Cilique 250/35 Microgram Tablets
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Cilique 250/ 35 microgram tablets
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
Each tablet contains 250 micrograms of norgestimate and 35 micrograms of ethinylestradiol.
Excipients with known effect: Lactose 75.74 mg For the full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Tablet
Blue, round, biconvex tablets approximately 6mm in diameter.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Hormonal contraception.
The decision to prescribe Cilique should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Cilique compares with other Combined Hormonal Contraceptives (CHCs) (see sections 4.3 and 4.4).
4.2 Posology and method of administration
For oral administration.
Adults:
How to use Cilique:
One tablet is to be taken at around the same time of day on each of 21 consecutive days followed by a tablet-free interval of 7 days. Each subsequent pack is started after keeping a tablet-free interval. Withdrawal bleed occurs usually 2-3 days after the last tablet and may not finish before the next pack is started.
How to start Cilique:
No preceding hormonal contraceptive use in the last month Tablet-taking from the first pack of Cilique is started on the 1st day of the menstrual cycle, i.e. the first day of menstrual bleeding. If menstruation has already begun, Cilique may be commenced up to day 5 of the menstrual period, provided additional contraceptive precautions are taken for the first 7 days of tablet taking.
- Changing from a combined contraceptive (combined oral contraceptive (COC), vaginal ring or transdermalpatch) to Cilique:
The woman should start taking Cilique the next day after having taken the last active tablet of her previous pack of contraceptive pills - but no later than the day after the usual tablet-free or placebo-tablet period of her previous contraceptive pill.
In case a vaginal ring or transdermal patch has been used the woman should start using Cilique preferably on the day of removal, but at the latest when the next application would have been due.
- Changing from a progestin-only method (progestin-only pill, injection, implant) or from a progestogen-releasing intrauterine system (IUS):
The woman may change from progestogen-only pills (POPs) any day. The first tablet should be taken the day after any tablet of the POP pack. When changing from an implant or the IUS, Cilique should be started the day when the implant is removed. When changing from injections, Cilique should be started when the next injection is to be given. In all these cases the woman is advised to use also a barrier method for the first 7 days of taking the Pills.
Following a first trimester abortion:
Cilique can be used immediately, while another additional contraceptive method is not needed.
Following delivery or a second-trimester abortion
Women should be advised to start at day 21 to 28 day after delivery or second trimester abortion. When starting later, the woman should be advised to additionally use a barrier method for the first 7 days. However, if intercourse has already occurred, pregnancy should be excluded before the actual start of COC use or the woman has to wait for her first menstrual period.
NB: When oral contraceptives are administered in the immediate postpartum/post miscarriage period, the increased risk of thromboembolic disease must be considered.
Missed tablets:
Missing a tablet for less than 12 hours does not diminish the, contraceptive protection. The woman should take the tablet as soon as she remembers and proceed taking the rest of the tablets as usual.
Missing a tablet for more than 12 hours can diminish the contraceptive protection. The two following rules may be helpful in dealing with missed tablets:
1. Taking tablets should never be delayed by a period discontinued for longer than 7 days.
2. It takes 7 days of uninterrupted ingestion of the tablets to achieve suppression of the hypothalamus-pituitary- ovarian-axis.
Thus, the following advice can be given in daily practice:
Week 1
The user should take the last missed tablet as soon as she remembers, even if this means that she needs to take 2 tablets at the same time. From then on she should continue to take the tablets at the usual time. At the same time she should use a barrier method, i.e. condom, for the next 7 days. If she had intercourse during the previous 7 days, she should consider the possibility that she might be pregnant. The more tablets have been missed, and the closer this happened to the monthly tablet-free period, the higher the risk of pregnancy is.
Week 2
The user should take the last missed tablet as soon as she remembers, even if it means that she has to take 2 tablets at the same time. From then on, she should go ahead with taking the tablets at the usual time. If the tablets have been taken correctly for the 7 days prior to the missed tablet, it is not necessary to take any additional contraceptive precautions. If this is not the case, however, or if more than 1 tablet has been missed, the woman should be advised to use another birth-control method for 7 days.
Week 3
The risk of reduced protection is imminent because of the approaching tablet-free period. The reduced contraceptive protection can be prevented, however, by adjusting the intake of the tablets. It is, therefore, not necessary to take any additional contraceptive precautions, provided that the tablets have been taken correctly for the 7 days prior to the missed tablet, if one follows any of the following choices. If this is not the case, the woman should be advised to go ahead according to the first of the two opportunities, and at the same time use another birth-control method for 7 days.
1.The patient should take the last missed tablet as soon as she remembers, even if this means taking two tablets at the same time. She then continues to take tablets at her usual time. The next pack must be started as soon as the current pack is finished, i.e. no gap should be left between packs. The patient is unlikely to have a withdrawal bleed until the end of the second pack, but she may experience spotting or breakthrough bleeding on tablet-taking days.
2. The woman may also be advised to discontinue tablet-taking from the current pack. She should then have a tablet- free interval of up to 7 days, including the days she missed tablets, and subsequently continue with the next pack.
If the woman missed tablets and subsequently has no withdrawal bleed in the first normal tablet-free interval, the possibility of a pregnancy should be considered.
- Postpartum
Women who choose not to breast-feed their newborn infant may start a new Cilique treatment on the first day of the first spontaneous menstruation or 3 weeks after delivery, whichever comes first. However, if intercourse has already occurred, pregnancy should be excluded before the actual start of COC use or the woman has to wait for her first menstrual period.
- Delaying of menstruation
When all the tablets of the strip have been taken, a new strip can be started and tablets taken for the number of days needed. Subsequently, no tablets are taken for 7 days, followed by starting a new strip of 21 tablets with a new start day.
- Absence of withdrawal bleeding
If, in exceptional cases, withdrawal bleeding fails to occur, pregnancy must be ruled out before the use of Cilique is continued.
