Copralineb 0.5 Mg/2.5 Mg Per 2.5 Ml Nebuliser Solution
PACKAGE LEAFLET: INFORMATION FOR THE USER SZ00000LT000
Copralineb 0.5 mg/2.5 mg per 2.5 ml Nebuliser Solution
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, pharmacist or nurse.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1. What Copralineb is and what it is used for
2. What you need to know before you use Copralineb
3. How to use Copralineb
4. Possible side effects
5. How to store Copralineb
6. Contents of the pack and other information
Your medicine is called Copralineb. The active ingredients are ipratropium bromide and salbutamol. Ipratropium bromide and salbutamol both belong to a group of medicines called bronchodilators, which help to improve your breathing by opening up your airways. This is achieved by preventing the contraction of the smooth muscles surrounding the airways, therefore allowing the airways to remain open. Ipratropium bromide acts by blocking the nerve signals that go to the muscles surrounding the airways, and salbutamol acts by stimulating the beta2 receptors in the muscles.
Copralineb is used to treat breathing problems in people with long-standing breathing difficulties (such as chronic bronchitis, emphysema).
Copralineb will relieve wheezing, shortness of breath and chest tightness.
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
If you are going to have a general anaesthetic in hospital, please tell the anaesthetist what drugs you are taking.
Copralineb with food and drink
Food and drink have no influence on Copralineb.
Pregnancy and breast-feeding
Tell your doctor or pharmacist if you are pregnant, think you might be pregnant, are planning to become pregnant or are breast-feeding.
Copralineb should not be used during pregnancy or breast feeding unless your doctor decides that the benefits to the mother outweigh the risk to the baby.
Ask your doctor for advice before taking any medicine.
Driving and using machines
If you experience side effects such as dizziness, difficulty focusing and blurred vision during treatment with Copralineb you should avoid potentially hazardous tasks such as driving or operating machinery.
Do not use Copralineb if:
• you suffer from fast heart rhythms.
• you know that you have an enlarged heart or a condition known as hypertrophic obstructive cardiomyopathy or HOCM.
• you are allergic to salbutamol, ipratropium bromide or atropine (including drugs similar to atropine) or to any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor before using Copralineb if:
• you suffer from or think you may suffer from an eye condition known as glaucoma (increased pressure in the eyes) or if you suffer from any other eye conditions Your doctor may advise you to protect your eyes when using Copralineb.
• you know that you (if male) have an enlarged prostate or if you have problems passing urine (water).
• you have had a recent heart attack (myocardial infarction).
• you have problems with your arteries or get pain in your legs when you walk.
• you have a history of heart disease, irregular heart rhythm or angina (please tell your doctor before starting this medication).
• you have diabetes.
• you have an overactive thyroid gland.
• you suffer from cystic fibrosis.
• you have been told that you have a tumour of the adrenal gland.
Copralineb can cause tooth decay. Please pay attention to proper oral hygiene, particularly in children, and get your teeth checked regularly by your dentist.
Other medicines and Copralineb
Certain medicines may interact with Copralineb and may worsen side effects or reduce the effect of Copralineb.
You must always tell your doctor if you are taking any of the following medicines:
• other asthma medicines, including inhalers and tablets for asthma and including treatments known as “relievers” such as salbutamol and “preventers” such as beclometasone dipropionate. These may increase the effect of Copralineb and increase the severity of side effects.
• beta-blockers i.e. medicines that are commonly used to treat heart conditions such as chest pain that occurs on exertion (called angina pectoris), irregular heart beats or arrhythmias and high blood pressure (called hypertension).
They include drugs such as propranolol, which may cause blood potassium levels to fall when given at the same time as Copralineb.
• certain drugs to treat depression (such “anti-depressants” are drugs that are prescribed for patients suffering from depression and anxiety). This class of drug includes medicines such as monoamine oxidase inhibitors (e.g. phenelzine) or tricyclic antidepressants (e.g. amitriptyline).
• digoxin (for heart problems) may cause heart rhythm problems when given with Copralineb.
• diuretics (“water tablets”) can potentiate urinary blockade.
• steroid tablets (these are medicines that are used to reduce inflammatory processes within the body and include drugs such as prednisolone), which may increase the airway blockade.
• anaesthetic agents may increase the susceptibility of the effects of salbutamol on the heart - you will be monitored closely or your doctor might decide to discontinue Copralineb if you are going to have an operation.
