skip the missed dose.
• Do not take a double dose to make up for a forgotten dose.
If you have any further questions, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Ipratropium can cause side effects, although not everybody gets them.
Tell your doctor straight away if you notice any the following serious side effects - you may need urgent medical treatment:
• If after taking Ipratropium you are wheezy or have other difficulties in breathing, do not take any more (unless you have been told to by your doctor). You may need to take a fast-acting reliever inhaler such as salbutamol to help your breathing. Your doctor may decide that you need different medicines to help your breathing
• Allergic reactions - the signs may include skin rash and itching (affects less than 1 in 100 people). In severe cases the signs include swelling of your mouth and face, sudden difficulties in breathing and reduction of your blood pressure. Tightening of your throat (affects less than 1 in 100 people)
• Palpitations (fast or uneven heart beats) or quickening of the heart rate (affects less than 1 in 100 people)
• Increased heart rate or irregular heart rhythm such as atrial fibrillation (affects less than 1 in 1000 people)
See your doctor straight away if you have any of these side effects.
The side effects described below have been experienced by people taking Ipratropium and they are listed as either common, uncommon or rare.
Common (affects less than 1 in 10 people)
• Headache, dizziness
• Dry mouth, feeling sick (nausea), stomach upset or discomfort
• Cough and throat irritation when you have just used Ipratropium
Uncommon (affects less than 1 in 100 people)
• Itching, skin rash
• Unexpected tightness of the chest, swelling of the throat, dry throat
• Blurred vision, dilated pupils, glaucoma, painful, stinging, red or swelling of the eyes, see colours or lights
• Diarrhoea, constipation or being sick
• Mouth or lip sores
• Problems passing water (urine), especially if you already have problems passing urine
Rare (affects less than 1 in 1000 people)
• Difficulty focusing
• Nettle rash (urticaria)
If any of the side effects gets troublesome or serious, or if you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
If any of the spray accidentally gets into your eyes you may get painful, stinging or red eyes, dilated pupils, blurred vision, see colours or lights. If this happens, talk to your doctor for advice. If you get problems with your eyes at any other time, talk to your doctor for advice. You may be developing glaucoma, which will need treatment straight away. If your eyes are affected in any way do not drive or operate machinery.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard
By reporting side effects, you can help provide more information on the safety of this medicine.
5. HOW TO STORE IPRATROPIUM
• Keep out of the sight and reach of children
• Do not take your medicine after the expiry date which is stated on the carton and the canister label after ‘Exp'. The expiry date refers to the last day of that month.
• Do not store above 25°C.
• Do not freeze.
• Keep pressurised container away from heat and light.
• Do not expose to temperatures higher than 50°C.
• The canister contains a pressurised liquid. Do not pierce or burn container even when empty.
6. FURTHER INFORMATION What Ipratropium contains
The active ingredient is ipratropium bromide.
Each actuation contains 20 micrograms ipratropium bromide(as the monohydrate)
Other ingredients are HFA 134a (1,1,1,2-tetrafluoroethane), citric acid anhydrous, ethanol anhydrous and purified water.
Ipratropium does not contain any chlorofluorocarbon (CFC) propellants.
You may have been prescribed Ipratropium inhaler CFC-Free as you were previously being treated with Ipratropium inhaler. These products contain the same medicine, ipratropium bromide, but different propellants. Propellants are ingredients which enable the delivery of the medicine to the lungs. Ipratropium inhaler contained chlorofluorocarbons or CFCs as propellants which are known to damage the ozone layer. Your Ipratropium has been developed to include the new propellant HFA-134a which does not damage the ozone layer i.e. Ipratropium does not contain any CFCs. In terms of safety and effectiveness the CFC-Free product is the same as the old CFC-containing product.
What Ipratropium looks like and contents of the pack
Iratropium is an inhaler in which a stainless steel pressurised canister with metering valve and outer clear and white body with a green cap. The canister is filled with a clear, colourless liquid.
Each canister contains 10ml solution (200 actuations).
Each carton contains one inhaler.
Manufactured by: Boehringer Ingelheim Pharma GmbH & Co. KG, Binger Strasse 173, D-55216 Ingelheim/Rhein, Germany.
Procured from within the EU and repackaged by the Product Licence holder: B&S Healthcare, Unit 4, Bradfield Road, Ruislip, Middlesex, HA40NU, UK.
Ipratropium bromide 20 micrograms CFC-Free Inhaler |POM| PL No: 18799/2394
Leaflet date: 29.01.2015