Fentanyl 200 Microgram Compressed Lozenge With Integral Oromucosal Applicator
Out of date information, search anotherSUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Fentanyl 200 microgram compressed lozenge with integral oromucosal applicator
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
One lozenge contains 200 micrograms fentanyl (as citrate).
Excipient(s):
Each lozenge contains dextrates (equivalent to approximately 2 grams of glucose), sucrose (approximately 30 milligrams confectioner’s sugar) and propylene glycol (part of the artificial berry flavour and imprinting ink) as excipients.
For a full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Compressed lozenge with integral oromucosal applicator.
Fentanyl is formulated as a white to off-white compressed powder drug matrix attached using edible glue to a fracture resistant radio opaque plastic applicator, marked with the dosage strength.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Fentanyl is indicated for the management of breakthrough pain in patients already receiving maintenance opioid therapy for chronic cancer pain. Breakthrough pain is a transitory exacerbation of pain that occurs on a background of otherwise controlled persistent pain.
Patients receiving maintenance opioid therapy are those who are taking at least 60 mg of oral morphine daily, at least 25 micrograms of transdermal fentanyl per hour, at least 30 mg of oxycodone daily, at least 8 mg of oral hydromorphone daily or an equianalgesic dose of another opioid for a week or longer.
4.2 Posology and method of administration
In order to minimise the risks of opioid-related side-effects and to identify the “successful” dose, it is imperative that patients be monitored closely by health professionals during the titration process.
Fentanyl is not interchangeable on a mcg to mcg basis with other short-acting fentanyl products that are indicated for the use of breakthrough cancer pain, as the pharmacokinetic profiles and/or dosing schedules of these products are significantly different. Patients should be instructed not to use more than one short-acting fentanyl product concurrently for the treatment of breakthrough cancer pain, and to dispose of any fentanyl product prescribed for breakthrough pain (BTP) when switching to Fentanyl. The number of Fentanyl strengths available to the patient at any time should be minimised to prevent confusion and potential overdose.
Any unused Fentanyl units that the patient no longer requires must be disposed of properly. Patients must be reminded of the requirements to keep Fentanyl stored in a location away from children.
Method of administration
Fentanyl is intended for oromucosal administration, and therefore should be placed in the mouth against the cheek and should be moved around the mouth using the applicator, with the aim of maximising the amount of mucosal exposure to the product. The Fentanyl unit should be sucked, not chewed, as absorption of fentanyl via the buccal mucosa is rapid in comparison with systemic absorption via the gastrointestinal tract. Water may be used to moisten the buccal mucosa in patients with a dry mouth.
The Fentanyl unit should be consumed over a 15 minute period. If signs of excessive opioid effects appear before the Fentanyl unit is fully consumed it should be immediately removed, and consideration given to decreasing future dosages.
Adults
Dose titration and maintenance therapy
Fentanyl should be individually titrated to a “successful” dose that provides adequate analgesia and minimises side effects. In clinical trials the successful dose of Fentanyl for breakthrough pain was not predicted from the daily maintenance dose of opioid.
a) Titration
Before patients are titrated with Fentanyl, it is expected that their background persistent pain will be controlled by use of opioid therapy and that they are typically experiencing no more than 4 episodes of breakthrough pain per day.
The initial dose of Fentanyl used should be 200 micrograms, titrating upwards as necessary through the range of available dosage strengths (200, 400, 600, 800, 1200 and 1600 micrograms). Patients should be carefully monitored until a dose is reached that provides adequate analgesia with acceptable side effects using a single dosage unit per episode of breakthrough pain. This is defined as the successful dose.
During titration, if adequate analgesia is not obtained within 30 minutes after starting the first unit (i.e. 15 minutes after the patient completes consumption of a single Fentanyl unit), a second Fentanyl unit of the same strength may be consumed. No more than two Fentanyl units should be used to treat any individual pain episode. At 1600 micrograms, a second dose is only likely to be required by a minority of patients.
If treatment of consecutive breakthrough pain episodes requires more than one dosage unit per episode, an increase in dose to the next higher available strength should be considered.
