Flixotide 250 Micrograms Cfc-Free Inhaler
502322/PL1f
Package Leaflet: Information for the User
Flixotide®
250 micrograms Evohaler®
(fluticasone propionate)
The name of your medicine is Flixotide® 250 micrograms Evohaler®. Throughout this leaflet it will be referred to as Flixotide®.
• If you are over 16 years of age and are on higher doses (above
1,000 micrograms daily) you should take your medicine via the Volumatic® large-volume spacer device to help reduce side-effects in the mouth and throat. Your doctor, nurse or pharmacist will be able to advise you about this.
• Some people find it difficult to release a puff of medicine just after they start to breathe in. The Volumatic® spacer device helps to overcome this problem. Your doctor, nurse or pharmacist will be able to advise you about this.
• It takes a few days for this medicine to work and it is very important that you use it regularly.
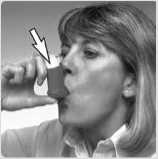
4 Hold the inhaler upright with your thumb on the base, below the mouthpiece. Breathe out as far as is comfortable. Do not breathe in again yet.
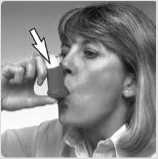
5Place the
mouthpiece in your mouth between your teeth. Close your lips around it. Do not bite.
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, nurse or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor, nurse or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1 What Flixotide® is and what it is used for
2 What you need to know before you use Flixotide®
3 How to use Flixotide®
4 Possible side effects
5 How to store Flixotide®
6 Contents of the pack and other information
1 What Flixotide® is and what it is used for
Fluticasone propionate belongs to a group of medicines called corticosteroids (often just called steroids). A very small dose of steroid is needed when it is inhaled. This is because it is inhaled straight to your lungs.
Flixotide® works by reducing swelling and irritation in the lungs. It has what is called an 'anti-inflammatory action'.
Flixotide® helps to prevent asthma attacks in people who need regular treatment. This is why it is sometimes called a 'preventer'. It needs to be used regularly, every day.
Flixotide® will not help treat sudden asthma attacks where you feel breathless.
• A different medicine is used for treating sudden attacks (called a 'reliever').
• If you have more than one medicine, be careful not to confuse them.
2 What you need to know before you use Flixotide®
Do not use:
• if you are allergic to fluticasone propionate or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, nurse or pharmacist before taking if:
• you have ever been treated for tuberculosis (TB).
• you are using Flixotide® at the same time as taking steroid tablets. Also if you have just finished taking steroid tablets. In both cases, you should carry a steroid warning card until your doctor tells you not to carry one.
If you are not sure if any of the above applies to you, talk to your doctor, nurse or pharmacist before using Flixotide®.
Other medicines and Flixotide®
Tell your doctor, nurse or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription. This includes herbal medicines. Remember to take this medicine with you if you have to go into hospital.
In particular tell your doctor or pharmacist if you are taking any of the following:
• a type of antiviral medicine known as a 'protease inhibitor' (such as ritonavir)
• medicines used to treat fungal infections (such as ketoconazole).
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist before using Flixotide®.
Using Flixotide® with food and drink
You can use Flixotide® at any time of day, with or without food.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
Driving and using machines
Flixotide® is not likely to affect you being able to drive or use any tools or machines.
3 How to use Flixotide®
Flixotide® comes in three different strengths. Your doctor will have decided which strength you need. Always use Flixotide® exactly as your doctor has told you. Check with your doctor, nurse or pharmacist if you are not sure.
Using this medicine
The medicine in Flixotide® should be inhaled using a special kind of inhaler called an Evohaler®.
• Make sure that you have one and can use it properly.
• Instructions on how to use the inhaler are given as a step-by-step guide.
Adults and Children over 16 years of age
Mild asthma
• The usual starting dose is 100 micrograms twice a day.
Moderate to severe asthma
• The usual starting dose is 250 to 500 micrograms twice a day.
• The most taken should be 1000 micrograms twice a day.
Flixotide® Evohaler® 125 and 250 micrograms are not recommended for children below 16 years of age.
It is recommended that children being treated with steroids, including Flixotide® Evohaler® have their height checked regularly by their doctor.
Your doctor may give you a Flixotide® 250 microgram Evohaler® if your dose is increased.
If you are using high doses of an inhaled steroid for a long time you may sometimes need extra steroids for example during stressful circumstances such as a road traffic accident or before an operation. Your doctor may decide to give you extra steroid medicines during this time.
Patients who have been on high doses of steroids, including Flixotide® for a long time, must not stop taking their medicine suddenly without talking to their doctor. Suddenly stopping treatment can make you feel unwell and may cause symptoms such as vomiting, drowsiness, nausea, headache, tiredness, loss of appetite, low blood sugar level and fitting.