Procedure in the event of irregular bleeding Breakthrough bleeding and spotting are sometimes encountered, primarily during the first three months of use, and usually cease spontaneously. The woman, therefore, should continue to use Cilique even if irregular bleeding occurs. Should break-through bleeding persist or recur, appropriate diagnostic measures to exclude an organic cause are indicated, and may include curettage.
This also applies in the case of spotting which occurs at irregular intervals in several consecutive cycles or which occurs for the first time after long use of Cilique.
Gastro-intestinal upset
Vomiting or diarrhoea may reduce the efficacy of oral contraceptives by preventing full absorption. If vomiting occurs within 3 hours of taking the tablet, or if severe diarrhoea lasts for more than 24 hours, the effectiveness of the contraception may not be adequate, and an additional non-hormonal method of contraception should be used until 7 tablets have been taken for 7 days without interruption. If these 7 days overrun the end of a pack, the next pack should be started without a break. In this situation, a withdrawal bleed should not be expected until the end of the second pack.
If the patient does not have a withdrawal bleed during the tablet-free
interval following the end of the second pack, the possibility of pregnancy must be ruled out before resuming with the next pack. Other methods of contraception should be considered if the gastro-intestinal disorder is likely to be prolonged (i.e. greater than 12 hours).
Children:
Safety and efficacy of Cilique Tablets have only been established in women of reproductive age.
Elderly:
Not indicated in post menopausal women.
4.3 Contraindications
Combined hormonal contraceptives (CHCs) should not be used in the following conditions:
- Presence or risk of venous thromboembolism (VTE)
• Venous thromboembolism - current VTE (on anticoagulants) or history of (e.g. deep venous thrombosis [DVT] or pulmonary embolism [PE])
• Known hereditary or acquired predisposition for venous thromboembolism, such as APC-resistance, (including Factor V Leiden), antithrombin-III-deficiency, protein C deficiency, protein S deficiency (see section 4.4)
• Major surgery with prolonged immobilisation (see section 4.4)
• A high risk of venous thromboembolism due to the presence of multiple risk factors
(see section 4.4)
- Presence or risk of arterial thromboembolism (ATE)
• Arterial thromboembolism - current arterial thromboembolism, history of arterial thromboembolism (e.g. myocardial infarction) or prodromal condition (e.g. angina pectoris)
• Cerebrovascular disease - current stroke, history of stroke or prodromal condition
(e.g. transient ischaemic attack, TIA)
• Known hereditary or acquired predisposition for arterial thromboembolism, such
as hyperhomocysteinaemia and antiphospholipid-antibodies (anticardiolipin- antibodies, lupus anticoagulant)
• History of migraine with focal neurological symptoms
A high risk of arterial thromboembolism due to multiple risk factors (see section 4.4)
or to the presence of one serious risk factor such as:
• diabetes mellitus with vascular symptoms
• severe hypertension
• severe dyslipoproteinaemia
- Acute or chronic liver disease, including hepatitis (viral or non-viral) or severe cirrhosis, or a history of these conditions until at least 3 months after abnormal liver function tests have returned to normal; hepatic adenomas or carcinomas.
- Known or suspected sex-steroid influenced malignancies (e.g. of the genital
organs or
the breast)
- Undiagnosed vaginal bleeding
- Hypersensitivity to the active substances or to any of the excipients
Should any of the conditions appear during CHC use, the product should be stopped immediately.
4.4 Special warnings and precautions for use Warnings
Adults:
If any of the conditions/risk factors mentioned below is present, the suitability of Cilique should be discussed with the woman.
In the event of aggravation, or first appearance of any of the conditions or risk factors, the woman should be advised to contact her doctor to determine whether the use of Cilique should be discontinued.
Exclude likelihood of pregnancy before starting treatment.
In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Conditions requiring supervision
- The theoretical or proven risks usually outweigh the advantages of using Combined
oral contraceptives (COCs) in the conditions listed below. Consequently the decision
to prescribe the COC must be made with specialist clinical judgement.
Breast feeding (see section 4.6).
- Increased risk of venous thromboembolic disorders (See section 4.3 and “Circulatory disorders” below).
- Adequately controlled hypertension (persistently elevated baseline systolic values 140-159 mm Hg or diastolic values 90-94 mm Hg).
- Obesity (BMI > 35 kg/m2).
- History of cholestasis (related to COCs), current or medically treated gall bladder disease, porphyria.
- History of breast cancer, 5 years disease-free.
Circulatory disorders
Risk of Venous Thromboembolism (VTE)
The use of any CHCs increases the risk of venous thromboembolism (VTE) compared with no use. Products that contain levonorgestrel, norgestimate (including Cilique) or norethisterone are associated with the lowest risk of VTE. The decision to use Cilique should be taken after a discussion with the woman to ensure she understands the risk of VTE with Cilique, how her current risk factors influence this risk, and that her VTE risk is highest in the first ever year of use. There is also some evidence that the risk is increased when a CHC is re-started after a break in use of 4 weeks or more.
