Clexane 20mg/0.2ml Syringe
Out of date information, search anotherPOM
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Clexane.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you loose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Clexane. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Clexane might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Clexane.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Clexane
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Clexane contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Clexane only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Clexane looks like and contant of the pack
Clexane are type 1 glass pre-filled syringes fitted with injection needles. Clexane comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Clexane is manufactured by Sanofi Winthrop Industrie, 180 rue Jeans jaures, 94702 Maisons Alfort, France and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Clexane 20mg/0.2ml Syringe/ Clexane 40mg/0.4ml Syringe/ Clexane 60mg/0.6ml Syringe/ Clexane 80mg/0.8ml Syringe/ Clexane 100mg/1ml Syringe
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Clexane is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more likely to break
• Headache
• Hair loss
Clexane is a registered trademark of Aventis Pharma SA.
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Ref: 0742/160315/1/F
Clexane® 20mg/0.2ml Syringe/ Clexane®40mg/0.4ml Syringe/ Clexane® 60mg/0.6ml Syringe/Clexane® 80mg/0.8ml Syringe/
Clexane®100mg/1ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Clexane is and what it is used for Q Before you use Clexane Q How to use Clexane Q Possible side-effects Q How to store and dispose of Clexane Q Further information
O What Clexane is and what it is used for
The name of your medicine is either Clexane 20mg/0.2ml Syringe/ Clexane 40mg/0.4ml Syringe/ Clexane 60mg/0.6ml Syringe/ Clexane 80mg/0.8ml Syringe/ Clexane 100mg/1ml Syringe (called Clexane in this leaflet). Clexane contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Clexane works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Clexane can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Clexane
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Clexane (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Clexane.
Take special care with Clexane
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Clexane.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Clexane can affect the way some other medicines work. Also some medicines can affect the way Clexane works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• Warfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Clexane
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Clexane is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Clexane. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Clexane. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
[m How to use Clexane Having this medicine
• Before you use Clexane your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Clexane. This is because it needs to be given as an injection
• When you go home you may need to continue to use Clexane and give it to yourself (see below instructions on how to do this)
• Clexane is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Clexane or have any questions about how much Clexane is being given to you, speak to your doctor, pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Clexane given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Clexane
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Clexane will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Clexane each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Clexane each day for 6 to 14 days
c) After you have had a heart attack
Clexane can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Clexane given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Clexane will be given as an injection into your vein (intravenous injection using Clexane Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Clexane as an injection under your skin (subcutaneous injection). The usual dose is 1mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Clexane given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Clexane under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Clexane given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Clexane, your doctor may decide to give an additional dose of Clexane before a PCI operation. This is by injection into your vein (intravenous using Clexane Multidose Vial or
60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Clexane is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1mg for every kilogram of your weight if necessary
How to give yourself an injection of Clexane
If you are able to give Clexane to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Clexane
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
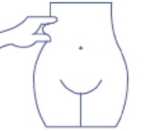
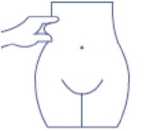
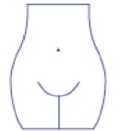
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Clexane should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Clexane:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
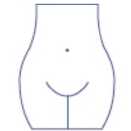
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Clexane syringe. Throw away the cap. The syringe is pre-filled and ready to use.
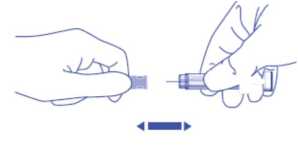
Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
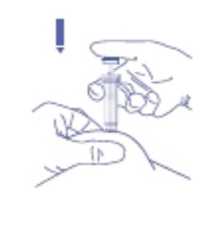
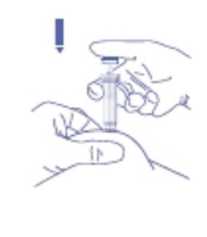
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin
Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
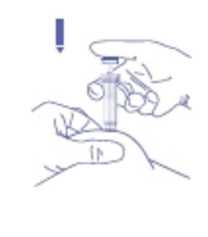
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Clexane than you should
If you think that you have used too much or too little Clexane, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Clexane, take them to a hospital casualty department straight away.
If you forget to use Clexane
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Clexane
It is important for you to keep having Clexane injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Clexane may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Clexane.
^ Possible side-effects
Like all medicines, Clexane can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Page 2
Ref:0742/160315/1/B
Page 3
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Lovenox.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you loose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Lovenox. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Lovenox might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Lovenox.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Lovenox is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more
likely to break
• Fleadache
• Hair loss
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.aov.uk/vellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Lovenox
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Lovenox contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Lovenox only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Lovenox looks like and contant of the pack
Lovenox are type 1 glass pre-filled syringes fitted with injection needles. Lovenox comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Lovenox is manufactured by Sanofi Winthrop Industrie, 180 rue Jeans jaures, 94702 Maisons Alfort, France and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe
Lovenox is a registered trademark of Aventis Pharma SA.
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Ref: 0742/160315/1/F
Lovenox® 20mg/0.2ml Syringe/ Lovenox®40mg/0.4ml Syringe/ Lovenox® 60mg/0.6ml Syringe/ Lovenox® 80mg/0.8ml Syringe/
Lovenox® 100mg/1 ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
^ What Lovenox is and what it is used for Q Before you use Lovenox Q How to use Lovenox Q Possible side-effects Q How to store and dispose of Lovenox Q Further information
Q What Lovenox is and what it is used for
The name of your medicine is either Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe (called Lovenox in this leaflet).