Fentanyl
® Titration Process
b) Maintenance
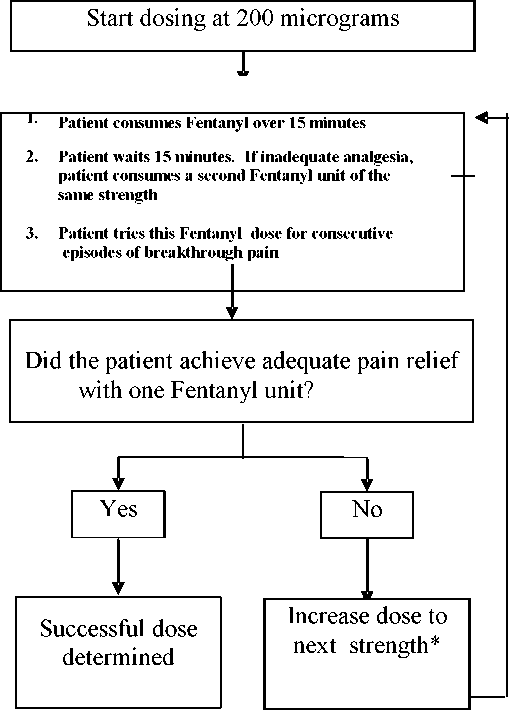
*Available dosage strengths include: 200, 400, 600, 800, 1200 and 1600 micrograms
Once a successful dose has been established (i.e., on average, an episode is effectively treated with a single unit), patients should be maintained on this dose and should limit consumption to a maximum of four Fentanyl units per day.
Patients should be monitored by a health professional to ensure that the maximum consumption of four units of Fentanyl per day is not exceeded.
Dose re-adjustment
The maintenance dose of Fentanyl should be increased when an episode is not effectively treated with a single unit for several consecutive BTP episodes. For dose-readjustment the same principles apply as outlined for dose titration (see above).
If more than four episodes of breakthrough pain are experienced per day the dose of the long acting opioid used for persistent pain should be re-evaluated. If the dose of the long acting opioid is increased, the dose of Fentanyl to treat breakthrough pain may need to be reviewed.
It is imperative that any dose re-titration of any analgesic is monitored by a health professional.
Discontinuation of therapy
Fentanyl therapy may usually be immediately discontinued if no longer required for breakthrough pain, only in patients who continue to take their chronic opioid therapy for persistent pain.
For patients requiring discontinuation of all opioid therapy, account should be taken of the Fentanyl dose in consideration of a gradual downward opioid titration to avoid the possibility of abrupt withdrawal effects.
Use in the elderly
Elderly patients have been shown to be more sensitive to the effects of fentanyl when administered intravenously. Therefore dose titration needs to be approached with particular care. In the elderly, elimination of fentanyl is slower and the terminal elimination half-life is longer, which may result in accumulation of the active substance and to a greater risk of undesirable effects.
Formal clinical trials with Fentanyl have not been conducted in the elderly. It has been observed, however, in clinical trials that patients over 65 years of age required lower doses of Fentanyl for successful relief of breakthrough pain.
Use in patients with hepatic or renal impairment
Special care should be taken during the titration process in patients with kidney or liver dysfunction (see section 4.4).
Paediatric population
Children aged 16 years and above: follow adult dosage
Children aged 2 to 16 years old:
There is limited clinical trial experience of the use of Fentanyl in paediatric patients already receiving maintenance opioid therapy (see sections 5.1 and 5.2). Safety and efficacy in paediatric patients below the age of 16 years have not been established; use in this patient population is therefore not recommended.
4.3 Contraindications
Hypersensitivity to fentanyl or to any of the excipients.
Patients without maintenance opioid therapy (see section 4.1) as there is an increased risk of respiratory depression.
Treatment of acute pain other than breakthrough pain (e.g. postoperative pain, headache, migraine).
Simultaneous use of monoamine-oxidase (MAO) inhibitors, or within 2 weeks after the cessation of the use of MAO inhibitors.
Severe respiratory depression or severe obstructive lung conditions.
4.4 Special warnings and precautions for use
Patients and their carers must be instructed that Fentanyl contains an active substance in an amount that can be fatal to a child. Death has been reported in children who have accidentally ingested Fentanyl.
Patients and their carers must be instructed to keep all units out of the reach and sight of children and to discard open and unopened units appropriately. An evaluation of each out-patient concerning possible accidental child exposures should be undertaken.