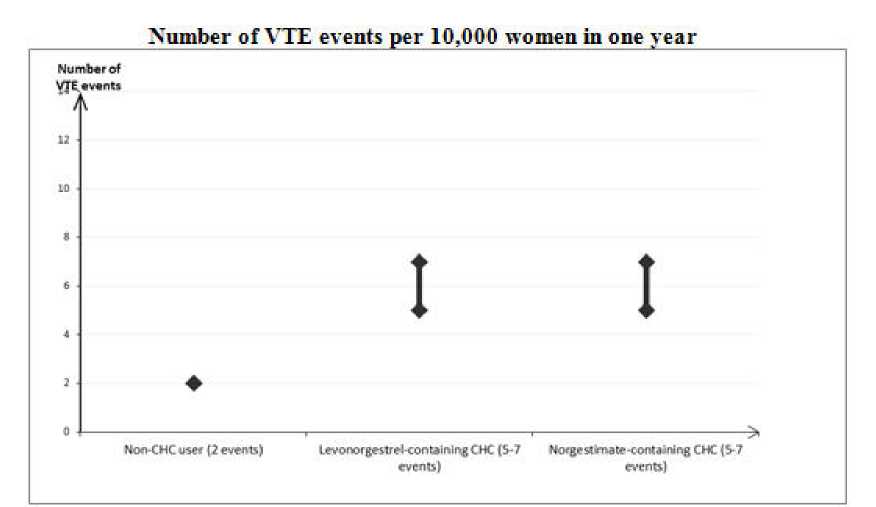
In women who do not use a CHC and are not pregnant, about 2 out of 10,000 will develop a VTE over the period of one year. However, in any individual woman the risk may be far higher, depending on her underlying risk factors (see below).
It is estimated that out of 10,000 women who use a CHC that contains levonorgestrel, about 6 will develop a VTE in a year.
Current evidence suggests that the risk of VTE with use of norgestimate-containing CHCs is similar to the risk with levonorgestrel-containing CHCs.
This number of VTEs per year is fewer than the number expected in women during pregnancy or in the postpartum period.
VTE may be fatal in 1-2% of cases.
Extremely rarely, thrombosis has been reported to occur in CHC users in other blood vessels, e.g. hepatic, mesenteric, renal or retinal veins and arteries.
Risk factors for VTE
The risk for venous thromboembolic complications in CHC users may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see table).
Cilique is contraindicated if a woman has multiple risk factors that put her at high risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors - in this case her total risk of VTE should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3).
Table: Risk factors for VTE
|
Risk factor |
Comment |
|
Obesity (body mass index over 30 kg/m ) |
Risk increases substantially as BMI rises. Particularly important to consider if other risk factors also present. |
|
Prolonged immobilisation, major surgery, any surgery to the legs or pelvis, neurosurgery, or major trauma Note: temporary immobilisation including air travel >4 hours can also be a risk factor for VTE, particularly in women with other risk factors |
In these situations it is advisable to discontinue use of the patch/Pill/ring (in the case of elective surgery at least four weeks in advance) and not resume until two weeks after complete remobilisation. Another method of contraception should be used to avoid |
|
unintentional pregnancy. Antithrombotic treatment should be considered if Cilique has not been discontinued in advance. | |
|
Positive family history (venous thromboembolism ever in a sibling or parent especially at a relatively early age e.g. before 50) |
If a hereditary predisposition is suspected, the woman should be referred to a specialist for advice before deciding about any CHC use. |
|
Other medical conditions associated with VTE |
Cancer, systemic lupus erythematosus, haemolytic uraemic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis) and sickle cell disease. |
|
Increasing age |
Particularly above 35 years old. |
There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in the onset or progression of venous thrombosis.
The increased risk of thromboembolism in pregnancy, and particularly the 6 week period of the puerperium, must be considered (for information on “Pregnancy and lactation” see section 4.6; see also graph on VTE risk).
Symptoms of VTE (deep vein thrombosis and pulmonary embolism)
In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC.
Symptoms of deep vein thrombosis (DVT) can include:
unilateral swelling of the leg and/or foot or along a vein in the leg
pain or tenderness in the leg which may be felt only when standing or walking
increased warmth in the affected leg; red or discoloured skin on the leg. Symptoms of pulmonary embolism (PE) can include: sudden onset of unexplained shortness of breath or rapid breathing sudden coughing which may be associated with haemoptysis sharp chest pain
severe light headedness or dizziness
Some of these symptoms (e.g. shortness of breath, coughing) are nonspecific and might be misinterpreted as more common or less severe events (e.g. respiratory tract infections).
Other signs of vascular occlusion can include: sudden pain, swelling and slight blue discolouration of an extremity.
If the occlusion occurs in the eye, symptoms can range from painless blurring of vision which can progress to loss of vision. Sometimes loss of vision can occur almost immediately.
Risk of arterial thromboembolism (ATE)
Epidemiological studies have associated the use of CHCs with an increased risk for arterial thromboembolism (myocardial infarction) or for cerebrovascular accident (e.g. transient ischaemic attack, stroke). Arterial thromboembolic events may be fatal.
Risk factors for ATE
The risk of arterial thromboembolic complications or of a cerebrovascular accident in CHC users increases in women with risk factors (see table).
Cilique is contraindicated if a woman has one serious or multiple risk factors for ATE that puts her at high risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors - in this case her total risk should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3).
Table: Risk factors for ATE
|
Risk factor |
Comment |
|
Increasing age |
Particularly above 35 years old. |
|
Smoking |
Women should be advised not to smoke if they wish to use a CHC. Women over 35 years old who continue to smoke should be strongly advised to use a different method of contraception. |
|
Hypertension | |
|
2 Obesity (body mass index over 30 kg/m ) |
Risk increases substantially as BMI increases. Particularly important in women with additional risk factors. |
|
Positive family history (arterial thromboembolism ever in a sibling or parent especially at a relatively |
If a hereditary predisposition is suspected, the woman should be |
|
early age e.g. below 50 years old). |
referred to a specialist for advice before deciding about any CHC use. |
|
Migraine |
An increase in frequency or severity of migraine during CHC use (which may be prodromal of a cerebrovascular event) may be a reason for immediate discontinuation. |
|
Other medical conditions associated with adverse vascular events |
Diabetes mellitus, hyperhomocysteinaemia, valvular heart disease and atrial fibrillation, dyslipoproteinaemia and systemic lupus erythematosus. |
Symptoms of ATE
In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC.
Symptoms of a cerebrovascular accident can include:
- sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- sudden trouble walking, dizziness, loss of balance or coordination
- sudden confusion, trouble speaking or understanding
- sudden trouble seeing in one or both eyes
- sudden, severe or prolonged headache with no known cause
- loss of consciousness or fainting with or without seizure.
