Cilest Tablets
Out of date information, search anotherPg 4 Pg 1
Pg 4 Pg 1
^ Tell your doctor, pharmacist or family planning nurse if you are worried about any side effects which you think may be due to Cilest. Also tell them if any existing conditions get worse while you are taking Cilest.
4.3 Bleeding between periods should not last long
Usually you should only have a withdrawal bleed like a period during the seven pill-free days. However, a few women have a little unexpected bleeding or spotting while they are taking Cilest, especially during the first few months. Normally, this bleeding is nothing to worry about and will stop after a day or two. Keep taking Cilest as usual. The problem should disappear after the first few strips.
You may also have unexpected bleeding if you are not taking your pills regularly, so try to take your pill at the same time every day. Also, unexpected bleeding can sometimes be caused by other medicines.
^ Make an appointment to see your doctor if you get breakthrough bleeding or spotting that:
• carries on for more than the first few months
• starts after you've been taking Cilest for a while
• carries on even after you've stopped taking Cilest.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Cilest
Cilest tablets should be protected from light and not be stored above 25°C.
KEEP ALL MEDICINES OUT OF THE SIGHT AND REACH OF CHILDREN.
Do not use after the expiry date printed on the carton label or blister strip.
If your doctor tells you to stop taking the tablets, please take them back to the pharmacist for safe disposal. Only keep the tablets if your doctor tells you to.
If the tablets become discoloured or show any other signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.
6. What is in Cilest and who makes it
Your medicine is called Cilest tablets. Each tablet contains two active ingredients, 250 micrograms of the progestogen, norgestimate and 35 micrograms of the oestrogen ethinylestradiol in a round light blue tablet marked ‘C 250' on each side.
Cilest tablets also contain the following:
anhydrous lactose, pregelatinized maize starch, magnesium stearate and a dye called FD&C blue No 2 (E132).
Each pack contains 21 tablets or 63 tablets, available as 3 strips of 21 tablets.
POM PL No: 6464/2077
This product is manufactured by Cilag AG, Hochstrasse 201, CH-8205 Schaffhausen, Switzerland and/or Janssen Pharmaceutica NV, Turnhoutseweg 30, B-2340 Beerse, Belgium and/or McGregor Cory Ltd., Exel, Middleton Close, Banbury, Oxon OX16 4RS and is procured from within the EU and repackaged by the Product Licence holder:
Waymade plc, Miles Gray Road, Basildon, Essex SS14 3FR
Leaflet revision and issue date (Ref.) 7.5.2014 Cilest is a registered trademark of Johnson & Johnson.
CILEST® TABLETS (ethinylestradiol/norgestimate)
Patient Information Leaflet
Five important things to know about the Pill.
• The Pill is a reliable contraceptive and may reduce your risk of cancer of the ovary and womb if used fora long time.
• The Pill will not protect you against sexually transmitted diseases.
• This medicine can increase your risk of problems such as blood clots and breast cancer.
• Some women should not take the Pill because of current medical problems or illnesses.
Please read the leaflet to make sure Cilest is right for you.
• To prevent pregnancy it is important to take Cilest as instructed and start each strip on time.
Please make sure that you understand what to do if you miss a pill or think you are pregnant.
Read all of this leaflet carefully before you start taking this medicine.
• Keep this leaflet. You may need to read it again.
• If you have any questions or need more advice, ask your doctor, family planning nurse or pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them.
• If any of the side effects gets severe, or if you notice any not listed in this leaflet, please tell your doctor, family planning nurse or pharmacist.
|
In this |
eaflet: |
|
1. |
What Cilest does |
|
2. |
Make sure Cilest is OK for you |
|
3. |
Taking Cilest |
|
3.3 |
A missed pill |
|
4. |
Possible side effects |
|
5. |
How to store Cilest |
|
6. |
What is in Cilest and who makes it |
1. What Cilest does
Cilest is a combined oral contraceptive pill (‘the Pill'). You take it to stop getting pregnant.
This contraceptive contains two types of female sex hormones, oestrogen and progestogen. These hormones prevent an egg being released from your ovaries so you can't get pregnant. Also, Cilest makes the fluid (mucus) in your cervix thicker which makes it more difficult for sperm to enter the womb.