The product should not be given to patients without maintenance opioid therapy as there is an increased risk of respiratory depression and death. It is important that the maintenance opioid therapy used to treat the patient’s persistent pain has been stabilised before Fentanyl therapy begins and that the patient continues to be treated with the maintenance opioid therapy whilst taking Fentanyl.
Like for all opioids, tolerance, physical and/or psychological dependence and abuse of fentanyl may occur. However, iatrogenic addiction following therapeutic use of opioids is rare. The risk is considered low in cancer patients with breakthrough pain, but may be higher in those patients with a history of substance abuse and alcohol dependence.
All patients treated with opioids require careful monitoring for signs of abuse and addiction.
As with all opioids, there is a risk of clinically significant respiratory depression associated with the use of Fentanyl. Particular caution should be used when titrating Fentanyl in patients with non-severe chronic obstructive pulmonary disease or other medical conditions predisposing them to respiratory depression, as even normally therapeutic doses of Fentanyl may further decrease respiratory drive to the point of respiratory failure.
Fentanyl should only be administered with extreme caution in patients who may be particularly susceptible to the intracranial effects of CO2 retention, such as those with evidence of increased intracranial pressure, or impaired consciousness. Opioids may obscure the clinical course of a patient with a head injury and should be used only if clinically warranted.
Intravenous fentanyl may produce bradycardia. Therefore, Fentanyl should be used with caution in patients with bradyarrhythmias.
In addition, Fentanyl should be administered with caution to patients with liver or kidney dysfunction. The influence of liver and renal impairment on the pharmacokinetics of the medicinal product has not been evaluated, however, when administered intravenously the clearance of fentanyl has been shown to be altered in hepatic and renal disease due to alterations in metabolic clearance and plasma proteins. After administration of Fentanyl, impaired liver and renal function may both increase the bioavailability of swallowed fentanyl and decrease its systemic clearance, which could lead to increased and prolonged opioid effects. Therefore, special care should be taken during the titration process in patients with moderate or severe hepatic or renal disease.
Careful consideration should be given to patients with hypovolaemia and hypotension.
Diabetic patients should be advised that the medicine product contains dextrates (dextrates are composed of 93% dextrose monohydrate and 7% maltodextrin. The total glucose load per dosage unit is approximately 1.89 grams per dose).
Patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine.
Normal oral hygiene is recommended to reduce any potential harm to the teeth. Because Fentanyl contains approximately 2 grams of sugar, frequent consumption increases the risk of dental decay. The occurrence of dry mouth associated with the use of opioid medications may add to this risk.
4.5 Interaction with other medicinal products and other forms of interaction
Fentanyl is metabolized by the CYP3A4 isoenzyme in the liver and intestinal mucosa. Potent inhibitors of CYP3A4 such as macrolide antibiotics (e.g. erythromycin), azole antifungals (e.g. ketoconazole, itraconazole, and fluconazole) and certain protease inhibitors (e.g. ritonavir), may increase the bioavailability of swallowed fentanyl and may also decrease its systemic clearance which may result in increased or prolonged opioid effects. Similar effects could be seen after concurrent ingestion of grapefruit juice, which is known to inhibit CYP3A4. Hence caution is advised if fentanyl is given concomitantly with CYP3A4 inhibitors.
Coadministration with agents that induce 3A4 activity may reduce the efficacy of Fentanyl.
The concomitant use of other CNS depressants, including other opioids, sedatives or hypnotics, general anaesthetics, phenothiazines, tranquillisers, skeletal muscle relaxants, sedating antihistamines and alcohol may produce additive depressant effects.
Withdrawal symptoms may be precipitated through the administration of drugs with opioid antagonist activity, e.g., naloxone, or mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, buprenorphine, nalbuphine).
4.6 Fertility, pregnancy and lactation
There are no adequate data from the use of fentanyl in pregnant women. Studies in animals have shown reproductive toxicity (see Section 5.3). Opioid analgesic agents can cause neonatal respiratory depression. With long-term use during pregnancy, there is a risk of neonatal withdrawal symptoms. Fentanyl should not be used in pregnancy unless clearly necessary.
It is advised not to use fentanyl during delivery because fentanyl passes through the placenta and may cause respiratory depression in the fretus. The placental transfer ratio is 0.44 (fxtal:maternal ratio 1.00:2.27).