Copralineb is for inhalation use. The nebuliser solution is for oral inhalation after nebulisation.
Always use this medicine exactly as your doctor has told you to. Check with your doctor (or the nurse if appropriate) if you are not sure.
The recommended dose for adults and children over 12 years of age is the contents of one ampoule, three or four times a day.
Elderly patients should take the usual adult dose.
Copralineb is not recommended for children under 12 years of age.
The label will tell you how much to take and how often to take it.
Never use more medicine than your doctor has told you to.
Tell your doctor if your breathing problems get worse or your medicine does not provide as much relief from your breathing problems as before or if you are using your blue short-acting “reliever” inhaler more often than is usual for you.
Copralineb should be used with a suitable nebuliser, e.g. PARI LC PLUS Nebuliser, jet nebulizer. Please read the full instructions for use of the nebuliser in the leaflet provided with PARI LC PLUS before starting the inhalation.
Instructions for use
• Prepare your nebuliser for use according to the manufacturer’s instructions and advice from your doctor.
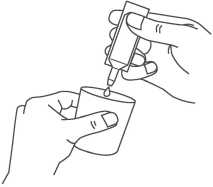
• Carefully remove an ampoule from the labelled strip by twisting and pulling. Never use an ampoule that has been opened already or if the nebuliser solution is discoloured (diagram A).
• Hold the ampoule upright and twist off the cap (diagram B).
• Squeeze the contents into the reservoir of your nebuliser (diagram C).



Continued on the next page >>
r
draft: 44052398

o ns
« E
Artwork Proof Box
Ref: V006 - TW corrective action, Safety update SPC & PIL + RFI
Proof no. Date prepared: Font size:
006.2 31/08/2016 9pt
Colours: Fonts:
■ Black □ Helvetica
□ □
Dimensions: 210 x 500 mm
o
draft: 44052398

« £
• Follow the manufacturer’s instructions and the advice from your doctor on how to assemble and how to use your nebuliser.
• After you have used your nebuliser, throw away any nebuliser solution that is left in the reservoir. Any nebuliser solution left in the ampoule should also be thrown away.
• Clean your nebuliser thoroughly according to the manufacturer’s instructions. It is important that the nebuliser is kept clean.
• memory disorders
• anxiety
• depression
• hyperactivity in children
• eye pain or other problems with the eyes including blurring of vision, mydriasis (the excessive dilation of the pupil of the eye) and glaucoma (increased pressure in the eyes).
Do not dilute the nebuliser solution or mix it with other medicines, Frequency not known but may also occur unless your doctor tells you to. • tooth decay.
The single dose ampoules of Copralineb do not contain preservatives and therefore it is important to use the contents immediately after opening. A new ampoule must be used each time you use Copralineb in your nebuliser.
Partly used, opened or damaged ampoules should be discarded. You should never use an ampoule, which has been opened earlier.
It is important that you follow these instructions in order to avoid any contamination of the nebuliser solution within the ampoules.
Do not swallow the nebuliser solution or use it in injections.
Do not allow the nebuliser solution or mist to enter your eyes.
If you use more Copralineb than you should
If you have taken a slightly larger dose than usual, you may notice a faster heart beat (palpitations) or tremor. Other symptoms might include chest pain, changes in blood pressure, flushing, restlessness or dizziness. These effects usually wear off in a few hours. The level of potassium in your blood may fall and the doctor may want to monitor the potassium in your blood by taking a blood test to measure the levels from time to time. Tell your doctor if you are worried by any of these symptoms or if they persist.
If you have taken more medicine than you should have taken, tell your doctor immediately or go to the nearest hospital. If you need to visit a doctor or need to go into hospital then you should take all of your medicines with you, including any you may have bought without a prescription; these should be in their original packaging if at all possible. Take this leaflet with you to show the doctor.
If you forget to use Copralineb
If you forget to take a dose at the right time, take it as soon as you remember. Do not take a double dose to make up for a forgotten dose.
If you stop using Copralineb
You should not stop taking Copralineb without prior discussion with your doctor.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Although it is not known exactly how often this happens, some people might experience chest pain (due to problems such as angina). Tell your doctor as soon as possible if you develop these symptoms whilst receiving treatment with Copralineb, but do not stop using this medicine unless told to do so.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist.