Lovenox contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Lovenox works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Lovenox can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Lovenox
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Lovenox (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Lovenox.
Take special care with Lovenox
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Lovenox.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Lovenox can affect the way some other medicines work. Also some medicines can affect the way Lovenox works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• VWrfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Lovenox
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Lovenox is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Lovenox. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Lovenox. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
How to use Lovenox
Having this medicine
• Before you use Lovenox your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Lovenox. This is because it needs to be given as an injection
• When you go home you may need to continue to use Lovenox and give it to yourself (see below instructions on how to do this)
• Lovenox is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Lovenox or have any questions
about how much Lovenox is being given to you, speak to your doctor,
pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Lovenox given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Lovenox
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Lovenox will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Lovenox each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Lovenox each day for 6 to 14 days
c) After you have had a heart attack Lovenox can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Lovenox given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Lovenox will be given as an injection into your vein (intravenous injection using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Lovenox as an injection under your skin (subcutaneous injection). The usual dose is 1 mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Lovenox given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Lovenox under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Lovenox given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Lovenox, your doctor may decide to give an additional dose of Lovenox before a PCI operation. This is by injection into your vein (intravenous using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Lovenox is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1 mg for every kilogram of your weight if necessary
How to give yourself an injection of Lovenox
If you are able to give Lovenox to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Lovenox
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Lovenox should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Lovenox:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
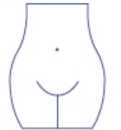
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Lovenox syringe. Throw away the cap. The syringe is pre-filled and ready to use.
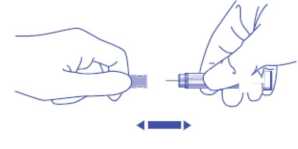
Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin
Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Lovenox than you should
If you think that you have used too much or too little Lovenox, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Lovenox, take them to a hospital casualty department straight away.
If you forget to use Lovenox
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Lovenox
It is important for you to keep having Lovenox injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Lovenox may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Lovenox.
ft Possible side-effects
Like all medicines, Lovenox can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Ref:0742/160315/1/B Page 3
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Enoxaparin sodium.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and noticed tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you loose control over your bladder or bowel
(so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Enoxaparin sodium. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Enoxaparin sodium might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unkown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Enoxaparin sodium.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Enoxaparin sodium is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your
bones are more likely to break
• Fleadache
• Hair loss
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Enoxaparin sodium
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
O Further information What Enoxaparin sodium contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Enoxaparin sodium only has water for injection as its other ingredient. Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Enoxaparin sodium looks like and contant of the pack
Enoxaparin sodium are type 1 glass pre-filled syringes fitted with injection needles. Enoxaparin sodium comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Enoxaparin sodium is manufactured by Sanofi Winthrop Industrie, 180 rue Jeans jaures, 94702 Maisons Alfort, France and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/ Enoxaparin sodium 100mg/1ml Syringe
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/
Enoxaparin sodium 100mg/1ml Syringe
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Enoxaparin sodium is and what it is used for Q Before you use Enoxaparin sodium Q Howto use Enoxaparin sodium Q Possible side-effects
Q How to store and dispose of Enoxaparin sodium Q Further information
Q What Enoxaparin sodium is and what it is used for
The name of your medicine is either Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/ Enoxaparin sodium 100mg/1ml Syringe (called Enoxaparin sodium in this leaflet). Enoxaparin sodium contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Enoxaparin sodium works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Enoxaparin sodium can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
Q Before you use Enoxaparin sodium
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Enoxaparin sodium (listed in Section 6: Further information) Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Enoxaparin sodium.
Take special care with Enoxaparin sodium
Check with your doctor or pharmacist or nurse before using this
medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Enoxaparin sodium.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Enoxaparin sodium can affect the way some other medicines work. Also some medicines can affect the way Enoxaparin sodium works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• VWrfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Enoxaparin sodium
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Enoxaparin sodium is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Enoxaparin sodium. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Enoxaparin sodium. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
Q How to use Enoxaparin sodium
Having this medicine
• Before you use Enoxaparin sodium your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Enoxaparin sodium. This is because it needs to be given as an injection
• When you go home you may need to continue to use Enoxaparin sodium and give it to yourself (see below instructions on how to do this)
• Enoxaparin sodium is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Enoxaparin sodium or have any
questions about how much Enoxaparin sodium is being given to you, speak
to your doctor, pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Enoxaparin sodium given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Enoxaparin sodium
1) Treating blood clots that are in your blood
• The usual dose is 1,5mg for every kilogram of your weight, each day
• Enoxaparin sodium will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Enoxaparin sodium will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Enoxaparin sodium each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Enoxaparin sodium each day for 6 to 14 days
c) After you have had a heart attack
Enoxaparin sodium can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Enoxaparin sodium given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Enoxaparin sodium will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Enoxaparin sodium will be given as an injection into your vein (intravenous injection using Enoxaparin sodium Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Enoxaparin sodium as an injection under your skin (subcutaneous injection). The usual dose is 1 mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Enoxaparin sodium given for the first two injections is 100mg
• The injections will normally be given for up to 8 days If you are aged 75 years or older
• Your doctor or nurse will give you injections of Enoxaparin sodium under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Enoxaparin sodium given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Enoxaparin sodium, your doctor may decide to give an additional dose of Enoxaparin sodium before a PCI operation. This is by injection into your vein (intravenous using Enoxaparin sodium Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Enoxaparin sodium is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1 mg for every kilogram of your weight if necessary
How to give yourself an injection of Enoxaparin sodium
If you are able to give Enoxaparin sodium to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Enoxaparin sodium
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Enoxaparin sodium should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Enoxaparin sodium:
1) Wash your hands and the area that you will inject with soap and water. Dry them.