Temporary symptoms suggest the event is a transient ischaemic attack (TIA). Symptoms of myocardial infarction (MI) can include:
- pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm, or below the breastbone
- discomfort radiating to the back, jaw, throat, arm, stomach
- feeling of being full, having indigestion or choking
- sweating, nausea, vomiting or dizziness
- extreme weakness, anxiety, or shortness of breath
Medical examination/consultation
Prior to the initiation or reinstitution of Cilique, a complete medical history (including family history) should be taken and pregnancy must be ruled out. Blood pressure should be measured and a physical examination should be performed, guided by the contraindications (see section 4.3) and warnings (see section 4.4).
It is important to draw a woman's attention to the information on venous and arterial thrombosis, including the risk of Cilique compared with other CHCs, the symptoms of VTE and ATE, the known risk factors and what to do in the event of a suspected thrombosis.
The woman should also be instructed to carefully read the user leaflet and to adhere to the advice given. The frequency and nature of examinations should be based upon established practice guidelines and should be adapted to the individual woman.
Women should be advised that hormonal contraceptives do not protect against HIV infections (AIDS) and other sexually transmitted diseases.
In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy.
Hepatic adenomas
Malignant hepatic tumours have been reported on rare occasions in long-term users of oral contraceptives. Benign hepatic tumours have also been associated with oral contraceptive usage. A hepatic tumour should be considered in the differential diagnosis when upper abdominal pain, enlarged liver or signs of intra-abdominal haemorrhage occur. In isolated cases, life-threatening intraabdominal haemorrhage may occur.
Breast cancer
A meta-analysis from 54 epidemiological studies reported that there is a slightly increased relative risk (RR = 1.24) of having breast cancer diagnosed in women who are currently using COCs. The observed pattern of increased risk may be due to an earlier diagnosis of breast cancer in COC users, the biological effects of COCs or a combination of both. The additional breast cancers diagnosed in current users of COCs or in women who have used COCs in the last 10 years are more likely to be localised to the breast than those in women who never used COCs.
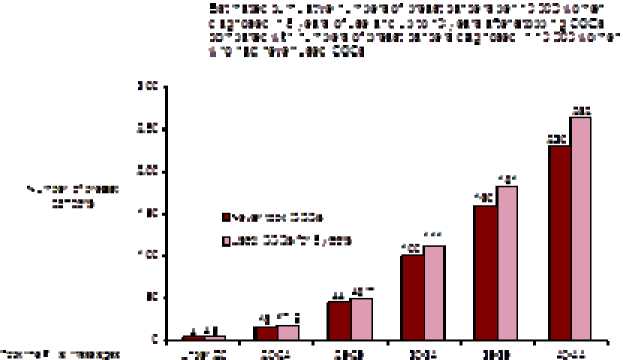
Breast cancer is rare among women under 40 years of age whether or not they take COCs. Whilst this background risk increases with age, the excess number of breast cancer diagnoses in current and recent COC users is small in relation to the overall risk of breast cancer (see bar chart).
The most important risk factor for breast cancer in COC users is the age women discontinue the COC; the older the age at stopping, the more breast cancers are diagnosed. Duration of use is less important and the excess risk gradually disappears during the course of the 10 years after stopping COC use such that by 10 years there appears to be no excess.
The possible increase in risk of breast cancer should be discussed with the user and weighed against the benefits of COCs taking into account the evidence that they offer substantial protection against the risk of developing certain other cancers (e.g. ovarian and endometrial cancer).
«*■ j ::: :i -i c u
Cervical cancer
The most important risk factor for cervical cancer is persistent Human Papilloma Virus (HPV) infection. Some epidemiological studies have indicated that long-term use of COCs may further contribute to this increased risk but there continues to be controversy about the extent to which this finding is attributable to confounding effects, e.g. cervical screening and sexual behaviour including use of barrier contraceptives.
There is some theoretical concern that COCs enhance progression of Cervical Intraepithelial Neoplasia (CIN) to invasive disease. For women with diagnosed cervical cancer, COCs may be used whilst awaiting treatment.
Other tumours
Numerous epidemiological studies have been reported on the risk of ovarian and endometrial cancer in women using COCs. The evidence is clear that COCs offer substantial protection against both ovarian and endometrial cancer.
Bleeding irregularities
Breakthrough bleeding, spotting and/or absence of withdrawal flow may be
encountered in patients on oral contraceptives, especially during the first three months of use.
If bleeding irregularities persist beyond three cycles or occur after previously regular cycles, non-hormonal causes should be considered and adequate diagnostic measures are indicated to exclude malignancy or pregnancy.
Some woman may experience post-Pill amenorrhoea or oligomenorrhoea, especially when such a condition was pre-existing.
Laboratory tests
In the literature, at least a hundred different laboratory test parameters have been reported to be possibly influenced by oral contraceptive use, predominantly by the oestrogenic component. Among these are: biochemical parameters of the liver, thyroid, adrenal and renal function, plasma levels of (carrier) proteins and lipid/lipoprotein fractions and parameters of coagulation and fibrinolysis.
Reduced efficacy
The efficacy of CHCs may be reduced in the event of missed tablets (section 4.2), vomiting (section 4.2) or concomitant medication (section 4.5).
Herbal preparations containing St John’s Wort (Hypericum perforatum) should not be used while taking Cilique due to the risk of decreased plasma concentrations and reduced clinical effects of Cilique (see Section 4.5 Interactions).