Fentanyl passes into breast milk, therefore women should not breast-feed while taking Fentanyl because of the possibility of sedation and/or respiratory depression in their infants. Breast feeding should not be restarted until at least 48 hours after the last administration of fentanyl.
4.7 Effects on ability to drive and use machines
No studies of the effects on the ability to drive and use machines have been performed. However, opioid analgesics may impair the mental and/or physical ability required for the performance of potentially dangerous tasks (e.g., driving a car or operating machinery). Patients should be advised not to
drive or operate machinery if they experience somnolence, dizziness, blurred or double vision while taking Fentanyl.
This medicine can impair cognitive function and can affect a patient’s ability to drive safely. This class of medicine is in the list of drugs included in regulations under 5a of the Road Traffic Act 1988. When prescribing this medicine, patients should be told:
The medicine is likely to affect your ability to drive,
• Do not drive until you know how the medicine affects you
• It is an offence to drive while under the influence of this medicine
However, you would not be committing an offence (called ‘statutory defence’) if:
• The medicine has been prescribed to treat a medical or dental problem and
• You have taken it according to the instructions given by the prescriber and in the information provided with the medicine and
• It was not affecting your ability to drive safely.
4.8 Undesirable effects
Typical opioid side effects are to be expected with Fentanyl. Frequently, these will cease or decrease in intensity with continued use of the product, as the patient is titrated to the most appropriate dose. However, the most serious adverse events are respiratory depression (potentially leading to apnoea or respiratory arrest), circulatory depression, hypotension and shock and all patients should be closely monitored for these.
Application site reactions, including gum bleeding, irritation, pain and ulcer have been reported in post-marketing use.
Because the clinical trials of Fentanyl were designed to evaluate safety and efficacy in treating breakthrough pain, all patients were also taking concomitant opioids, such as sustained-release morphine or transdermal fentanyl, for their persistent pain. Thus it is not possible to definitively separate the effects of Fentanyl alone.
The following adverse reactions have been reported with Fentanyl during clinical studies and post marketing experience. Adverse reactions are listed below as MedDRA preferred term by system organ class and frequency (frequencies are defined as: very common >1/10, common >1/100 to <1/10, uncommon > 1/1,000 to <1/100, not known (cannot be estimated from the available data):
Immune system disorders
Not known: anaphylactic reaction, tongue oedema, lip oedema
Metabolism and nutrition disorders
Common: anorexia
Psychiatric disorders
Common: confusion, anxiety, hallucinations, depression, emotional lability
Uncommon: abnormal dreams, depersonalisation, abnormal thinking, euphoria
Nervous system disorders
Very common: somnolence, dizziness, headache
Common: loss of consciousness, convulsion, vertigo, myoclonus, sedation,
paraesthesia (including hyperaesthesia/circumoral paraesthesia), abnormal gait/incoordination, taste perversion
Uncommon: coma, slurred speech
Eye disorders
Common: abnormal vision (blurred, double vision)
Vascular disorders
Unommon: vasodilatation
Respiratory, thoracic and mediastinal disorders
Very common: dyspnoea
Not known: pharyngeal oedema
Gastrointestinal disorders
Very common: nausea, vomiting, constipation, abdominal pain
Common: dry mouth, dyspepsia, stomatitis, tongue disorder (for example,
burning sensation, ulcers), flatulence, abdomen enlarged
Uncommon: ileus, , mouth ulcers, dental caries, gingival bleeding
Not known: tooth loss, gingival recession, gingivitis
Skin and subcutaneous tissue disorders
Common: pruritus, sweating, rash
Uncommon: urticaria
Renal and urinary disorders
Ccommon: urinary retention
General disorders and administration site conditions
Very common: asthenia
Common: application site reactions including irritation, pain and ulcer, malaise
Investigations
Common: weight decreased
Injury, poisoning and procedural complications
Common: accidental injury (for example, falls)
4.9 Overdose
The symptoms of fentanyl overdosage are expected to be similar in nature to those of intravenous fentanyl and other opioids, and are an extension of its pharmacological actions, with the most serious significant effects being altered mental status, loss of consciousness, coma, cardiorespiratory arrest, respiratory depression, respiratory distress, and respiratory failure, which have resulted in death.