2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
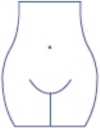
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Enoxaparin sodium syringe. Throw away the cap. The syringe is pre-filled and ready to use.

Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin

Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Enoxaparin sodium than you should
If you think that you have used too much or too little Enoxaparin sodium, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Enoxaparin sodium, take them to a hospital casualty department straight away.
If you forget to use Enoxaparin sodium
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Enoxaparin sodium
It is important for you to keep having Enoxaparin sodium injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Enoxaparin sodium may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Enoxaparin sodium.
O Possible side-effects
Like all medicines, Enoxaparin sodium can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Ref:0742/160315/1/B Page 3
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Clexane.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particulary in the lower part of your body. Also if you loose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Clexane. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Clexane might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Clexane.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Clexane is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more
likely to break
• Fleadache
• Hair loss
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Clexane
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Clexane contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Clexane only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Clexane looks like and contant of the pack
Clexane are type 1 glass pre-filled syringes fitted with injection needles. Clexane comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Clexane is manufactured by Sanofi-Aventis, S.AAvda. de Leganes, 62, 28925 Alcorcon-Madrid, Spain and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Clexane 20mg/0.2ml Syringe/ Clexane 40mg/0.4ml Syringe/ Clexane 60mg/0.6ml Syringe/ Clexane 80mg/0.8ml Syringe/ Clexane 100mg/1ml Syringe
Clexane is a registered trademark of Aventis Pharma SA.
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Ref: 0742/160315/2/F
Clexane® 20mg/0.2ml Syringe/ Clexane®40mg/0.4ml Syringe/ Clexane® 60mg/0.6ml Syringe/Clexane®80mg/0.8ml Syringe/
Clexane®100mg/1ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Clexane is and what it is used for Q Before you use Clexane Q How to use Clexane Q Possible side-effects Q How to store and dispose of Clexane Q Further information
O What Clexane is and what it is used for
The name of your medicine is either Clexane 20mg/0.2ml Syringe/ Clexane 40mg/0.4ml Syringe/ Clexane 60mg/0.6ml Syringe/ Clexane 80mg/0.8ml Syringe/ Clexane 100mg/1ml Syringe (called Clexane in this leaflet). Clexane contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Clexane works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Clexane can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Clexane
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Clexane (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Clexane.
Take special care with Clexane
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Clexane.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Clexane can affect the way some other medicines work. Also some medicines can affect the way Clexane works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• VWrfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Clexane
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Clexane is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Clexane. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Clexane. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
3 How to use Clexane
Having this medicine
• Before you use Clexane your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Clexane. This is because it needs to be given as an injection
• When you go home you may need to continue to use Clexane and give it to yourself (see below instructions on how to do this)
• Clexane is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Clexane or have any questions
about how much Clexane is being given to you, speak to your doctor,
pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Clexane given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Clexane
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Clexane will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Clexane each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Clexane each day for 6 to 14 days
c) After you have had a heart attack
Clexane can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Clexane given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Clexane will be given as an injection into your vein (intravenous injection using Clexane Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Clexane as an injection under your skin (subcutaneous injection). The usual dose is 1mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Clexane given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Clexane under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Clexane given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Clexane, your doctor may decide to give an additional dose of Clexane before a PCI operation. This is by injection into your vein (intravenous using Clexane Multidose Vial or
60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Clexane is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1mg for every kilogram of your weight if necessary
How to give yourself an injection of Clexane
If you are able to give Clexane to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Clexane
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Clexane should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Clexane:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Clexane syringe. Throw away the cap. The syringe is pre-filled and ready to use.
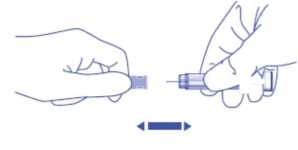
Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin

Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Clexane than you should
If you think that you have used too much or too little Clexane, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Clexane, take them to a hospital casualty department straight away.
If you forget to use Clexane
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Clexane
It is important for you to keep having Clexane injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Clexane may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Clexane.
Possible side-effects
Like all medicines, Clexane can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Page 2
Ref:0742/160315/2/B
Page 3
o
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Lovenox.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you loose control over yoour bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Lovenox. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Lovenox might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Lovenox.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Lovenox is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more likely to break
• Fleadache
• Hair loss
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
How to store and dispose of Lovenox
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Lovenox contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Lovenox only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Lovenox looks like and contant of the pack
Lovenox are type 1 glass pre-filled syringes fitted with injection needles. Lovenox comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Lovenox is manufactured by Sanofi-Aventis, S.AAvda. de Leganes, 62, 28925 Alcorcon-Madrid, Spain and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe
Lovenox is a registered trademark of Aventis Pharma SA.