Instructions for use
Your doctor, nurse or pharmacist should show you how to use your inhaler. They should check how you use it from time to time. Not using the Flixotide® Evohaler® properly or as prescribed, may mean that the medicine will not help your asthma as it should.
The medicine is contained in a pressurised canister in a plastic casing with a mouthpiece.
Testing your inhaler
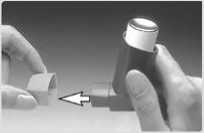
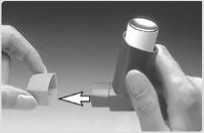
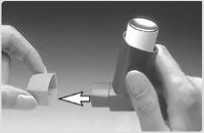
1When using the inhaler for the first time, test that it is working. Remove the mouthpiece cover by gently squeezing the sides with your thumb and forefinger and pull apart.
2 To make sure that it works, shake it well, point the mouthpiece away from you and press the canister to release a puff into the air. If you have not used the inhaler for a week or more, release two puffs of medicine into the air.
Using your inhaler
It is important to start to breathe as slowly as possible just before using your inhaler.
1 Stand or sit upright when using your inhaler.
2 Remove the mouthpiece cover (as shown in the first picture).
Check inside and outside to make sure that the mouthpiece is clean and free of objects.

Shake the inhaler 4 or 5 times to ensure that any loose objects are removed and that the contents of the inhaler are evenly mixed.

Breathe in through your mouth.
Just after starting to breathe in, press down on the top of the canister to release a puff of medicine. Do this while still breathing in steadily and deeply.

Hold your breath; take the inhaler from your mouth and your finger from the top of the inhaler. Continue holding your breath for a few seconds, or as long as is comfortable.

If your doctor has told you to take two puffs, wait about half a minute before you take another puff by repeating steps 3 to 7.
9 Afterwards, rinse your mouth with water and spit it out.
After use always replace the mouthpiece cover straight away to keep out dust. Replace the cover by firmly pushing and clicking into position.
Practise in front of a mirror for the first few times. If you see a 'mist' coming from the top of your inhaler or the sides of your mouth you should start again.
Older children or people with weak hands may find it easier to hold the inhaler with both hands. Put the two forefingers on top of the inhaler and both thumbs on the bottom below the mouthpiece. If this does not help, a special device called a Haleraid® may make it easier. Your doctor, nurse or pharmacist will be able to advise you.
Cleaning your Evohaler®
T o stop your inhaler blocking, it is important to clean it at least once a week.
To clean your inhaler:
• Remove the mouthpiece cover.
• Do not remove the metal canister from the plastic casing at any time.
• Wipe the inside and outside of the mouthpiece and the plastic casing with a dry cloth or tissue.
• Replace the mouthpiece cover.
Do not put the metal canister in water.
If you use more Flixotide® than you should
If you use more than you should, talk to your doctor as soon as possible.
It is important that you take your dose as stated on the pharmacist's label or as advised by your doctor. You should not increase or decrease your dose without seeking medical advice.
If you forget to use Flixotide®
• Take the next dose when it is due.
• Do not take a double dose to make up for the forgotten dose.
If you stop using Flixotide®
• Do not stop treatment even if you feel better unless told to do so by your doctor.
If you have any further questions on the use of this medicine, ask your doctor, nurse or pharmacist.
• level of sugar (glucose) in your blood may be increased.
• the way steroids are produced by your body may be affected when using Flixotide®. This is more likely to happen if you use high doses for a long period of time (e.g. 400 micrograms daily in children).This can cause:
- young people to grow more slowly.
- something called 'Cushing's syndrome'. This happens when you have too much steroid in your body and it can cause thinning of your bones and eye problems (such as cataracts and glaucoma which is high pressure in the eye).
Your doctor will help stop this happening by making sure you use the lowest dose of steroid which controls your symptoms.
Although the frequency is not known, the following side effects may also occur:
• depression, feeling restless or nervous. These effects are more likely to occur in children.
• nosebleeds
Talk to your doctor as soon as possible if:
• after 7 days of using Flixotide® your shortness of breath or wheezing does not get better, or gets worse.
• you or your child is on high doses of inhaled steroid and become unwell with vague symptoms such as tummy ache, sickness, diarrhoea, headache or drowsiness. This can happen during an infection such as a viral infection or stomach upset. It is important that your steroid is not stopped suddenly as this could make your asthma worse and could also cause problems with the body's hormones.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse.
This includes any possible side effects not listed in this leaflet.
You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5 How to store Flixotide®
• Keep out of the sight and reach of children.