Cilest is a 21-day Pill - you take one each day for 21 days, followed by 7 days when you take no pills.
The benefits of taking the Pill include:
• it is one of the most reliable reversible methods of contraception if used correctly
• it doesn't interrupt sex
• it usually makes your periods regular, lighter and less painful
• it may help with pre-menstrual symptoms.
Cilest will not protect you against sexually transmitted infections, such as Chlamydia or HIV. Only condoms can help to do this.
Cilest needs to be taken as directed to prevent pregnancy.
2. Make sure Cilest is OK for you
It's important that you understand the benefits and risks of taking the Pill before you start taking it, or when deciding whether to carry on taking it. Although the Pill is suitable for most healthy women it isn't suitable for everyone.
- Tell your doctor if you have any of the illnesses or risk factors mentioned in this leaflet.
Before you start taking the Pill
• Your doctor will ask about you and your family's medical problems and check your blood pressure. You may also need other checks, such as a breast examination but only if these are necessary for you or you have any special concerns.
While you're on the Pill
• You will need regular check-ups with your doctor or family planning nurse, usually when you need another prescription of the Pill.
• You should go for regular cervical smear tests.
• Check your breasts and nipples every month for changes - tell your doctor if you can see or feel anything odd, such as lumps or dimpling of the skin.
• If you need a blood test tell your doctor that you are taking the Pill, because the Pill can affect the results of some tests.
• If you're going to have an operation, make sure your doctor knows about it. You may need to stop taking the Pill about 4-6 weeks before the operation. This is to reduce the risk of a blood clot (see section 2.1).
Your doctor will tell you when you can start taking the Pill again.
2.1 The Pill and blood clots
The Pill may slightly increase your risk of having a blood clot (called a thrombosis), especially in the first year of taking it.
A clot in a leg vein - a deep vein thrombosis (or DVT) - is not always serious. However, if it moves up the veins to the lungs, it can cause chest pain, breathlessness, collapse or even death. This is called a ‘pulmonary embolism' and is very rare.
Your chances of having a blood clot are only increased slightly by taking the Pill.
• Of 100,000 women who are not on the Pill and not pregnant, about 5 will have a blood clot in a year.
• Of 100,000 women taking a Pill such as Cilest, about 20-40 will have a blood clot in a year.
• Of 100,000 women who are pregnant, around 60 will have a blood clot in a year.
You are more at risk of having a blood clot in your veins:
• as you get older
• if you are seriously overweight
• if you smoke
• if you or any of your close family have had blood clots
• if you have any blood clotting problem that needs treatment with a medicine such as warfarin
• if you're off your feet for a long time because of major surgery, injury or illness
• if you have had one or more miscarriages
• if you have recently had a baby
^ Tell your doctor if any of these risk factors apply to you. Taking the Pill may add to this risk so Cilest may not be suitable for you.
Signs of a blood clot include:
• painful swelling in your leg
• sudden chest pain, difficulty breathing
• sudden changes in eyesight (such as loss of vision or blurred vision)
^ See a doctor as soon as possible. Do not take any more Cilest until your doctor says you can. Use other method of contraception, such as condoms, in the meantime.
Very rarely, blood clots can also form in the blood vessels of the heart (causing a heart attack) or the brain (causing a stroke). In healthy young women the chance of having a heart attack or stroke is extremely small.
You are more at risk of having a heart attack or stroke:
• as you get older
• if you have high blood pressure
• if you smoke or drink too much alcohol
• if you have high levels of fat in your blood or are seriously overweight
• if you have an irregular heartbeat (atrial fibrillation), problems with heart valves or heart failure
• if you or someone in your close family has had a heart attack or stroke at a young age
• if you have migraines
• if you have diabetes
• if you have a blood problem called sickle cell anaemia
^ Tell your doctor if any of these risk factors apply to you. Taking the Pill may add to this risk so Cilest may not be suitable for you.
Signs of a heart attack or stroke include:
• sudden crushing pains in your chest which may reach your left arm
• sudden weakness or numbness in one side or part of your body
• severe headache or migraine for the first time or worse than normal
• slurred speech or any other difficulties affecting your speech
• any sudden changes to your eyesight (such as loss of vision or blurred vision)
^ See a doctor as soon as possible. Do not take any more Cilest until your doctor says you can. Use another method of contraception, such as condoms, in the meantime.