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
n R ef: 0742/160315/2/F
Lovenox 20mg/0.2ml Syringe/ Lovenox®40mg/0.4ml Syringe/ Lovenox® 60mg/0.6ml Syringe/ Lovenox® 80mg/0.8ml Syringe/
Lovenox® 100mg/1ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Lovenox is and what it is used for Q Before you use Lovenox Q How to use Lovenox Q Possible side-effects Q How to store and dispose of Lovenox Q Further information
Q What Lovenox is and what it is used for
The name of your medicine is either Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe (called Lovenox in this leaflet).
Lovenox contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Lovenox works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Lovenox can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Lovenox
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Lovenox (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Lovenox.
Take special care with Lovenox
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Lovenox.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Lovenox can affect the way some other medicines work. Also some medicines can affect the way Lovenox works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• Warfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Lovenox
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Lovenox is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Lovenox. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Lovenox. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
3 How to use Lovenox
Having this medicine
• Before you use Lovenox your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Lovenox. This is because it needs to be given as an injection
• When you go home you may need to continue to use Lovenox and give it to yourself (see below instructions on how to do this)
• Lovenox is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Lovenox or have any questions
about how much Lovenox is being given to you, speak to your doctor,
pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Lovenox given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Lovenox
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Lovenox will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Lovenox each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Lovenox each day for 6 to 14 days
c) After you have had a heart attack
Lovenox can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Lovenox given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Lovenox will be given as an injection into your vein (intravenous injection using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Lovenox as an injection under your skin (subcutaneous injection). The usual dose is 1mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Lovenox given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Lovenox under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Lovenox given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Lovenox, your doctor may decide to give an additional dose of Lovenox before a PCI operation. This is by injection into your vein (intravenous using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Lovenox is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1mg for every kilogram of your weight if necessary
How to give yourself an injection of Lovenox
If you are able to give Lovenox to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Lovenox
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Lovenox should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Lovenox:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
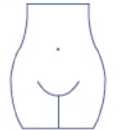
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Lovenox syringe. Throw away the cap. The syringe is pre-filled and ready to use.

Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin
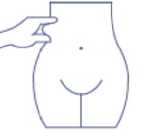
Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
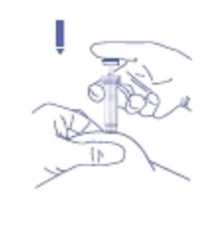
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Lovenox than you should
If you think that you have used too much or too little Lovenox, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Lovenox, take them to a hospital casualty department straight away.
If you forget to use Lovenox
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Lovenox
It is important for you to keep having Lovenox injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Lovenox may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Lovenox.
Possible side-effects
Like all medicines, Lovenox can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Page 2
Ref:0742/160315/2/B Page 3
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Enoxaparin sodium.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularlyin the lower part of your body. Also if you loose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Enoxaparin sodium. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Enoxaparin sodium might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Enoxaparin sodium.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www. m h ra. gov.uk/yellowca rd.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Enoxaparin sodium
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Enoxaparin sodium contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Enoxaparin sodium only has water for injection as its other ingredient. Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Enoxaparin sodium looks like and contant of the pack
Enoxaparin sodium are type 1 glass pre-filled syringes fitted with injection needles. Enoxaparin sodium comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Enoxaparin sodium is manufactured by Sanofi-Aventis, S.AAvda. de Leganes, 62, 28925 Alcorcon-Madrid, Spain and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/ Enoxaparin sodium 100mg/1ml Syringe
Revision date: 16/03/15
Frequency unknown
• If Enoxaparin sodium is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more likely to break
• Headache
• Hair loss
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/
Enoxaparin sodium 100mg/1ml Syringe
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Enoxaparin sodium is and what it is used for Q Before you use Enoxaparin sodium Q Howto use Enoxaparin sodium Q Possible side-effects
Q How to store and dispose of Enoxaparin sodium Q Further information
Q What Enoxaparin sodium is and what it is used for
The name of your medicine is either Enoxaparin sodium 20mg/0.2ml Syringe/ Enoxaparin sodium 40mg/0.4ml Syringe/ Enoxaparin sodium 60mg/0.6ml Syringe/ Enoxaparin sodium 80mg/0.8ml Syringe/ Enoxaparin sodium 100mg/1ml Syringe (called Enoxaparin sodium in this leaflet). Enoxaparin sodium contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Enoxaparin sodium works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Enoxaparin sodium can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
Q Before you use Enoxaparin sodium
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Enoxaparin sodium (listed in Section 6: Further information) Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Enoxaparin sodium.