Other conditions
In the following conditions the benefit of oral contraception generally outweighs the theoretical or known risk. However, they may need to be considered before prescribing to individual patients:
• Known hyperlipidaemias. A small proportion of women will have persistent hypertriglyceridemia while on the pill. Changes in serum triglycerides, cholesterol and lipoprotein levels have been reported in users of oral contraceptives. However, routine screening of women with hypertriglyceridaemia is not considered appropriate. Women with hypertriglyceridaemia, or a family history thereof, may be at an increased risk of pancreatitis when using CHCs.
• Diabetes without vascular involvement (although all patients with diabetes are at increased risk of arterial disease).
• Oral contraceptives may cause a decrease in glucose tolerance. This effect has been
shown to be directly related to oestrogen dose. Additionally, progestogens may increase insulin secretion and create insulin resistance, this effect varies with different progestational agents. However, in the non-diabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, pre-diabetic and diabetic women in particular should
be carefully monitored while taking oral contraceptives.
• Asymptomatic gall bladder disease or cholecystectomy.
• Benign liver tumours (focal nodular hyperplasia). There is limited, direct evidence that hormonal contraceptive use does not influence either progression or regression of liver lesions among women with focal nodular hyperplasia.
• Migraine without focal aura. The onset or exacerbation of migraine or development of headache with a new pattern which is recurrent, persistent or severe requires discontinuation of oral contraceptives and evaluation of the cause.
• Crohn’s disease and ulcerative colitis have been associated with CHC use.
If any of the following conditions developed or worsened during a prior pregnancy or during previous COC use, they may occur while taking Cilique:
• elevated blood pressure
• cholestasis
• porphyria
• herpes gestationis
• otosclerosis
• SLE
• severe headaches
• haemolytic uraemic syndrome
• Sydenham’s chorea
Chloasma
Chloasma may occasionally occur, especially in women with a history of chloasma gravidarum. Women with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation while taking this preparation. Chloasma is often not fully reversible.
Additional contraceptive precautions
When additional contraceptive precautions are required, the patient should be advised either not to have sex, or to use a cap plus spermicide or for her partner to use a condom. Rhythm methods should not be advised as the Pill disrupts the usual cyclical changes associated with the natural menstrual cycle, eg changes in temperature and cervical mucus.
Excipients: The tablets contain lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
4.5 Interaction with other medicinal products and other forms of interaction
Changes in Contraceptive Effectiveness Associated With Co-administration
Drugs or herbal products that induce enzymes, including CYP3A4, that metabolise contraceptive hormones, may decrease the plasma concentrations of contraceptive hormones, and may decrease the effectiveness of hormonal contraceptives or increase breakthrough bleeding. Some drugs or herbal products that may decrease the effectiveness of hormonal contraceptives include:
• barbiturates
• bosentan
• carbamazepine
• eslicarbazepine acetate
• felbamate
• aprepitant and fosaprepitant
• griseofulvin
• some (combinations of) HIV protease inhibitors (e.g. nelfinavir, ritonavir, ritonavir-boosted protease inhibitors)
• some HCV protease inhibitors (e.g.boceprevir, telaprevir)
• modafinil
• some non-nucleoside reverse transcriptase inhibitors (e.g. nevirapine)
• oxcarbazepine
• phenytoin and fosphenytoin
• primidone
• rifampicin and rifabutin
• rufinamide
• St. John’s Wort
• topiramate
Drugs that affect absorption:
Drugs that increase gastrointestinal motility, e.g. metoclopramide, may reduce hormone absorption.
Treatment with activated charcoal will compromise absorption of steroid hormones.
Colesevelam:
Colesevelam, given together with a combined oral hormonal contraceptive, has been shown to significantly decrease the AUC of ethinyl estradiol. No interaction was seen when the contraceptive was given 4 hours before colesevelam.
Antibiotics:
There have been reports of pregnancy while taking hormonal contraceptives and antibiotics (e.g. ampicillin and tetracycline), but clinical pharmacokinetic studies have not shown consistent effects of antibiotics on plasma concentrations of synthetic steroids.
Women receiving short courses of any of the above-mentioned classes of drugs or individual drugs should take additional, non-hormonal (except rhythm or temperature method) contraceptive precautions during the time
of concurrent medication and for 7 days afterwards. If these 7 days overrun the end of the pack, the next pack should be started without a break. In this situation, a withdrawal bleed should not be expected until the end of the second pack. If the patient does not have a withdrawal bleed during the tablet-free interval following the end of the second pack, the possibility of pregnancy must be ruled out before resuming with the next pack. With rifampicin, additional contraceptive precautions should be continued for 4 weeks after treatment stops, even if only a short course was administered. With aprepitant and fosprepitant additional contraceptive precautions should be used during treatment and continued for 8 weeks after treatment stops.
Increase in Plasma Hormone Levels Associated With Co-Administered Drugs:
Some drugs and grapefruit juice may increase the plasma levels of ethinyl estradiol if co-administered. Examples include:
• paracetamol
• ascorbic acid
• etoricoxib
• CYP3A4 inhibitors (including itraconazole, ketoconazole, voriconazole, fluconazole and grapefruit juice)
• some HIV protease inhibitors (e.g. atazanavir, indinavir)
• HMG-CoA reductase inhibitors (including atorvastatin and rosuvastatin)
• some non-nucleoside reverse transcriptase inhibitors (e.g. etravirine)
Changes in Plasma Levels of Co-Administered Drugs:
Combination hormonal contraceptives may also affect the pharmacokinetics of some other drugs if used concomitantly.
Examples of drugs whose plasma levels may be increased (due to CYP inhibition) include:
• ciclosporin
• omeprazole
• prednisolone
• selegiline
• theophylline
• tizanidine
• voriconazole
Drugs whose plasma levels may be decreased (due to induction of glucuronidation).
Examples include:
• paracetamol
• clofibric acid
• lamotrigine (see below)
• morphine
• salicylic acid
• temazepam
Lamotrigine: Combined hormonal contraceptives have been shown to significantly decrease plasma concentrations of lamotrigine when coadministered due to induction of lamotrigine glucuronidation. This may reduce seizure control; therefore, dosage adjustments of lamotrigine may be necessary.