2.2 The Pill and cancer
The Pill reduces your risk of cancer of the ovary and womb if used for a long time. However, it also seems to slightly increase your risk of cancer of the cervix - although this may be due to having sex without a condom, rather than the Pill. All women should have regular smear tests.
If you have breast cancer, or have had it in the past, you should not take the Pill. The Pill slightly increases your risk of breast cancer. This risk goes up the longer you're on the Pill, but returns to normal within about 10 years of stopping it. Because breast cancer is rare in women under the age of 40, the extra cases of breast cancer in current and recent Pill users are small. For example:
• Of 10,000 women who have never taken the Pill, about 16 will have breast cancer by the time they are 35 years old.
• Of 10,000 women who take the Pill for 5 years in their early twenties, about 17-18 will have breast cancer by the time they are 35 years old.
• Of 10,000 women who have never taken the Pill, about 100 will have breast cancer by the time they are 45 years old.
• Of 10,000 women who take the Pill for 5 years in their early thirties, about 111 will have breast cancer by the time they are 45 years old.
Your risk of breast cancer is higher:
• as you get older
• if you have a close relative (mother, sister or grandmother) who has had breast cancer
• if you are seriously overweight
^ See a doctor as soon as possible if you notice any changes in your breasts, such as dimpling of the skin, changes in the nipple or any lumps you can see or feel.
Taking the Pill has also been linked to liver diseases, such as jaundice and non-cancer liver tumours, but this is rare. Very rarely, the Pill has also been linked with some forms of liver cancer in women who have taken it for a long time.
^ See a doctor as soon as possible if you get severe pain in your stomach, or yellow skin or eyes (jaundice). You may need to stop taking Cilest.
2.3 Cilest should not be taken by some women
^ Tell your doctor or family planning nurse if you have any medical problems or illnesses.
Do not take Cilest if any of the following apply to you:
• If you are breast feeding and your baby is less than 6 weeks old
• If you have breast or liver cancer
• If you have an irregular heartbeat (atrial fibrillation), problems with heart valves or heart failure
• If you have ever had a problem with your blood circulation. This includes blood clots, for example
in the legs (deep vein thrombosis) or lungs (pulmonary embolism), or a heart attack or stroke
• If you have any conditions which make you more at risk of a blood clot (thrombosis - see section 2.1), such as having an operation and being off your feet for a long time
• If you have very high blood pressure
• If you smoke 15 or more cigarettes a day and you are 35 years old or more
• If you have migraines which affect your vision
• If you have had diabetes for more than 20 years or have diabetes with secondary problems
• If you have or have recently had a severe liver disease
• If you have the disease systemic lupus erythematosus (SLE) with or without Raynaud's disease
• If you are allergic (hypersensitive) to any of the ingredients in Cilest.
^ If you suffer from any of these, or get them for the first time while taking Cilest, contact your
doctor as soon as possible. Do not take Cilest as it may put your health at risk.
2.4 Cilest can make some illnesses worse
Some of the conditions listed below can be made worse by taking the Pill. Or they may mean it is less suitable for you. You may still be able to take Cilest but you need to take special care and have check-ups more often. Tell your doctor or family planning nurse if any of these apply to you:
• If you have problems with your heart, circulation or blood clotting, such as high blood pressure
• If you have diabetes without secondary problems
• If you have gall bladder problems
• If you have ulcerative colitis or Crohn's disease (inflammation of the gut which causes pain in the abdomen, frequent diarrhoea and tiredness)
• If you have porphyria
• If you have a history of migraines
• If you have brown patches on your face or body (chloasma) as you may need to keep out of the sun
• If you have (or you have a family history of) high levels of fat in your blood as you may have a higher risk of pancreatitis (inflammation of the pancreas, which causes severe pain in the abdomen and back)
• If you have had any of the following problems while pregnant or during previous Pill use, such as itchy skin or blister-like rash, yellowing of skin or eyes, hearing problem, systemic lupus erythematosus (SLE), severe headaches, uncontrollable jerky movements, severe diarrhoea with blood in stools (diagnosed as haemolytic uraemic syndrome or HUS).
^ Tell your doctor or family planning nurse if any of these apply to you. Also tell them if you get any of these for the first time while taking the Pill, or if any get worse or come back, because you may need to stop taking Cilest and use another method of contraception, such as condoms.