Take special care with Enoxaparin sodium
Check with your doctor or pharmacist or nurse before using this
medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Enoxaparin sodium.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Enoxaparin sodium can affect the way some other medicines work. Also some medicines can affect the way Enoxaparin sodium works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• Warfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Enoxaparin sodium
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Enoxaparin sodium is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Enoxaparin sodium. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Enoxaparin sodium. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
^ How to use Enoxaparin sodium
Having this medicine
• Before you use Enoxaparin sodium your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Enoxaparin sodium. This is because it needs to be given as an injection
• When you go home you may need to continue to use Enoxaparin sodium and give it to yourself (see below instructions on how to do this)
• Enoxaparin sodium is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Enoxaparin sodium or have any
questions about how much Enoxaparin sodium is being given to you, speak
to your doctor, pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Enoxaparin sodium given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Enoxaparin sodium
1) Treating blood clots that are in your blood
• The usual dose is 1,5mg for every kilogram of your weight, each day
• Enoxaparin sodium will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Enoxaparin sodium will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Enoxaparin sodium each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Enoxaparin sodium each day for 6 to 14 days
c) After you have had a heart attack
Enoxaparin sodium can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Enoxaparin sodium given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Enoxaparin sodium will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Enoxaparin sodium will be given as an injection into your vein (intravenous injection using Enoxaparin sodium Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Enoxaparin sodium as an injection under your skin (subcutaneous injection). The usual dose is 1 mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Enoxaparin sodium given for the first two injections is 100mg
• The injections will normally be given for up to 8 days If you are aged 75 years or older
• Your doctor or nurse will give you injections of Enoxaparin sodium under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Enoxaparin sodium given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Enoxaparin sodium, your doctor may decide to give an additional dose of Enoxaparin sodium before a PCI operation. This is by injection into your vein (intravenous using Enoxaparin sodium Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Enoxaparin sodium is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1 mg for every kilogram of your weight if necessary
How to give yourself an injection of Enoxaparin sodium
If you are able to give Enoxaparin sodium to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Enoxaparin sodium
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Enoxaparin sodium should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Enoxaparin sodium:
1) Wash your hands and the area that you will inject with soap and water. Dry them.


2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
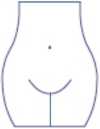
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Enoxaparin sodium syringe. Throw away the cap. The syringe is pre-filled and ready to use.

Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin

Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold
8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Enoxaparin sodium than you should
If you think that you have used too much or too little Enoxaparin sodium, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Enoxaparin sodium, take them to a hospital casualty department straight away.
If you forget to use Enoxaparin sodium
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Enoxaparin sodium
It is important for you to keep having Enoxaparin sodium injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Enoxaparin sodium may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Enoxaparin sodium.
Q Possible side-effects
Like all medicines, Enoxaparin sodium can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Page 3
Ref:0742/160315/2/B
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Clexane.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frequency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you lose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Clexane. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Clexane might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy, having pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be a liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Clexane.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Frequency unknown
• If Clexane is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more likely to break
• Fleadache
• Hair loss
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Clexane
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
Q Further information What Clexane contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Clexane only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Clexane looks like and contant of the pack
Clexane are type 1 glass pre-filled syringes fitted with injection needles. Clexane comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Clexane is manufactured by Sanofi Winthrop Industrie, Boulevard Industriel, Zone Industrielle 76580 Le Trait, France and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Clexane 20mg/0.2ml Syringe/
Clexane 40mg/0.4ml Syringe/
Clexane 60mg/0.6ml Syringe/
Clexane 80mg/0.8ml Syringe/
Clexane 100mg/1ml Syringe
Clexane is a registered trademark of Aventis Pharma SA.
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
Ref: 0742/160315/3/F
Clexane® 20mg/0.2ml Syringe/ Clexane®40mg/0.4ml Syringe/ Clexane® 60mg/0.6ml Syringe/Clexane®80mg/0.8ml Syringe/
Clexane®100mg/1ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Clexane is and what it is used for Q Before you use Clexane Q How to use Clexane Q Possible side-effects Q How to store and dispose of Clexane Q Further information
O What Clexane is and what it is used for
The name of your medicine is either Clexane 20mg/0.2ml Syringe/ Clexane 40mg/0.4ml Syringe/ Clexane 60mg/0.6ml Syringe/ Clexane 80mg/0.8ml Syringe/ Clexane 100mg/1ml Syringe (called Clexane in this leaflet). Clexane contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Clexane works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Clexane can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Clexane
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Clexane (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Clexane.
Take special care with Clexane
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Clexane.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Clexane can affect the way some other medicines work. Also some medicines can affect the way Clexane works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• VWrfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions.
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Clexane
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Clexane is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Clexane. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Clexane. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
How to use Clexane
Having this medicine
• Before you use Clexane your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Clexane. This is because it needs to be given as an injection
• When you go home you may need to continue to use Clexane and give it to yourself (see below instructions on how to do this)
• Clexane is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Clexane or have any questions
about how much Clexane is being given to you, speak to your doctor,
pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Clexane given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Clexane
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Clexane will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Clexane each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Clexane each day for 6 to 14 days
c) After you have had a heart attack
Clexane can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Clexane given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Clexane will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Clexane will be given as an injection into your vein (intravenous injection using Clexane Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Clexane as an injection under your skin (subcutaneous injection). The usual dose is 1mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Clexane given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Clexane under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Clexane given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Clexane, your doctor may decide to give an additional dose of Clexane before a PCI operation. This is by injection into your vein (intravenous using Clexane Multidose Vial or
60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Clexane is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1mg for every kilogram of your weight if necessary
How to give yourself an injection of Clexane
If you are able to give Clexane to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Clexane
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Clexane should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Clexane:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
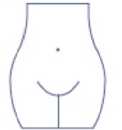
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Clexane syringe. Throw away the cap. The syringe is pre-filled and ready to use.
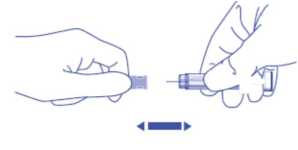
Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin

Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold

8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Clexane than you should
If you think that you have used too much or too little Clexane, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Clexane, take them to a hospital casualty department straight away.
If you forget to use Clexane
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Clexane
It is important for you to keep having Clexane injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Clexane may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Clexane.