• Clean your inhaler on a weekly basis and if it becomes blocked as described under 'Cleaning',
• Do not use this medicine after the expiry date, which is stated on the label and carton after 'EXP'. The expiry date refers to the last day of that month.
• Do not store above 30°C. Protect from frost. Protect from sunlight.
• Do not refrigerate or freeze.
• If the inhaler gets very cold, take the metal canister out of the plastic case and warm it in your hands for a few minutes before use. Never use anything else to warm it up.
• The metal canister is pressurised. Do not puncture, break or burn it even when apparently empty.
• Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
• If you are told to stop taking this medicine, return the inhaler to your pharmacist to be destroyed.
4 Possible side effects
6 Contents of the pack and other information
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If you notice any of the following serious side effects, stop using this medicine and talk to your doctor straight away. You may need urgent medical treatment.
• allergic reactions (may affect up to 1 in 100 people) - the signs include skin rashes, redness, itching or weals like nettle rash or hives
• severe allergic reactions (may affect up to 1 in 10,000 people) - the signs include swelling of your face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing, itchy rash, feeling faint and light headed and collapse
• your breathing or wheezing gets worse straight after using your inhaler. Other side effects include:
Very common (may affect more than 1 in 10 people)
• thrush in the mouth and throat
Common (may affect up to 1 in 10 people)
• sore tongue or throat
• hoarseness of voice
Problems with your mouth and throat can be reduced by doing certain things straight after inhaling your dose. These are brushing your teeth, rinsing your mouth or gargling with water and spitting it out. Tell your doctor if you have these problems with your mouth or throat, but do not stop treatment unless you are told to.
The following side effects have also been reported in patients with Chronic Obstructive Pulmonary Disease (COPD):
• Pneumonia and bronchitis (lung infection). Tell your doctor if you notice any of the following symptoms: increased sputum production, change in sputum colour, fever, chills, increased cough, increased breathing problems
• Bruising.
Rare (may affect up to 1 in 1,000 people)
• thrush (candidiasis) in the oesophagus
Very rare (may affect up to 1 in 10,000 people)
• sleeping problems or feeling worried, over-excited and irritable. These effects are more likely to occur in young people
• joint pains
• indigestion
What Flixotide® contains
• Each actuation contains 250 micrograms of fluticasone propionate.
• The other ingredient is HFA 134a.
What Flixotide® looks like and contents of the pack
• A two-tone orange inhaler comprising of an aluminium alloy canister, sealed with a metering valve, actuator and dust cap, delivering a pressurised inhalation suspension.
• Each canister contains 120 doses.
Product Licence Holder:
Procured from within the EU. Product Licence Holder Ginova Ltd and repackager Ginova UK Ltd both at St James' House, 8 Overcliffe, Gravesend, Kent, DA11 0HJ.
Manufacturers:
Glaxo Wellcome S.A., Aranda de Duero, Burgos, Spain.
Glaxo Wellcome S.A., Severo Ochoa, 2, 28760 Tres Cantos, Madrid, Spain.
Flixotide® 250 micrograms Evohaler® _
PL No: 18067/0285 |POM|
Other formats:
T o request a copy of this leaflet in Braille, large print or audio please call 01622 690172.
Leaflet date: 11th June 2015.
Flixotide®, Evohaler®, Volumatic® and Haleraid® are registered trademarks of the GlaxoSmithKline group of companies.
502322/PL1f
4 Hold the inhaler upright with your thumb on the base, below the mouthpiece. Breathe out as far as is comfortable. Do not breathe in again yet.
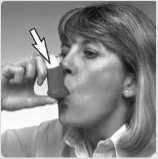
5Place the
mouthpiece in your mouth between your teeth. Close your lips around it. Do not bite.
500775/PL1g
Package Leaflet: Information for the User
Flixotide®
250 micrograms CFC-Free Inhaler (fluticasone propionate)
The name of your medicine is Flixotide® 250 micrograms CFC-Free Inhaler. Throughout this leaflet it will be referred to as Flixotide®.
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, nurse or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor, nurse or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1 What Flixotide® is and what it is used for
2 What you need to know before you use Flixotide®
3 How to use Flixotide®
4 Possible side effects
5 How to store Flixotide®
6 Contents of the pack and other information
1 What Flixotide® is and what it is used for
Fluticasone propionate belongs to a group of medicines called corticosteroids (often just called steroids). A very small dose of steroid is needed when it is inhaled. This is because it is inhaled straight to your lungs.
Flixotide® works by reducing swelling and irritation in the lungs. It has what is called an 'anti-inflammatory action'.
Flixotide® helps to prevent asthma attacks in people who need regular treatment. This is why it is sometimes called a 'preventer'. It needs to be used regularly, every day.