This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the yellow card scheme (Website: www.mhra.gov.uk/yellowcard). By reporting side effects you can help provide more information on the safety of this medicine.
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton and label after EXP. The expiry date refers to the last day of that month.
Do not refrigerate or freeze. Do not store above 25°C.
Keep the nebuliser solution in the outer pouch or carton in order to protect from light.
After first opening the pouch, the closed ampoule should be used within 3 months.
For single use only. Use immediately after first opening the ampoule. Discard immediately after first use.
Partly used, opened or damaged ampoules should be disposed in accordance with local requirements.
Do not use this medicine if you notice the nebuliser solution is cloudy.
Do no throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
Like all medicines, this medicine can cause side effects, although not everybody gets them. Some of the side-effects may be serious and require medical intervention.
Serious side effects
If your asthma or wheezing gets worse immediately after inhaling Copralineb, or your breathing becomes more difficult and you become short of breath do not take any more Copralineb but use your short-acting ‘reliever’ inhaler straightaway. You should stop using Copralineb and should contact your doctor immediately.
Your doctor may prescribe alternative treatment for your condition.
If you experience eye pain or eye discomfort, blurred vision or red eyes, or if you see halos or coloured spots then you should contact your doctor straightaway as treatment for these symptoms may be required.
If you think that you may be allergic to Copralineb or if you think you may be having an allergic reaction to the nebuliser solution then you should stop using Copralineb straightaway and contact your doctor immediately.
A reduction in the level of potassium (hypokalaemia) in the blood due to the salbutamol component of Copralineb can occur - and this may cause muscle weakness, twitching or abnormal heart rhythm. This is more likely to happen if you are taking Copralineb with some other asthma treatments, with inhaled steroids or steroid tablets or with diuretics ("water tablets”). Your doctor may need to take a blood test to measure your potassium levels from time to time.
What Copralineb contains
Each 2.5 ml Copralineb contains:
• The active substances are 0.5 mg of ipratropium bromide as 520 micrograms ipratropium bromide monohydrate and salbutamol 2.5 mg as sulphate.
• The other ingredients are sodium chloride, water for injection and sulfuric acid.
What Copralineb looks like and contents of the pack
The pack is a Plastic Form fill Seal (FFS) ampoule containing 2.5 ml of nebuliser solution, 5 of which are over wrapped in a triple laminated pouch and then packed into cardboard cartons containing 10, 20, 30, 40, 50, 60, 80, 100, 120 and 150 ampoules.
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer Marketing Authorisation Holder
Sandoz Ltd,
Frimley Business Park, Frimley,
Camberley, Surrey, GU16 7SR, UK.
Manufacturer
Lek Pharmaceuticals d.d,
Verovskova 57, 1526 Ljubljana,
Slovenia
or
Side effects can occur with the following frequencies: Common, affects 1 to 10 per 100 users
• headaches
• palpitations or rapid heartbeat
• dryness of the mouth
• nausea (feeling sick)
• coughing
• speech difficulties
• problems with blurred vision.
Uncommon, affects 1 to 10 per 1,000 users
• dizziness
• increased blood pressure
• abnormal or very fast heartbeat
• a feeling of nervousness
• vomiting (being sick)
• tremor
• difficulty in passing urine (water).
Rare, affects 1 to 10 per 10,000 users
• anaphylactic (allergic) reactions including swelling, which may affect the tongue, lips and face
• breathing difficulties and shortness of breath
• sweating
• flushing
• reduced blood pressure
• mouth and throat irritation
• upset stomach / upset bowels
• itching
• rashes
• muscular pains
• weakness and cramps
• restlessness
Salutas Pharma GmbH, Otto-von-Guericke-Allee 1,
39179 Barleben, Germany
or
Neolab Limited,
57 High Street, Odiham,
Hampshire, RG29 1LF, UK.
This leaflet was last revised in 08/2016.
00000000
SZ00000LT000
Artwork Proof Box
Ref: V006 - TW corrective action, Safety update SPC & PIL + RFI
|
Proof no. 006.2 |
Date prepared: 31/08/2016 |
Font size: 9pt | |
|
Colours: |
Fonts: | ||
|
| Black |
□ |
Helvetica | |
|
□ |
□ | ||
|
Dimensions: 210 x 500 |
mm | ||