Possible side-effects
Like all medicines, Clexane can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Ref:0742/160315/3/B
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots under the skin which do not go away when you put pressure on them. You may also notice pink patches on your skin. These are more likely to appear in the area you have been injected with Lovenox.
Uncommon (affects 1 to 10 people in a 1,000)
• Sudden severe headache. This could be a sign of bleeding in the brain.
• A feeling of tenderness and swelling in your stomach. You may have bleeding inside your stomach.
Rare (affects less than 1 in a 1000 people)
• If you have an allergic reaction. The signs may include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
Frquency unknown
• If you have had a spinal puncture or a spinal anaesthetic and notice tingling, numbness and muscular weakness, particularly in the lower part of your body. Also if you lose control over your bladder or bowel (so you cannot control when you go to the toilet).
Tell a nurse or doctor as soon as possible if you notice any of the
following side effects:
Common (affects 1 to 10 people in a 100)
• You bruise more easily than usual. This could be because of a blood problem (thrombocytopenia).
• You have pain, swelling or irritation in the area you have been injected with Lovenox. This normally gets better after a few days.
Rare (affects less than 1 in a 1000 people)
• If you have a mechanical heart valve, treatment with Lovenox might not be sufficient to prevent blood clots. You may notice that you have difficulty breathing, tiredness or difficulty exercising, chest pain, numbness, feeling sick or loss of consciousness. This could be due to a blood clot on the heart valve.
Frequency unknown
• Feeling tired, faint, dizzy havin pale skin. These could be symptoms of anaemia.
• You notice yellowing of your skin or eyes and your urine becomes darker in colour. This could be liver problem.
Other side effects that you should discuss with your nurse or doctor if
you are concerned about them:
Very common (affects more than 1 in 10 people)
• Changes in the results of blood tests done to check how your liver is working. These usually go back to normal after you stop having Lovenox.
Rare (affects less than 1 in a 1000 people)
• Changes in the potassium levels in your blood. This is more likely to happen in people with kidney problems or diabetes. Your doctor will be able to check this by carrying out a blood test.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.aov.uk/vellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
Q How to store and dispose of Lovenox
Do not use this medicine after the expiry date shown on the carton or syringe blister container. If your doctor tells you to stop taking this medicine, return any unused medicine to your pharmacist for safe disposal. Only keep this medicine, if your doctor tells you to. If your medicine becomes discoloured or shows any other signs of deterioration, consult your pharmacist who will tell you what to do.
• KEEP OUT OF THE SIGHT AND REACH OF CHILDREN.
• Do not store above 25°C.
• Do not refrigerate or freeze.
• Do not take the syringe out of the box until you need to use it.
O Further information What Lovenox contains
Each glass pre-filled syringe contains enoxaparin sodium as the active ingredient.
Lovenox only has water for injection as its other ingredient.
Each 0.2ml syringe contains 20mg enoxaparin sodium.
Each 0.4ml syringe contains 40mg enoxaparin sodium.
Each 0.6ml syringe contains 60mg enoxaparin sodium.
Each 0.8ml syringe contains 80mg enoxaparin sodium.
Each 1ml syringe contains 100mg enoxaparin sodium.
What Lovenox looks like and contant of the pack
Lovenox are type 1 glass pre-filled syringes fitted with injection needles. Lovenox comes in packs of 6 or 10 syringes.
Product Licence Holder and Manufacturer
Lovenox is manufactured by Sanofi Wlnthrop Industrie, Boulevard Industriel, Zone Industrielle 76580 Le Trait, France and is procured from within the EU and repackaged by the Product Licence Holder: Lexon (UK) Limited, Unit 18, Oxleasow Road, East Moons Moat, Redditch, Worcestershire, B98 ORE.
PL 15184/0742 Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe
Lovenox is a registered trademark of Aventis Pharma SA.
Frequency unknown
• If Lovenox is used for a long period of time (more than 3 months), it may increase the risk of you getting a condition called ‘osteoporosis’. This is when your bones are more likely to break
• Headache
• Hair loss
Revision date: 16/03/15
Blind or partially sighted?
Is this leaflet hard to see or read?
Phone Lexon (UK) Limited, Tel: 01527 505414 for help.
R ef: 0742/160315/3/F
Lovenox® 20mg/0.2ml Syringe/ Lovenox®40mg/0.4ml Syringe/ Lovenox® 60mg/0.6ml Syringe/ Lovenox® 80mg/0.8ml Syringe/
Lovenox® 100mg/1 ml Syringe
(enoxaparin sodium)
Patient Information Leaflet
Read all of this leaflet carefully before you start using this medicine
• Keep this leaflet. You may need to read it again
• If you have any further questions, ask your doctor or pharmacist
• This medicine has been prescribed for you. Do not pass it on to others.
It may harm them, even if their symptoms are the same as yours
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist
In this leaflet:
Q What Lovenox is and what it is used for Q Before you use Lovenox Q How to use Lovenox Q Possible side-effects Q How to store and dispose of Lovenox Q Further information
Q What Lovenox is and what it is used for
The name of your medicine is either Lovenox 20mg/0.2ml Syringe/ Lovenox 40mg/0.4ml Syringe/ Lovenox 60mg/0.6ml Syringe/ Lovenox 80mg/0.8ml Syringe/ Lovenox 100mg/1ml Syringe (called Lovenox in this leaflet).