Physicians are advised to consult the labelling of concurrently-used drugs to obtain further information about interactions with hormonal contraceptives or the potential for enzyme alterations and the possible need to adjust dosages, advice regarding extra precautions and how long they must be used for.
Oral antidiabetics and insulin: The requirement for oral anti-diabetics or insulin can change as a result of the effect on glucose tolerance.
The use of oral contraceptives may influence the results of certain laboratory tests including biochemical parameters of liver, thyroid, adrenal, and renal function, plasma levels of carrier proteins and lipid/lipoprotein fractions, parameters of carbohydrate metabolism and parameters of coagulation and fibrinolysis. Laboratory staff should therefore be informed about oral contraceptive use when laboratory tests are requested.
Serum folate levels may be depressed by oral contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.
4.6 Fertility, pregnancy and lactation
Pregnancy
Cilique is not indicated during pregnancy.
If pregnancy occurs during medication with Cilique, the preparation should be withdrawn immediately.
Epidemiological studies indicate no increased risk of congenital anomalies in children born to women who used oral contraceptives prior to pregnancy. The majority of recent epidemiological studies also do not indicate a teratogenic effect, when taken inadvertently during early pregnancy.
The increased risk of VTE during the postpartum period should be considered when re-starting Cilique (see sections 4.2 and 4.4).
Breast-feeding
The use of Cilique during lactation may lead to a reduction in the volume of milk produced and to a change in its composition.
Minute amounts of the active substances are excreted with the milk.
If possible, the nursing mother should be advised not to use Cilique or other combination hormonal contraceptives but to use other
forms of contraception particularly in the first 6 weeks post-partum.
4.7 Effects on ability to drive and use machines
No effects on ability to drive and use machines have been observed.
4.8 Undesirable effects
Description of selected adverse reactions An increased risk of arterial and venous thrombotic and thromboembolic events, including myocardial infarction, stroke, transient ischemic attacks, venous thrombosis and pulmonary embolism has been observed in women using CHCs. These are discussed in more detail in section 4.4.
The safety of Cilique was evaluated in 1,891 healthy women of child bearing potential who participated in 5 clinical trials (2 randomized active-controlled trials and 3 uncontrolled open-label trials) and received at least 1 dose of Cilique for contraception. In 3 trials, subjects were followed for up to 24 cycles and in the other 2 trials, subjects were followed for up to 12 cycles. In these studies the following ADRs were solicited or determined from bleeding pattern or cycle characteristics data and the incidence could only be determined by treatment cycle (by cycle) and not overall: nausea, gastrointestinal disorder (reported as nausea or vomiting), vomiting, dysmenorrhoea, metrorrhagia, abnormal withdrawal bleeding, amenorrhoea, and diarrhoea (diarrhoea was identified as an ADR during post-marketing review). An additional uncontrolled study (N=8,331) reported ADRs by cycle only and was only included in the incidence calculation for the bycycle ADRs. For these by cycle ADRs, the pooled incidences for cycles 1,
3, 6, 12 and 24 were calculated and the highest cycle incidence (cycle 1 for all except vomiting and diarrhoea) presented and used to assign the ADR to a frequency category.
Based on pooled safety data from these clinical trials, the most commonly reported (i.e., >5% incidence) ADRs (with % incidence) were headache (27.9%), vaginal infection (7.5%), genital discharge (6.0%) and breast pain (5.7%). All by- cycle ADRs, except amenorrhoea, were very common (>10%) in cycle 1 (dysmenorrhoea: 40.4%; nausea: 29.1%; metrorrhagia: 26.3%; gastrointestinal disorder [reported as nausea or vomiting]: 24.6%; abnormal withdrawal bleeding: 16.9% and vomiting: 7.0%). With the exception of vomiting and dysmenorrhoea, the incidence of these ADRs was highest in cycle 1 and decreased over time with further treatment cycles (based on incidence data from cycles 1, 3, 6, 12 and 24). Vomiting increased in some later cycles, whereas dysmenorrhoea remained relatively stable, with a slight decrease over time.
The most commonly reported ( >5% incidence) ADRs identified during post marketing experience with norgestimate and ethinyl estradiol tablets ( incidence from pooled clinical trial data) were diarrhoea (11.8%) and back
pain* (5.4%)
*This calculated incidence value may be slightly higher than the actual incidence, as more than 1 event term reported in the same trial coded to the MedDRA preferred term of ‘Back pain’. It is possible that the same subject(s) may have reported more than 1 of the event terms and may therefore be counted more than once for the Preferred Term of ‘Back pain’.
The clinical trial incidence of diarrhoea was reported by cycle, therefore assignment of frequency category was based on the highest cycle incidence (cycle 12). Including the above-mentioned ADRs, Table A displays all ADRs that have been reported with the use of Cilique in clinical trials or from post marketing experiences with norgestimate and ethinyl estradiol tablets.
The displayed frequency categories use the following convention: Very common (>1/10); common (>1/100 to <1/10); uncommon (>1/1,000 to <1/100); rare (>1/10,000 to <1/1,000); very rare (<1/10,000); and not known (cannot be estimated from the available data).