Flixotide® will not help treat sudden asthma attacks where you feel breathless.
• A different medicine is used for treating sudden attacks (called a 'reliever').
• If you have more than one medicine, be careful not to confuse them.
2 What you need to know before you use Flixotide®
Do not use:
• if you are allergic to fluticasone propionate or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, nurse or pharmacist before taking if:
• you have ever been treated for tuberculosis (TB).
• you are using Flixotide® at the same time as taking steroid tablets. Also if you have just finished taking steroid tablets. In both cases, you should carry a steroid warning card until your doctor tells you not to carry one.
If you are not sure if any of the above applies to you, talk to your doctor, nurse or pharmacist before using Flixotide®.
Other medicines and Flixotide®
Tell your doctor, nurse or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription. This includes herbal medicines. Remember to take this medicine with you if you have to go into hospital.
In particular tell your doctor or pharmacist if you are taking any of the following:
• a type of antiviral medicine known as a 'protease inhibitor' (such as ritonavir)
• medicines used to treat fungal infections (such as ketoconazole).
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist before using Flixotide®.
Using Flixotide® with food and drink
You can use Flixotide® at any time of day, with or without food.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
Driving and using machines
Flixotide® is not likely to affect you being able to drive or use any tools or machines.
3 How to use Flixotide®
Flixotide® comes in three different strengths. Your doctor will have decided which strength you need. Always use Flixotide® exactly as your doctor has told you. Check with your doctor, nurse or pharmacist if you are not sure.
Using this medicine
The medicine in Flixotide® should be inhaled using a special kind of inhaler called a CFC-Free Inhaler.
• Make sure that you have one and can use it properly.
• Instructions on how to use the inhaler are given as a step-by-step guide.
If you are over 16 years of age and are on higher doses (above
1,000 micrograms daily) you should take your medicine via the Volumatic® large-volume spacer device to help reduce side-effects in the mouth and throat. Your doctor, nurse or pharmacist will be able to advise you about this. Some people find it difficult to release a puff of medicine just after they start to breathe in. The Volumatic® spacer device helps to overcome this problem. Your doctor, nurse or pharmacist will be able to advise you about this.
It takes a few days for this medicine to work and it is very important that you use it regularly.
Adults and Children over 16 years of age
Mild asthma
• The usual starting dose is 100 micrograms twice a day.
Moderate to severe asthma
• The usual starting dose is 250 to 500 micrograms twice a day.
• The most taken should be 1000 micrograms twice a day.
Flixotide® CFC-Free Inhaler 125 and 250 micrograms are not recommended for children below 16 years of age.
It is recommended that children being treated with steroids, including Flixotide® CFC-Free Inhaler have their height checked regularly by their doctor.
Your doctor may give you a Flixotide® 250 microgram CFC-Free Inhaler if your dose is increased.
If you are using high doses of an inhaled steroid for a long time you may sometimes need extra steroids for example during stressful circumstances such as a road traffic accident or before an operation. Your doctor may decide to give you extra steroid medicines during this time.
Patients who have been on high doses of steroids, including Flixotide® for a long time, must not stop taking their medicine suddenly without talking to their doctor. Suddenly stopping treatment can make you feel unwell and may cause symptoms such as vomiting, drowsiness, nausea, headache, tiredness, loss of appetite, low blood sugar level and fitting.
Instructions for use
Your doctor, nurse or pharmacist should show you how to use your inhaler.
They should check how you use it from time to time. Not using the Flixotide® CFC-Free Inhaler properly or as prescribed, may mean that the medicine will not help your asthma as it should.
The medicine is contained in a pressurised canister in a plastic casing with a mouthpiece.
Testing your inhaler
1When using the inhaler for the first time, test that it is working. Remove the mouthpiece cover by gently squeezing the sides with your thumb and forefinger and pull apart.
2 To make sure that it works, shake it well, point the mouthpiece away from you and press the canister to release a puff into the air. If you have not used the inhaler for a week or more, release two puffs of medicine into the air.
Using your inhaler
It is important to start to breathe as slowly as possible just before using your inhaler.
1 Stand or sit upright when using your inhaler.
2 Remove the mouthpiece cover (as shown in the first picture).
Check inside and outside to make sure that the mouthpiece is clean and free of objects.

Shake the inhaler 4 or 5 times to ensure that any loose objects are removed and that the contents of the inhaler are evenly mixed.

Breathe in through your mouth.
Just after starting to breathe in, press down on the top of the canister to release a puff of medicine. Do this while still breathing in steadily and deeply.

Hold your breath; take the inhaler from your mouth and your finger from the top of the inhaler. Continue holding your breath for a few seconds, or as long as is comfortable.