Immediate management of opioid overdose includes removal of the Fentanyl unit via the applicator, if still in the mouth, ensuring a patent airway, physical and verbal stimulation of the patient, assessment of the level of consciousness, ventilatory and circulatory status, and assisted ventilation (ventilatory support) if necessary.
For treatment of overdosage (accidental ingestion) in the opioid naive person, intravenous access should be obtained, and naloxone or other opioid antagonists should be employed as clinically indicated. The duration of respiratory depression following overdose may be longer than the effects of the opioid antagonist’s action (e.g., the half-life of naloxone ranges from 30 to 81 minutes) and repeated administration may be necessary. Consult the Summary of Product Characteristics of the individual opioid antagonist for details about such use.
For treatment of overdose in opioid-maintained patients, intravenous access should be obtained. The judicious use of naloxone or another opioid antagonist may be warranted in some instances, but it is associated with the risk of precipitating an acute withdrawal syndrome.
Although muscle rigidity interfering with respiration has not been seen following the use of Fentanyl, this is possible with fentanyl and other opioids. If it occurs, it should be managed by the use of assisted ventilation, by an opioid antagonist, and as a final alternative, by a neuromuscular blocking agent.
5 PHARMACOLOGICAL PROPERTIES
Pharmacodynamic properties
5.1
Pharmacotherapeutic group: Opioid analgesic, phenylpiperidone derivative. ATC code N02A BO3.
Fentanyl, a pure opioid agonist, acts primarily through interaction with mu-opioid receptors located in the brain, spinal cord and smooth muscle. The primary site of therapeutic action is the central nervous system (CNS). The most clinically useful pharmacological effect of the interaction of fentanyl with mu-opioid receptors is analgesia. The analgesic effects of fentanyl are related to the blood level of the active substance, if proper allowance is made for the delay into and out of the CNS (a process with a 3-5 minute half-life). In opioid-naive individuals, analgesia occurs at blood levels of 1 to 2 ng/ml, while blood levels of 10-20 ng/ml would produce surgical anaesthesia and profound respiratory depression.
In patients with chronic cancer pain on stable doses of regularly scheduled opioids to control their persistent pain, Fentanyl produced significantly more breakthrough pain relief compared with placebo at 15, 30, 45, and 60 minutes following administration.
Secondary actions include increase in the tone and decrease in the contractions of the gastrointestinal smooth muscle, which results in prolongation of gastrointestinal transit time and may be responsible for the constipatory effect of opioids.
While opioids generally increase the tone of urinary tract smooth muscle, the overall effect tends to vary, in some cases producing urinary urgency, in others difficulty in urination.
All opioid mu-receptor agonists, including fentanyl, produce dose dependent respiratory depression. The risk of respiratory depression is less in patients with pain and those receiving chronic opioid therapy who develop tolerance to respiratory depression and other opioid effects. In non-tolerant subjects, typically peak respiratory effects are seen 15 to 30 minutes following the administration of Fentanyl, and may persist for several hours.
There is limited experience of the use of Fentanyl in paediatric patients, below the age of 16. In a clinical study, 15 (out of 38) paediatric patients, ranging in age from 5 to 15 years, already receiving maintenance opioid therapy and with breakthrough pain were treated with Fentanyl. The study was too small to allow conclusions on safety and efficacy in this patient population.
5.2 Pharmacokinetic properties General introduction
Fentanyl is highly lipophilic and can be absorbed very rapidly through the oral mucosa and more slowly by the conventional gastrointestinal route. It is subject to first-pass hepatic and intestinal metabolism and the metabolites do not contribute to fentanyl’s therapeutic effects.
Absorption
The absorption pharmacokinetics of fentanyl from Fentanyl are a combination of rapid oromucosal absorption and slower gastrointestinal absorption of swallowed fentanyl. Approximately 25% of the total dose of Fentanyl is rapidly absorbed from the buccal mucosa. The remaining 75% of the dose is swallowed and slowly absorbed from the gastrointestinal tract. About 1/3 of this amount (25% of the total dose) escapes hepatic and intestinal first-pass elimination and becomes systemically available. Absolute bioavailability is about 50% compared to intravenous fentanyl, divided equally between rapid oromucosal and slower gastrointestinal absorption. Cmax ranges from 0.39 to 2.51 ng/ml after consumption of Fentanyl (200 micrograms to 1600 micrograms). Tmax is around 20 to 40 minutes after consumption of an Fentanyl unit (range 20 - 480 minutes).