Table: Adverse Drug Reactions
|
Infections and infestations | |
|
Common |
Urinary tract infection, vaginal infection |
|
Neoplasms benign, malignant and unspecified (including cysts and polyps) | |
|
Uncommon |
Cervical dysplasia |
|
Rare |
Breast cyst |
|
Frequency not known |
Breast cancer, Hepatic adenomas, Benign breast neoplasm, Focal nodular hyperplasia, Fibroadenoma of breast, Hepatic tumours |
|
Immune system disorders | |
|
Common |
Hypersensitivity |
|
Metabolism and nutrition disorders | |
|
Common |
Fluid retention, Weight increased |
|
Uncommon |
Weight fluctuation, Weight decreased, Increased appetite, Decreased appetite |
|
Rare |
Appetite disorder |
|
Frequency not known |
Dyslipidaemia |
|
Psychiatric disorders | |
|
Common |
Mood altered, depression, nervousness, insomnia |
|
Uncommon |
Anxiety, libido disorder |
|
Nervous system disorders | |
|
Very common |
Headache |
|
Common |
Migraine, dizziness |
|
Uncommon |
Syncope, paraesthesia |
|
Frequency not known |
Cerebrovascular accident, convulsion |
|
Eye disorders | |
|
Uncommon |
Visual impairment, dry eye |
|
Frequency not known |
Contact lenses intolerance, retinal vascular thrombosis* |
|
Ear and labyrinth disorders | |
|
Rare |
Vertigo |
|
Cardiac disorders | |
|
Uncommon |
Palpitations |
|
Rare |
Tachycardia |
|
Frequency not known |
Myocardial infarction |
|
Vascular disorders | |
|
Uncommon |
Thrombosis, hypertension, hot flush |
|
Rare |
Venous thromboembolism, Arterial thromboembolism |
|
Frequency not known |
Deep venous thrombosis* |
|
Respiratory, thoracic and mediastinal disorders | |
|
Uncommon |
Dyspnoea |
|
Frequency not known |
Pulmonary embolism* |
|
Gastrointestinal disorders | |
|
Very common |
Gastrointestinal disorder, Vomiting, Diarrhoea, Nausea |
|
Common |
Gastrointestinal pain, Abdominal pain, Abdominal distension, Constipation, Flatulence |
|
Rare |
Pancreatitis |
|
Hepato-biliary disorders | |
|
Rare |
Hepatitis |
|
Frequency not known |
Cholestatic jaundice |
|
Skin and subcutaneous tissue disorders | |
|
Common |
Acne, rash |
|
Uncommon |
Alopecia, Hirsutism, Urticaria, Pruritus, Erythema, Skin discolouration |
|
Rare |
Hyperhidrosis, Photosensitivity reaction |
|
Frequency not known |
Angioedema, Erythema nodosum, Night sweats |
|
Musculoskeletal and connective tissue disorders | |
|
Common |
Muscle spasms, Pain in extremity, Back pain |
|
Uncommon |
Myalgia |
|
Reproductive system and breast disorders | |
|
Very common |
Dysmenorrhoea, Metrorrhagia, Abnormal withdrawal bleeding |
|
Common |
Amenorrhoea, Genital discharge, Breast pain |
|
Uncommon |
Breast discharge, Galactorrhea, Breast enlargement, Ovarian cyst, Vulvovaginal dryness |
|
Rare |
Vaginal discharge |
|
Frequency not known |
Suppressed lactation |
|
General disorders and administration site conditions | |
|
Common |
Chest pain, Oedema, Asthenic conditions |
|
Investigations | |
|
Common |
Weight increased |
|
Uncommon |
Weight decreased |
* Not seen in clinical trials therefore frequency cannot be estimated. See section4.4 for frequency based on standard reporting rates for similar combined hormonal contraceptives.
Reporting of suspected adverse reactions in UK:
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at: www. mhra. gov.uk/yellowcard.
Reporting of suspected adverse reactions in Ireland:
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via HPRA Pharmacovigilance, Earlsfort Terrace, IRL -Dublin 2; Tel: +353 1 6764971; Fax: +353 1 6762517. Website: www.hpra.ie; E-mail: medsafety@hpra.ie. By reporting side effects you can help provide more information on the safety of this medicine.
4.9 Overdose
Overdosage may cause nausea, vomiting and, in young girls, withdrawal bleeding. Serious ill effects have not been reported following large doses of oral contraceptives in children. There are no antidotes and treatment should be symptomatic.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic Group: Hormonal Contraceptives for Systemic Use; Progestogens and estrogens, fixed combinations
ATC Code: G03AA11
Although the pharmacological actions of estrogens and progestogens which are present in all combined oral contraceptives are largely understood, the exact mechanism of their actions other than suppression of ovulation remains controversial.
Cilique acts through the mechanism of gonadotropin suppression by the estrogenic and progestational actions of ethinyl estradiol and norelgestromin. The primary mechanism of action is inhibition of ovulation, but alterations to the cervical mucus, the fallopian tube motility and to the endometrium may also contribute to the efficacy of the product.
Receptor and sex hormone binding globulin (SHBG) binding studies, as well as studies in animals and humans, have shown that both norgestimate (NGM) and norelgestromin, the major serum metabolite of norgestimate following oral administration, exhibits high progestational activity with minimal intrinsic androgenicity, which illustrates the selective action of Cilique. Norgestimate, in combination with ethinyl estradiol, does not counteract the estrogen-induced increases in SHBG, resulting in lower levels of free testosterone in serum compared to baseline.
When used perfectly, without missing any pills, the chance of becoming pregnant is less than 1% (i.e. <1 pregnancy per 100 women in their first year of use). Typical failure rates are actually 5% in the first year. The chance of becoming pregnant increases with each missed pill during a menstrual cycle.
5.2 Pharmacokinetic properties Absorption:
Norgestimate and ethinyl estradiol are rapidly absorbed following oral administration. Following single or multiple (three cycles) administration of Cilique, serum concentrations of norgestimate remain below the quantitation limit of the assay (0.1 ng/mL) due to rapid metabolism (see Metabolism below). Its metabolites, norelgestromin and norgestrel, are found in measurable concentrations in circulation, reaching maximal serum levels approximately 1.5 hours post-dose. Exposure to norelgestromin is proportional to dose following norgestimate doses of 0.180 to 0.250 mg. Ethinyl estradiol serum concentrations are measurable within 0.5 hours of dosing, reaching peak levels approximately 1.2 hours post-dose.