If your doctor has told you to take two puffs, wait about half a minute before you take another puff by repeating steps 3 to 7.
9 Afterwards, rinse your mouth with water and spit it out.
After use always replace the mouthpiece cover straight away to keep out dust. Replace the cover by firmly pushing and clicking into position.
Practise in front of a mirror for the first few times. If you see a 'mist' coming from the top of your inhaler or the sides of your mouth you should start again.
Older children or people with weak hands may find it easier to hold the inhaler with both hands. Put the two forefingers on top of the inhaler and both thumbs on the bottom below the mouthpiece. If this does not help, a special device called a Haleraid® may make it easier. Your doctor, nurse or pharmacist will be able to advise you.
Cleaning your CFC-Free Inhaler
To stop your inhaler blocking, it is important to clean it at least once a week.
To clean your inhaler:
• Remove the mouthpiece cover.
• Do not remove the metal canister from the plastic casing at any time.
• Wipe the inside and outside of the mouthpiece and the plastic casing with a dry cloth or tissue.
• Replace the mouthpiece cover.
Do not put the metal canister in water.
If you use more Flixotide® than you should
If you use more than you should, talk to your doctor as soon as possible.
It is important that you take your dose as stated on the pharmacist's label or as advised by your doctor. You should not increase or decrease your dose without seeking medical advice.
If you forget to use Flixotide®
• Take the next dose when it is due.
• Do not take a double dose to make up for the forgotten dose.
If you stop using Flixotide®
• Do not stop treatment even if you feel better unless told to do so by your doctor.
If you have any further questions on the use of this medicine, ask your doctor, nurse or pharmacist.
• level of sugar (glucose) in your blood may be increased.
• the way steroids are produced by your body may be affected when using Flixotide®. This is more likely to happen if you use high doses for a long period of time (e.g. 400 micrograms daily in children).This can cause:
- young people to grow more slowly.
- something called 'Cushing's syndrome'. This happens when you have too much steroid in your body and it can cause thinning of your bones and eye problems (such as cataracts and glaucoma which is high pressure in the eye).
Your doctor will help stop this happening by making sure you use the lowest dose of steroid which controls your symptoms.
Although the frequency is not known, the following side effects may also occur:
• depression, feeling restless or nervous. These effects are more likely to occur in children.
• nosebleeds
Talk to your doctor as soon as possible if:
• after 7 days of using Flixotide® your shortness of breath or wheezing does not get better, or gets worse.
• you or your child is on high doses of inhaled steroid and become unwell with vague symptoms such as tummy ache, sickness, diarrhoea, headache or drowsiness. This can happen during an infection such as a viral infection or stomach upset. It is important that your steroid is not stopped suddenly as this could make your asthma worse and could also cause problems with the body's hormones.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse.
This includes any possible side effects not listed in this leaflet.
You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5 How to store Flixotide®
• Keep out of the sight and reach of children.
• Clean your inhaler on a weekly basis and if it becomes blocked as described under 'Cleaning',
• Do not use this medicine after the expiry date, which is stated on the label and carton after 'EXP'. The expiry date refers to the last day of that month.
• Do not store above 30°C. Protect from frost. Protect from sunlight.
• Do not refrigerate or freeze.
• If the inhaler gets very cold, take the metal canister out of the plastic case and warm it in your hands for a few minutes before use. Never use anything else to warm it up.
• The metal canister is pressurised. Do not puncture, break or burn it even when apparently empty.
• Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
• If you are told to stop taking this medicine, return the inhaler to your pharmacist to be destroyed.
4 Possible side effects
6 Contents of the pack and other information
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If you notice any of the following serious side effects, stop using this medicine and talk to your doctor straight away. You may need urgent medical treatment.
• allergic reactions (may affect up to 1 in 100 people) - the signs include skin rashes, redness, itching or weals like nettle rash or hives
• severe allergic reactions (may affect up to 1 in 10,000 people) - the signs include swelling of your face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing, itchy rash, feeling faint and light headed and collapse
• your breathing or wheezing gets worse straight after using your inhaler.
Other side effects include:
Very common (may affect more than 1 in 10 people)
• thrush in the mouth and throat
Common (may affect up to 1 in 10 people)
• sore tongue or throat
• hoarseness of voice
Problems with your mouth and throat can be reduced by doing certain things straight after inhaling your dose. These are brushing your teeth, rinsing your mouth or gargling with water and spitting it out. Tell your doctor if you have these problems with your mouth or throat, but do not stop treatment unless you are told to.
The following side effects have also been reported in patients with Chronic Obstructive Pulmonary Disease (COPD):
• Pneumonia and bronchitis (lung infection). Tell your doctor if you notice any of the following symptoms: increased sputum production, change in sputum colour, fever, chills, increased cough, increased breathing problems
• Bruising.