Lovenox contains a medicine called enoxaparin sodium. This belongs to a group of medicines called Low Molecular Weight Heparins.
Lovenox works in two ways:
1) Stopping existing blood clots from getting any bigger. This helps your body to break them down and stop them causing you harm.
2) Stopping blood clots forming in your blood.
Lovenox can be used to:
• Treat blood clots that are in your blood
• Stop blood clots forming in your blood in the following situations:
• Unstable angina (where not enough blood gets to your heart)
• After an operation or long periods of bed rest due to illness
• After you have had a heart attack
• Stop blood clots forming in the tubes of your dialysis machine (used for people with kidney problems)
O Before you use Lovenox
Do not have this medicine and tell your doctor, pharmacist or nurse if:
• You are allergic (hypersensitive) to enoxaparin sodium or any of the other ingredients of Lovenox (listed in Section 6: Further information)
Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of your lips, face, throat or tongue
• You are allergic to heparin or other Low Molecular Weight Heparins such as tinzaparin or dalteparin
• You have a problem with bruising or bleeding too easily
• You have an ulcer in your stomach or gut (intestine)
• You have had a stroke caused by bleeding in the brain
• You have an infection in your heart
• You are using the medicine called heparin to treat blood clots
Do not have this medicine if any of the above apply to you. If you are not sure, talk to your doctor, pharmacist or nurse before having Lovenox.
Take special care with Lovenox
Check with your doctor or pharmacist or nurse before using this medicine if:
• You have high blood pressure
• You have kidney problems
• You have had a heart valve fitted
• You have ever had bruising and bleeding caused by the medicine ‘heparin’
• You have ever had a stroke
• You have ever had a stomach ulcer
• You have recently had an operation on your eyes or brain
• You are a diabetic or have an illness known as ‘diabetic retinopathy’ (problems with the blood vessels in the eye caused by diabetes)
• You have any problems with your blood
• You are underweight or overweight
• You are elderly (over 65 years old) and especially if you are aged over 75 years old
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist or nurse before using Lovenox.
Taking or using other medicines
Please tell your doctor, pharmacist or nurse if you are taking or have recently taken any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because Lovenox can affect the way some other medicines work. Also some medicines can affect the way Lovenox works.
In particular, do not have this medicine and tell your doctor if:
• You are using the medicine called heparin to treat blood clots
Tell your doctor if you are taking any of the following medicines:
• Warfarin - used for thinning the blood
• Aspirin, dipyridamole, clopidogrel or other medicines - used to stop blood clots forming
• Dextran injection - used as a blood replacer
• Ibuprofen, diclofenac, ketorolac or other medicines - used to treat pain and swelling in arthritis and other illnesses
• Prednisolone, dexamethasone or other medicines - used to treat asthma, rheumatoid arthritis and other conditions
• Water tablets (diuretics) such as spironolactone, triamterene or amiloride. These may increase the levels of potassium in your blood when taken with Lovenox
Your doctor may change one of your medicines or take regular blood tests to check that taking these medicines with Lovenox is not causing you any harm.
Operations and anaesthetics
If you are going to have a spinal puncture or an operation where an epidural or spinal anaesthetic is used, tell your doctor that you are using Lovenox. Tell also your doctor if you have any problem with your spine or if you have ever had spinal surgery.
You should not use this medicine if you are pregnant and have a mechanical heart valve as you may be at increased risk of developing blood clots. Your doctor should discuss this with you.
You should not breast-feed whilst using Lovenox. If you are planning to breast-feed, talk to your doctor, pharmacist or nurse. Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breast-feeding.
3 How to use Lovenox
Having this medicine
• Before you use Lovenox your doctor or nurse may carry out a blood test
• While you are in hospital your doctor or nurse will normally give you Lovenox. This is because it needs to be given as an injection
• When you go home you may need to continue to use Lovenox and give it to yourself (see below instructions on how to do this)
• Lovenox is usually given by injection underneath the skin (subcutaneous)
If you are not sure why you are receiving Lovenox or have any questions
about how much Lovenox is being given to you, speak to your doctor,
pharmacist or nurse.
How much will be given to you
• Your doctor will decide how much to give you. The amount of Lovenox given to you will depend on the reason it is being used
• If you have problems with your kidneys, you may be given a smaller amount of Lovenox
1) Treating blood clots that are in your blood
• The usual dose is 1.5mg for every kilogram of your weight, each day
• Lovenox will usually be given for at least 5 days
2) Stopping blood clots forming in your blood in the following situations:
a) Unstable angina
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
b) After an operation or long periods of bed rest due to illness
The usual dose is 20mg or 40mg each day. The dose will depend on how likely you are to develop a clot
• If you have a low to medium risk of getting a clot, you will be given 20mg of Lovenox each day. If you are going to have an operation, your first injection will usually be given 2 hours before your operation
• If you have a higher risk of getting a clot, you will be given 40mg each day. If you are going to have an operation, your first injection will usually be given 12 hours before your operation
• If you are bedridden due to illness, you will be normally be given 40mg of Lovenox each day for 6 to 14 days
c) After you have had a heart attack
Lovenox can be used for two different types of heart attack called NSTEMI or STEMI. The amount of Lovenox given to you will depend on your age and the kind of heart attack you have had.
i) NSTEMI type of heart attack
• The usual amount is 1mg for every kilogram of weight, every 12 hours
• Lovenox will usually be given for 2 to 8 days. Your doctor will normally ask you to take aspirin as well
ii) STEMI type of heart attack If you are under 75 years old
• 30mg of Lovenox will be given as an injection into your vein (intravenous injection using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
• At the same time, you will also be given Lovenox as an injection under your skin (subcutaneous injection). The usual dose is 1mg for every kilogram of your weight.