Distribution:
Norelgestromin and norgestrel are highly bound (>97%) to serum proteins. norelgestromin is bound to albumin but not to SHBG, while norgestrel is bound primarily to SHBG and to a much lesser extent to albumin. Ethinyl estradiol is extensively bound to serum albumin.
Studies have shown that the lack of binding of norelgestromin to SHBG is unique when compared to other progestogens in oral contraceptives and plays a key role in enhancing its biological activity.
In contrast, norgestrel formed from norgestimate is largely bound to SHBG, which limits its biologic activity.
These findings together with the selectivity of norelgestromin for the progesterone receptor indicate that this metabolite may explain the unique clinical profile of norgestimate.
Metabolism:
Norgestimate is rapidly metabolized by first-pass (intestinal and/or hepatic) mechanisms to norelgestromin (peak serum concentrations observed within 2 hours) and norgestrel, both of which are pharmacologically active progestogens. Ethinyl estradiol is metabolized to various hydroxylated metabolites and their glucuronide and sulfate conjugates.
Elimination:
Both norelgestromin and norgestrel, and ethinyl estradiol are subsequently metabolized and their metabolites are eliminated by renal and fecal pathways. Elimination half-life values at steady-state were 10 to 15 hours for ethinyl estradiol, 24.9 hours for norelgestromin and 45 hours for
norgestrel. Following administration of 14C- norgestimate, 47% of the administered radioactivity was eliminated in the urine and 37% in the faeces.
Steady-State Pharmacokinetics:
Following administration of 0.250 mg /0.035 mg ethinyl estradiol, the daily exposure (mean AUC0-24h) at steady-state, based on non-SHBG
bound serum levels, was 18.1 h ng/mL for norelgestromin and 3.64 h ng/mL for norgestrel. Following oral administration of 0.150 mg levonorgestrel/0.030 mg ethinyl estradiol, mean daily exposure at steady-state, based on non-SHBG bound serum levels, was 18.9 h ng/mL for norgestrel. The exposure to norgestrel following administration of 0.250 mg /0.035 mg ethinyl estradiol, corresponds to the exposure after a levonorgestrel dose of approximately 30 micrograms in combination with ethinyl estradiol.
5.3 Preclinical safety data
A comprehensive set of toxicity studies have been conducted on each of the components individually and in combination. These studies include single dose studies in multiple species, repeated dose studies up to two years in the rat, seven years in the dog and ten years in the monkey, reproductive and developmental toxicity, and genetic toxicity.
Results show that the acute oral LD50 of norgestimate (NGM) plus ethinyl estradiol (EE) in rats is greater than 5g/kg, indicating a very low order of acute toxicity and a wide margin of safety. Repeated dose studies in general laboratory animals (rats, dogs, monkeys), at NGM + EE ratios of up to 10:1 in subchronic (3-month studies, at doses of ~ 1000 times the clinical dose) and ratios of up to 5:1 in chronic (2-year studies, at doses of ~ 100 times the clinical dose) studies, showed somewhat similar results, such as reduction of estrus cycles or menstruation, decreased uterine and ovarian weights, increased liver and pituitary weights, decreased serum cholesterol levels and erythrocytic parameters, with most of the primary treatment related effects judged to be due to an exaggerated pharmacology action of NGM + EE, or general ageing phenomenon.
In long-term studies, increased incidence of mammary neoplasm's and lenticular opacities in rats (2-year study at doses up to 600 times the clinical dose) was considered a high dose effect and probably not relevant at optimally pharmacological dose levels. In the 7-year dog study, at doses up to 25 times the clinical dose, leiomyomas (fibroids) were observed at a slightly greater incidence in the high-dose group. These tumours are the most frequent occurring spontaneous neoplasm's of the reproductive tract in female dogs and are apparently due to estrogen overloading and are unlikely to occur at optimally pharmacological doses. A non-dose related lenticular opacities were also observed in the 7-year dog study. Although lenticular opacities is a normal observation in dogs, it generally has a longer latency period. Neoplasm's observed in the 10-year monkey study (at doses up to 50 times the clinical dose), are single occurrences and generally in different organs, with similar spontaneous occurrences being reported in the scientific literature.
In reproduction studies, noted, dose related effects on fertility, maternal and fetal parameters, and lactation are expected responses to the pharmacological actions of this class of anti-fertility compounds and were observed at dose levels within the pharmacodynamic range. Embryolethality and skeletal variations in rats was observed with no increase in extragenital anomalies. NGM + EE is not considered a teratogen. NGM + EE, NGM and its primary metabolite norelgestromin (NGMN), have shown no indication of any mutagenic potential.
In conclusion, the combination of norgestimate (NGM) and ethinyl estradiol (EE) in laboratory animals has shown some preclinical effects, which were observed at exposures considered sufficiently in excess of the maximum human exposure, or were the result of normal ageing process or from an exaggeration of pharmacological effects at higher than therapeutic doses indicating little relevance to clinical use.
Environmental Risk Assessment (ERA): Both actives substances are persistent in
environment and the environmental risk is not excluded (see section 6.6)
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Maize Starch Lactose
Magnesium Stearate (E470b)
Indigo Carmine (E132)
6.3
6.4
Special precautions for storage Do not store above 25°C.
Store in the original packaging to protect from light.
6.5
Nature and contents of container
Cartons containing 3 or 6 PVC/PVDC/Al blister strips of 21 tablets each. Not all pack sizes may be marketed.
Special precautions for disposal
Any unused medicinal product or waste material should be disposed of in accordance with the local requirements.
7
MARKETING AUTHORISATION HOLDER
Consilient Health Limited,
5th Floor, Beaux Lane House,
Mercer Street Lower,
Dublin 2, Ireland
8
23/11/2015
10
DATE OF REVISION OF THE TEXT
23/11/2015