Rare (may affect up to 1 in 1,000 people)
• thrush (candidiasis) in the oesophagus
Very rare (may affect up to 1 in 10,000 people)
• sleeping problems or feeling worried, over-excited and irritable. These effects are more likely to occur in young people
• joint pains
• indigestion
What Flixotide® contains
• Each actuation contains 250 micrograms of fluticasone propionate.
• The other ingredient is HFA 134a.
What Flixotide® looks like and contents of the pack
• A two-tone orange inhaler comprising of an aluminium alloy canister, sealed with a metering valve, actuator and dust cap, delivering a pressurised inhalation suspension.
• Each canister contains 120 doses.
Product Licence Holder:
Procured from within the EU. Product Licence Holder Ginova Ltd and repackager Ginova UK Ltd both at St James' House, 8 Overcliffe, Gravesend, Kent, DA11 0HJ.
Manufacturers:
Glaxo Wellcome S.A., Aranda de Duero, Burgos, Spain.
Glaxo Wellcome S.A., Severo Ochoa, 2, 28760 Tres Cantos, Madrid, Spain.
Flixotide® 250 micrograms CFC-Free Inhaler _
PL No: 18067/0285 |POM|
Other formats:
T o request a copy of this leaflet in Braille, large print or audio please call 01622 690172.
Leaflet date: 11th June 2015.
Flixotide®, Volumatic® and Haleraid® are registered trademarks of the GlaxoSmithKline group of companies.
500775/PL1g
Package Leaflet: Information for the User
Fluticasone Propionate
250 micrograms CFC-Free Inhaler
The name of your medicine is Fluticasone Propionate 250 micrograms CFC-Free Inhaler. Throughout this leaflet it will be referred to as Fluticasone Propionate.
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, nurse or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor, nurse or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1 What Fluticasone Propionate is and what it is used for
2 What you need to know before you use Fluticasone Propionate
3 How to use Fluticasone Propionate
4 Possible side effects
5 How to store Fluticasone Propionate
6 Contents of the pack and other information
1 What Fluticasone Propionate is and what it is used for
Fluticasone propionate belongs to a group of medicines called corticosteroids (often just called steroids). A very small dose of steroid is needed when it is inhaled. This is because it is inhaled straight to your lungs.
Fluticasone Propionate works by reducing swelling and irritation in the lungs. It has what is called an 'anti-inflammatory action'.
Fluticasone Propionate helps to prevent asthma attacks in people who need regular treatment. This is why it is sometimes called a 'preventer'. It needs to be used regularly, every day.
Fluticasone Propionate will not help treat sudden asthma attacks where you feel breathless.
• A different medicine is used for treating sudden attacks (called a 'reliever').
• If you have more than one medicine, be careful not to confuse them.
2 What you need to know before you use Fluticasone Propionate
Do not use:
• if you are allergic to fluticasone propionate or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, nurse or pharmacist before taking if:
• you have ever been treated for tuberculosis (TB).
• you are using Fluticasone Propionate at the same time as taking steroid tablets. Also if you have just finished taking steroid tablets. In both cases, you should carry a steroid warning card until your doctor tells you not to carry one.
If you are not sure if any of the above applies to you, talk to your doctor, nurse or pharmacist before using Fluticasone Propionate.
Other medicines and Fluticasone Propionate
Tell your doctor, nurse or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription. This includes herbal medicines. Remember to take this medicine with you if you have to go into hospital.
In particular tell your doctor or pharmacist if you are taking any of the following:
• a type of antiviral medicine known as a 'protease inhibitor' (such as ritonavir)
• medicines used to treat fungal infections (such as ketoconazole).
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist before using Fluticasone Propionate.
Using Fluticasone Propionate with food and drink
You can use Fluticasone Propionate at any time of day, with or without food.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
Driving and using machines
Fluticasone Propionate is not likely to affect you being able to drive or use any tools or machines.
3 How to use Fluticasone Propionate
Fluticasone Propionate comes in three different strengths. Your doctor will have decided which strength you need. Always use Fluticasone Propionate exactly as your doctor has told you. Check with your doctor, nurse or pharmacist if you are not sure.
Using this medicine
The medicine in Fluticasone Propionate should be inhaled using a special kind of inhaler called a CFC-Free Inhaler.
• Make sure that you have one and can use it properly.
• Instructions on how to use the inhaler are given as a step-by-step guide.
• If you are over 16 years of age and are on higher doses (above
1,000 micrograms daily) you should take your medicine via the Volumatic® large-volume spacer device to help reduce side-effects in the mouth and throat. Your doctor, nurse or pharmacist will be able to advise you about this.