• Then you will be given 1mg for every kilogram of your weight every 12 hours after that
• The maximum amount of Lovenox given for the first two injections is 100mg
• The injections will normally be given for up to 8 days
If you are aged 75 years or older
• Your doctor or nurse will give you injections of Lovenox under your skin (subcutaneous injection)
• The usual dose is 0.75mg for every kilogram of your weight, every 12 hours
• The maximum amount of Lovenox given for the first two injections is 75mg
For patients having an operation called Percutaneous Coronary Intervention (PCI)
• Depending on when you were last given Lovenox, your doctor may decide to give an additional dose of Lovenox before a PCI operation. This is by injection into your vein (intravenous using Lovenox Multidose Vial or 60, 80 or 100mg Pre-filled syringes)
3) Stop blood clots forming in the tubes of your dialysis machine
• The usual dose is 1 mg for every kilogram of your weight
• Lovenox is added to the tube leaving the body (arterial line) at the start of the dialysis session
• This amount is usually enough for a 4 hour session. However, your doctor may give you a further dose of 0.5 to 1mg for every kilogram of your weight if necessary
How to give yourself an injection of Lovenox
If you are able to give Lovenox to yourself, your doctor or nurse will show you how to do this. Do not try to inject yourself if you have not been trained how to do so. If you are not sure what to do, talk to your doctor or nurse immediately.
Before injecting yourself with Lovenox
• Check the expiry date on the medicine. Do not use if the date has passed
• Check the syringe is not damaged and the medicine in it is a clear solution. If not, use another syringe
• Make sure you know how much you are going to inject
• Check your abdomen to see if the last injection caused any redness, change in skin colour, swelling, oozing or is still painful, if so talk to your doctor or nurse
• Decide where you are going to inject the medicine. Change the place where you inject each time from the right to the left side of your stomach. Lovenox should be injected just under the skin on your stomach, but not too near the belly button or any scar tissue (at least 5 cm away from these)
Instructions on injecting yourself with Lovenox:
1) Wash your hands and the area that you will inject with soap and water. Dry them.

2) Sit or lie in a comfortable position so you are relaxed. Make sure you can see the place you are going to inject. A lounge chair, recliner, or bed propped up with pillows is ideal.
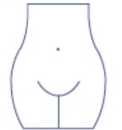
3) Choose an area on the right or left side of your stomach. This should be at least 5 centimetres away from your belly button and out towards your sides.
Remember: Do not inject yourself within 5 centimetres of your belly button or around existing scars or bruises. Change the place where you inject between the left and right sides of your stomach, depending on the area you were last injected.
4) Carefully pull off the needle cap from the Lovenox syringe. Throw away the cap. The syringe is pre-filled and ready to use.
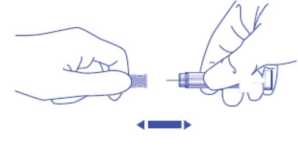
Do not press on the plunger before injecting yourself to get rid of air bubbles. This can lead to a loss of the medicine. Once you have removed the cap, do not allow the needle to touch anything. This is to make sure the needle stays clean (sterile).
5) Hold the syringe in the hand you write with (like a pencil) and with your other hand, gently pinch the cleaned area of your abdomen between your forefinger and thumb to make a fold in the skin

Make sure you hold the skin fold throughout the injection.
6) Hold the syringe so that the needle is pointing downwards (vertically at a 90° angle). Insert the full length of the needle into the skin fold

8) Remove the needle by pulling it straight out. You can now let go of the skin fold.
To avoid bruising, do not rub the injection site after you have injected yourself.
9) Drop the used syringe - needle first - into the sharps bin provided. Close the container lid tightly and place the container out of reach of children.
When the container is full, give it to your doctor or home care nurse for disposal. Do not put it in the household rubbish.
If you have more Lovenox than you should
If you think that you have used too much or too little Lovenox, tell your doctor, nurse or pharmacist immediately, even if you have no signs of a problem. If a child accidentally injects or swallows Lovenox, take them to a hospital casualty department straight away.
If you forget to use Lovenox
If you forget to give yourself a dose, have it as soon as you remember.
Do not give yourself a double dose on the same day to make up for a forgotten dose. Keeping a diary will help to make sure you do not miss a dose.
If you stop using Lovenox
It is important for you to keep having Lovenox injections until your doctor decides to stop them. If you stop, you could get a blood clot which can be very dangerous.
Blood Tests
Using Lovenox may affect the results of some blood tests. If you are going to have a blood test, it is important to tell your doctor you are having Lovenox.
Possible side-effects
Like all medicines, Lovenox can cause side effects, although not everybody gets them.
Tell a nurse or doctor or go to hospital straight away if you notice any of the following side-effects:
Very common (affects more than 1 in 10 people)
• Bleeding a lot from a wound.
Page 2
Ref:0742/160315/3/B Page 3
POM
Common (affects 1 to 10 people in a 100)
• A painful rash of dark red spots