2.5 Taking other medicines
If you ever need to take another medicine at the same time as being on the Pill, always tell your doctor, pharmacist or dentist that you're taking Cilest. Also check the leaflets that come with all your medicines to see if they can be taken with hormonal contraceptives.
Some medicines can stop Cilest from working properly - for example:
• some medicines used to treat epilepsy (such as topiramate, carbamazepine, phenytoin, fosphenytoin, oxcarbazepine, felbamate, primidone, eslicarbamazepine acetate, rufinamide)
• bosentan (for high blood pressure in the blood vessels of the lungs)
• antibiotics including rifampicin and rifabutin (for treatment of TB); also ampicillin and tetracyclines
• anti-HIV medicines
• aprepitant and fosaprepitant (for prevention of nausea and vomiting caused by certain cancer drug treatment)
• griseofulvin (for fungal infections)
• modafinil (for excessive daytime sleepiness)
• certain sedatives (called ‘barbiturates')
• St. John's Wort (a herbal remedy)
• metoclopramide (to increase movement through the gut)
• charcoal
• colesevelam (to treat high cholesterol levels)
• etoricoxib (to help with pain and inflammation or arthritis)
If you do need to take one of these medicines, Cilest may not be suitable for you or you may need to use extra contraception for a while. Your doctor, pharmacist or dentist can tell you if this is necessary and for how long.
Cilest can also affect other medicines - for example:
• ciclosporin (to prevent transplant rejection and for rheumatoid arthritis or some skin problems)
• lamotrigine (for epilepsy)
• prednisolone (a steroid to reduce inflammation)
• selegiline (for Parkinson's disease)
• theophylline (for asthma, bronchitis and emphysema)
• tizanidine (used to relax muscles)
Talk to your doctor before having Cilest if you are taking any of these medicines. They may have to change how much of these medicines you are taking.
2.6 Taking Cilest with food and drink
There are no special instructions about food and drink while on Cilest.
2.7 Pregnancy and breast-feeding
Do not start to use Cilest if you are pregnant. If you think you might be pregnant while taking Cilest, do a pregnancy test to confirm that you are before you stop taking it.
If you are breast-feeding, your doctor or family planning nurse may advise you not to take Cilest.
Talk to them about alternative contraception. Breast-feeding may not stop you getting pregnant.
2.8 Driving and using machines
Cilest has no known effect on the ability to drive or use machines.
2.9 Cilest contains lactose
If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before using Cilest.
3. Taking Cilest
3.1 How to take it
To prevent pregnancy, always take Cilest as described below. Check with your doctor or family planning nurse if you are not sure.
Take Cilest every day for 21 days
Cilest comes in a strip of 21 pills, each marked with a day of the week.
• Take your pill at the same time every day.
• Start by taking a pill marked with the correct day of the week.
• Follow the direction of the arrows on the strip. Take one pill each day.
• Swallow each pill whole, with water if necessary. Do not chew the pill.
Then have seven pill-free days
After you have taken all 21 pills in the strip, you have seven days when you take no pills. So if you take the last pill of one pack on a Friday, you will take the first pill of your next pack on the Saturday of the following week.
Within a few days of taking the last pill from the strip, you should have a withdrawal bleed like a period. This bleed may not have finished when it is time to start your next strip of pills.
You don't need to use extra contraception during these seven pill-free days - as long as you have taken your pills correctly and start the next strip of pills on time.
Then start your next strip
Start taking your next strip of Cilest after the seven pill-free days - even if you are still bleeding.
Always start the new strip on time.
As long as you take Cilest correctly, you will always start each new strip on the same day of the week.
3.2 Starting Cilest
As a new user or starting the Pill again after a break
Either take your first Cilest pill up to and including day 5 of your next period (counting the first day of your period as day 1). This way, you will have contraceptive protection with your first pill.
Or start taking Cilest at any time, if you are sure you are not already pregnant. But then you must use extra contraception, such as condoms, until you have taken the first 7 pills correctly.
Changing to Cilest from another contraceptive
If you are currently taking another Pill and you are taking it correctly, you can start Cilest at any time, if you are sure you are not already pregnant. There is no need to wait for your next period to start and you don't need extra contraception. If you are currently using a non-hormonal method and your period started more than 5 days ago, you must use extra contraception, such as condoms, until you have taken the first 7 pills correctly.