• Some people find it difficult to release a puff of medicine just after they start to breathe in. The Volumatic® spacer device helps to overcome this problem. Your doctor, nurse or pharmacist will be able to advise you about this.
• It takes a few days for this medicine to work and it is very important that you use it regularly.
Adults and Children over 16 years of age
Mild asthma
• The usual starting dose is 100 micrograms twice a day.
Moderate to severe asthma
• The usual starting dose is 250 to 500 micrograms twice a day.
• The most taken should be 1000 micrograms twice a day.
Fluticasone Propionate CFC-Free Inhaler 125 and 250 micrograms are not recommended for children below 16 years of age.
It is recommended that children being treated with steroids, including Fluticasone Propionate CFC-Free Inhaler have their height checked regularly by their doctor.
Your doctor may give you a Fluticasone Propionate 250 microgram CFC-Free Inhaler if your dose is increased.
If you are using high doses of an inhaled steroid for a long time you may sometimes need extra steroids for example during stressful circumstances such as a road traffic accident or before an operation. Your doctor may decide to give you extra steroid medicines during this time.
Patients who have been on high doses of steroids, including Fluticasone Propionate for a long time, must not stop taking their medicine suddenly without talking to their doctor. Suddenly stopping treatment can make you feel unwell and may cause symptoms such as vomiting, drowsiness, nausea, headache, tiredness, loss of appetite, low blood sugar level and fitting.
Instructions for use
Your doctor, nurse or pharmacist should show you how to use your inhaler.
They should check how you use it from time to time. Not using the Fluticasone Propionate CFC-Free Inhaler properly or as prescribed, may mean that the medicine will not help your asthma as it should.
The medicine is contained in a pressurised canister in a plastic casing with a mouthpiece.
Testing your inhaler
1When using the inhaler for the first time, test that it is working. Remove the mouthpiece cover by gently squeezing the sides with your thumb and forefinger and pull apart.
2 To make sure that it works, shake it well, point the mouthpiece away from you and press the canister to release a puff into the air. If you have not used the inhaler for a week or more, release two puffs of medicine into the air.
Using your inhaler
It is important to start to breathe as slowly as possible just before using your inhaler.
1 Stand or sit upright when using your inhaler.
2 Remove the mouthpiece cover (as shown in the first picture).
Check inside and outside to make sure that the mouthpiece is clean and free of objects.

Shake the inhaler 4 or 5 times to ensure that any loose objects are removed and that the contents of the inhaler are evenly mixed.

5Place the
mouthpiece in your mouth between your teeth. Close your lips around it. Do not bite.
4 Hold the inhaler upright with your thumb on the base, below the mouthpiece. Breathe out as far as is comfortable. Do not breathe in again yet.
Breathe in through your mouth.
Just after starting to breathe in, press down on the top of the canister to release a puff of medicine. Do this while still breathing in steadily and deeply.

Hold your breath; take the inhaler from your mouth and your finger from the top of the inhaler. Continue holding your breath for a few seconds, or as long as is comfortable.

If your doctor has told you to take two puffs, wait about half a minute before you take another puff by repeating steps 3 to 7.
9 Afterwards, rinse your mouth with water and spit it out.
After use always replace he mouthpiece cover straight away to keep out dust. Replace the cover by firmly pushing and clicking into position.
Practise in front of a mirror for the first few times. If you see a 'mist' coming from the top of your inhaler or the sides of your mouth you should start again.
Older children or people with weak hands may find it easier to hold the inhaler with both hands. Put the two forefingers on top of the inhaler and both thumbs on the bottom below the mouthpiece. If this does not help, a special device called a Haleraid® may make it easier. Your doctor, nurse or pharmacist will be able to advise you.
Cleaning your CFC-Free Inhaler
To stop your inhaler blocking, it is important to clean it at least once a week.
• level of sugar (glucose) in your blood may be increased.
• the way steroids are produced by your body may be affected when using Fluticasone Propionate. This is more likely to happen if you use high doses for a long period of time (e.g. 400 micrograms daily in children).This can cause:
- young people to grow more slowly.
- something called 'Cushing's syndrome'. This happens when you have too much steroid in your body and it can cause thinning of your bones and eye problems (such as cataracts and glaucoma which is high pressure in the eye).
Your doctor will help stop this happening by making sure you use the lowest dose of steroid which controls your symptoms.
Although the frequency is not known, the following side effects may also occur:
• depression, feeling restless or nervous. These effects are more likely to occur in children.
• nosebleeds
Talk to your doctor as soon as possible if:
• after 7 days of using Fluticasone Propionate your shortness of breath or wheezing does
not get better, or gets worse.