Distribution
Animal data show that fentanyl is rapidly distributed to the brain, heart, lungs, kidneys and spleen followed by a slower redistribution to muscles and fat. The plasma protein binding of fentanyl is 80-85%. The main binding protein is alpha-1-acid glycoprotein, but both albumin and lipoproteins contribute to some extent. The free fraction of fentanyl increases with acidosis. The mean volume of distribution at steady state (Vss) is 4 l/kg.
Biotransformation
Fentanyl is metabolised in the liver and in the intestinal mucosa to norfentanyl by CYP3A4 isoform. Norfentanyl is not pharmacologically active in animal studies. More than 90% of the administered dose of fentanyl is eliminated by biotransformation to N-dealkylated and hydroxylated inactive metabolites.
Elimination
Less than 7% of the dose is excreted unchanged in the urine, and only about 1% is excreted unchanged in the faeces. The metabolites are mainly excreted in the urine, while faecal excretion is less important. The total plasma clearance of fentanyl is 0.5 l/hr/kg (range 0.3-0.7 l/hr/kg). The terminal elimination half-life after Fentanyl administration is about 7 hours.
Linearity/non-linearity
Dose proportionality across the available range of dosages (200 micrograms to 1600 micrograms) of Fentanyl has been demonstrated.
Paediatric population
In a clinical study, 15 paediatric patients, ranging in age from 5 to 15 years, already receiving maintenance opioid therapy and with breakthrough pain were treated with Fentanyl at doses ranging from 200 mcg to 600 mcg. Area under the curve values based on observed concentrations were 2-fold higher in younger children than adolescents (5.25 versus 2.65 ng.hr/mL, respectively) and 4-fold higher in the younger children as compared to adults (5.25 versus 1.20 ng.hr/mL). On a weight-adjusted basis, clearance and volume of distribution values were similar across the age range.
5.3 Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity and carcinogenicity.
Embryo-foetal developmental toxicity studies conducted in rats and rabbits revealed no compound-induced malformations or developmental variations when administered during the period of organogenesis.
In a fertility and early embryonic development study in rats, a male-mediated effect was observed at high doses (300 mcg/kg/day, s.c.) and is consistent with the sedative effects of fentanyl in animal studies.
In studies on pre and postnatal development in rats the survival rate of offspring was significantly reduced at doses causing severe maternal toxicity. Further findings at maternally toxic doses in F1 pups were delayed physical development, sensory functions, reflexes and behaviour. These effects could either be indirect effects due to altered maternal care and/or decreased lactation rate or a direct effect of fentanyl on the pups.
Carcinogenicity studies (26-week dermal alternative bioassay in Tg.AC transgenic mice; two-year subcutaneous carcinogenicity study in rats) did not induce any findings indicative of oncogenic potential.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Lozenge:
Dextrates hydrated (containing glucose)
Citric acid, anhydrous Disodium phosphate, anhydrous
Artificial berry flavour (maltodextrin, propylene glycol, artificial flavours and triethylcitrate)
Magnesium stearate
Edible glue used to attach the lozenge to the handle:
Modified maize based food starch (E1450) Confectioner’s sugar (sucrose and maize starch) Water, purified
Imprinting ink:
De-ionised water De-waxed white shellac Propylene glycol
Blue synthetic coal tar dye (E133)
6.2 Incompatibilities
Not applicable
6.3 Shelf life
3 years
6.4 Special precautions for storage
Do not store above 30°C.
6.5 Nature and contents of container
Each Fentanyl dosage unit is contained in a heat sealed blister package consisting of a paper/foil laminated lid, and a PVC/Aclar thermoformed blister, supplied in cartons of 3, 6, 15 or 30 individual units.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
Lozenges with residual active substance should at no time be discarded or misplaced. Any used or unused but no longer required product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
TEVA UK Limited Brampton Road,
Hampden Park,
Eastbourne,
East Sussex BN22 9AG UNITED KINGDOM
8
9
MARKETING AUTHORISATION NUMBER(S)
PL 00289/1718
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
11/03/2013
DATE OF REVISION OF THE TEXT
25/09/2014