Starting Cilest after a miscarriage or abortion
If you have had a miscarriage or an abortion, your doctor may tell you to start taking Cilest straight away. This means that you will have contraceptive protection with your first pill.
Contraception after having a baby
If you have just had a baby, your doctor may tell you to start taking Cilest 21 days after the birth. This means that you will have contraceptive protection with your first pill.
If you start Cilest after this, you must use extra contraception, such as condoms, until you have taken the first 7 pills correctly.
3.3 A missed pill
Missing pills or starting a strip late may make your pill less effective. The chance of pregnancy after missing pills depends on when pills are missed and how many pills are missed.
Missing one pill anywhere in your strip or starting a new strip one day late is not a problem.
Missing more than one or starting a strip more than one day late may affect your contraceptive cover.
It is more risky to start a strip late and miss more than one pill.
|
How many pills have you missed? | |
|
T |
T |
|
One pill |
Two or more pills |
T -T
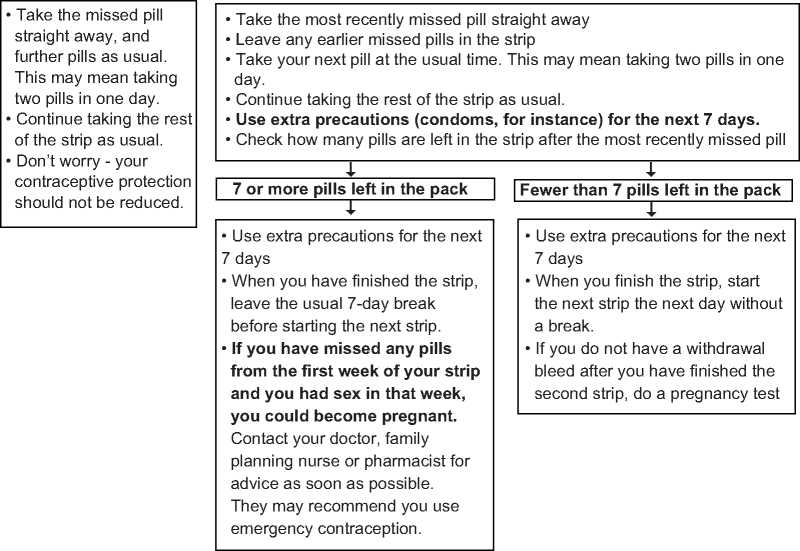
If you have missed any of the pills in a strip, and you do not bleed in the first pill-free break, you may be pregnant. Contact your doctor or family planning clinic, or do a pregnancy test yourself.
If you start a new strip of pills late, or make your ‘week off' longer than eight days, you may not be protected from pregnancy. If you had sex in the last seven days, ask your doctor, family planning nurse or pharmacist for advice. You may need to consider emergency contraception. You should also use extra contraception, such as a condom, for seven days.
3.4 A lost pill
If you lose a pill, just take a pill from a spare strip. Then take all the other pills from your current strip as usual. You can then keep the opened spare strip in case you lose any more pills.
3.5 If you are sick or have diarrhoea
If you are sick or have very bad diarrhoea, your body may not get its usual dose of hormones from that pill.
If you have been sick within 2 hours of taking Cilest, just take a pill from a spare strip. Carry on taking your pills as normal if you can. You won't need to use extra contraception.
If you are still sick or have diarrhoea for more than 1 day, follow the instructions for a missed pill - see section 3.3, A missed pill.
^ Talk to your doctor if your stomach upset carries on or gets worse. He or she may recommend another form of contraception.
3.6 Missed a period - could you be pregnant?
Occasionally, you may miss a withdrawal bleed. This could mean that you are pregnant, but that is very unlikely if you have taken your pills correctly. Start your next strip at the normal time. If you think that you might have put yourself at risk of pregnancy (for example, by missing pills or taking other medicines), or if you miss a second bleed, you should do a pregnancy test. You can buy these from the chemist or get a free test at your family planning clinic or doctor's surgery. If you are pregnant, stop taking Cilest and see your doctor.