• you or your child is on high doses of inhaled steroid and become unwell with vague symptoms such as tummy ache, sickness, diarrhoea, headache or drowsiness. This can happen during an infection such as a viral infection or stomach upset. It is important that your steroid is not stopped suddenly as this could make your asthma worse and could also cause problems with the body's hormones.
To clean your inhaler:
• Remove the mouthpiece cover.
• Do not remove the metal canister from the plastic casing at any time.
• Wipe the inside and outside of the mouthpiece and the plastic casing with a dry cloth or tissue.
• Replace the mouthpiece cover.
Do not put the metal canister in water.
If you use more Fluticasone Propionate than you should
If you use more than you should, talk to your doctor as soon as possible.
It is important that you take your dose as stated on the pharmacist's label or as advised by your doctor. You should not increase or decrease your dose without seeking medical advice.
If you forget to use Fluticasone Propionate
• Take the next dose when it is due.
• Do not take a double dose to make up for the forgotten dose.
If you stop using Fluticasone Propionate
• Do not stop treatment even if you feel better unless told to do so by your doctor.
If you have any further questions on the use of this medicine, ask your doctor, nurse or pharmacist.
4 Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If you notice any of the following serious side effects, stop using this medicine and talk to your doctor straight away. You may need urgent medical treatment.
• allergic reactions (may affect up to 1 in 100 people) - the signs include skin rashes, redness, itching or weals like nettle rash or hives
• severe allergic reactions (may affect up to 1 in 10,000 people) - the signs include swelling of your face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing, itchy rash, feeling faint and light headed and collapse
• your breathing or wheezing gets worse straight after using your inhaler. Other side effects include:
Very common (may affect more than 1 in 10 people)
• thrush in the mouth and throat
Common (may affect up to 1 in 10 people)
• sore tongue or throat
• hoarseness of voice
Problems with your mouth and throat can be reduced by doing certain things straight after inhaling your dose. These are brushing your teeth, rinsing your mouth or gargling with water and spitting it out. Tell your doctor if you have these problems with your mouth or throat, but do not stop treatment unless you are told to.
The following side effects have also been reported in patients with Chronic Obstructive Pulmonary Disease (COPD):
• Pneumonia and bronchitis (lung infection). Tell your doctor if you notice any of the following symptoms: increased sputum production, change in sputum colour, fever, chills, increased cough, increased breathing problems
• Bruising.
Rare (may affect up to 1 in 1,000 people)
• thrush (candidiasis) in the oesophagus
Very rare (may affect up to 1 in 10,000 people)
• sleeping problems or feeling worried, over-excited and irritable. These effects are more likely to occur in young people
• joint pains
• indigestion
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse.
This includes any possible side effects not listed in this leaflet.
You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5 How to store Fluticasone Propionate
• Keep out of the sight and reach of children.
• Clean your inhaler on a weekly basis and if it becomes blocked as described under 'Cleaning',
• Do not use this medicine after the expiry date, which is stated on the label and carton after 'EXP'. The expiry date refers to the last day of that month.
• Do not store above 30°C. Protect from frost. Protect from sunlight.
• Do not refrigerate or freeze.
• If the inhaler gets very cold, take the metal canister out of the plastic case and warm it in your hands for a few minutes before use. Never use anything else to warm it up.
• The metal canister is pressurised. Do not puncture, break or burn it even when apparently empty.
• Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
• If you are told to stop taking this medicine, return the inhaler to your pharmacist to be destroyed.
6 Contents of the pack and other information
What Fluticasone Propionate contains
• Each actuation contains 250 micrograms of fluticasone propionate.
• The other ingredient is HFA 134a.
What Fluticasone Propionate looks like and contents of the pack
• A two-tone orange inhaler comprising of an aluminium alloy canister, sealed with a metering valve, actuator and dust cap, delivering a pressurised inhalation suspension.
• Each canister contains 120 doses.
Product Licence Holder:
Procured from within the EU. Product Licence Holder Ginova Ltd and repackager Ginova UK Ltd both at St James' House, 8 Overcliffe,
Gravesend, Kent, DA11 0HJ.
Manufacturers:
Glaxo Wellcome S.A., Aranda de Duero, Burgos, Spain.
Glaxo Wellcome S.A., Severo Ochoa, 2, 28760 Tres Cantos, Madrid, Spain.
Fluticasone Propionate 250 micrograms CFC-Free Inhaler
PL No: 18067/0285 |POM|
Other formats:
T o request a copy of this leaflet in Braille, large print or audio please call 01622 690172.
Leaflet date: 11th June 2015.
Fluticasone Propionate, Volumatic® and Haleraid® are registered trademarks of the GlaxoSmithKline group of companies.
500777/PL1h