3.7 Taking more than one pill should not cause harm
It is unlikely that taking more than one pill will do you any harm, but you may feel sick, vomit or have some vaginal bleeding. Talk to your doctor if you have any of these symptoms.
3.8 You can delay a period
If you want to delay having a period, finish the strip of pills you are taking. Start the next strip the next day without a break. Pill taking should then continue as usual.
When you use the second strip, you may have some unexpected bleeding or spotting on the days that you take the pill, but don't worry. Take the next strip after the usual 7 day break even if you are still bleeding or spotting.
3.9 When you want to get pregnant
If you are planning a baby, it's best to use another method of contraception after stopping Cilest until you have had a proper period. Your doctor or midwife relies on the date of your last natural period to tell you when your baby is due. The Pill may reduce the levels of folic acid in the blood.
Talk to your doctor, nurse or pharmacist as this could be important if you get pregnant straight after stopping the Pill.
4. Possible side effects
Like all medicines, Cilest can cause side effects, although not everybody gets them.
^ Tell your doctor, pharmacist or family planning nurse if you are worried about any side effects which you think may be due to Cilest.
4.1 Serious side effects - see a doctor straight away Signs of a blood clot in a vein include:
• painful swelling in your leg
• sudden chest pain, difficulty breathing
• sudden changes in eyesight (such as loss of vision or blurred vision)
Signs of heart attack or stroke include:
• a severe headache or migraine for the first time, or any that is worse than normal
• sudden changes in eyesight (such as loss of vision or blurred vision)
• sudden weakness or numbness in one side or part of your body
• slurred speech or any other difficulties affecting your speech
• sudden crushing pains in your chest which may reach your left arm.
Signs of breast cancer include:
• dimpling of the skin
• changes in the nipple
• any lumps you can see or feel.
Signs of severe liver problems include:
• severe pain in your upper abdomen
• yellow skin or eyes (jaundice).
Other serious side effects include:
• increased blood pressure
• fits (convulsions)
• hives (urticaria), swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing. These may be signs of allergy.
^ If you think you may have any of these, see a doctor straight away. You may need to stop taking Cilest.
4.2 Other possible side effects - tell your doctor
Very common side effects (affects more than 1 in 10 patients)
• Headache (but if severe, unusual or long lasting, see a doctor as soon as possible)
• Stomach problems such as nausea, vomiting and diarrhoea
• Bleeding and spotting between your periods for the first few months (though this usually stops when your body adjusts to Cilest) - see section 4.3, Bleeding between periods should not last long.
• Painful or unusual periods.
Common side effects (affects more than 1 in 100 patients)
• Migraine (see a doctor as soon as possible if this is your first migraine or it's worse than usual)
• Swollen hands, ankles or feet
• Depression; mood changes; feeling nervous or dizzy
• Difficulty sleeping (insomnia)
• Stomach ache and bloating; constipation; wind
• Acne; rash
• Muscle spasms; pain in the legs, arms and back
• Painful breasts
• Urinary tract infections (pain on passing urine)
• Vaginal infections such as thrush
• Vaginal discharge
• No menstrual periods
• Feeling weak
• Weight gain.
Uncommon side effects (affects fewer than 1 in 100 patients)
• Breast problems, such as fuller breasts; producing fluid from the nipples
• Abnormal cells in the cervix (identified by a smear test)
• Feeling anxious or faint; tingling sensation or numbness
• Changes in skin colour
• Skin problems such as redness and itchiness
• Hair thinning (alopecia), excessive hair growth
• Changes in appetite
• Weight may vary
• Change in sex drive
• Dry eyes
• Changes in vision
• Palpitations (feeling your heart beat)
• Hot flushes
• Muscle pain
• Vaginal dryness
• Ovarian cysts (may cause pain and swelling of the abdomen, changes in periods)
Rare side effects (affects fewer than 1 in 1000 patients)
• Lumpy breasts
• Loss of sex drive
• Feeling giddy
• Faster heart beat
• Pancreatitis (inflammation of the pancreas, which causes severe pain in the abdomen and back)
• Increased sweating
• Sensitivity to light
Frequency not known
• Reduced amount of breast milk (if breast feeding)
• Contact lenses may feel uncomfortable
• Red painful lumpy swellings on the legs
• Changes in fat levels in the blood (seen by blood tests)
• Night sweats