Flutiform 125Microgram /5 Microgram Per Actuation Pressurised Inhalation Suspension
Package leaflet: Informat ion for the user
Abriff® 125 microgram /5 microgram per actuation pressurised inhalation, suspension
(fluticasone propionate/formoterol fumarate dihydrate)
Perform steps 2 to 5 below, slowly.

Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, pharmacist or asthma nurse.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects talk to your doctor, pharmacist or asthma nurse. This includes any possible side effects not listed in this leaflet. See section 4.
The name of your medicine is Abriff® 125 microgram /
5 microgram per actuation pressurised inhalation, suspension, but will be referred to as Abriff inhaler in this leaflet.
What is in this leaflet:
1. What Abriff inhaler is and what it is used for
2. What you need to know before you use Abriff inhaler
3. How to use Abriff inhaler
4. Possible side effects
5. How to store Abriff inhaler
6. Contents of the pack and other information
1. What Abriff inhaler is and what it is used for
Abriff is an inhaler (a pressurised inhalation, suspension) which contains two active ingredients:
• Fluticasone propionate which belongs to a group of medicines called steroids. Steroids help to reduce swelling and inflammation in the lungs.
• Formoterol fumarate dihydrate which belongs to a group of medicines called long-acting beta2 agonists. Long-acting beta2 agonists are long-acting bronchodilators which help the airways in your lungs to stay open, making it easier for you to breathe.
Together these two active ingredients help to improve your breathing. It is advised that you should use this medicine every day as directed by your doctor or asthma nurse.
This medicine helps to prevent breathing problems such as asthma and helps to stop you becoming breathless and wheezy. However, it does not work if you are already having an asthma attack i.e. you are already breathless and wheezing.
You will need to use a fast acting 'reliever' medicine such as salbutamol if this happens.
2. What you need to know before you use Abriff inhaler
Do not use Abriff inhaler if you:
• are allergic to fluticasone propionate, formoterol fumarate or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist or asthma nurse before using this inhaler.
Before treatment with this inhaler tell your doctor, pharmacist or asthma nurse if you have:
• tuberculosis (TB) now or in the past. Symptoms include a persistent cough often with blood streaked phlegm, fever, tiredness, loss of appetite, loss of weight and night sweats;
• an infection of the lungs or chest;
• heart problems such as problems with the blood flow to your heart or narrowing of one of your heart valves (the aortic valve), heart failure which can cause shortness of breath or ankle swelling, a condition where the heart muscle is enlarged (hypertrophic obstructive cardiomyopathy), an irregular heart beat (cardiac arrhythmias) or if you have been told that your heart trace is abnormal (prolongation of the QTc interval);
• an abnormal bulging of a blood vessel wall (an aneurysm);
• diabetes;
• high blood pressure;
• an overactive thyroid gland which can cause increased appetite, weight loss or sweating (thyrotoxicosis);
• low blood levels of potassium which can cause muscle weakness, twitching or abnormal heart rhythm (hypokalaemia);
• poor adrenal gland function (if your adrenal gland is not working properly you may have symptoms such as headaches, weakness, tiredness, abdominal pain, loss of appetite, weight loss, dizziness, very low blood pressure, diarrhoea, feeling or being sick or fits) or a tumor of the adrenal gland (phaeochromocytoma);
• liver problems.
If you are going to have an operation or are extremely stressed, please tell your doctor as you may need additional steroid treatment to control your asthma.
Other medicines and Abriff inhaler
Tell your doctor, pharmacist or asthma nurse if you are taking, have recently taken or might take any other medicines. If you use this inhaler with some other medicines the effect of this inhaler or the other medicine may be altered.
Tell your doctor, pharmacist or asthma nurse if you are taking:
• medicines known as beta-blockers (such as atenolol to treat blood pressure, sotalol to treat an irregular heart beat, metoprolol to treat a fast heart beat or timolol eye drops to treat glaucoma);
• certain other medicines used to treat asthma or breathing conditions (such as theophylline or aminophylline);
• medicines containing adrenaline or related substances (including other beta-agonists like salbutamol or beta-antagonists including atenolol, metoprolol, propranolol, timolol). Additional long-acting beta2 agonists should not be used together with this inhaler. If your asthma becomes worse between doses of Abriff inhaler then you should use your quick acting 'reliever' inhaler for immediate relief;
• medicines to treat allergic reactions (antihistamines);
• medicines to treat high blood pressure or fluid build up by increasing the amount of urine produced (diuretics);
• medicines used to treat heart failure (such as digoxin);
• medicines to treat abnormal heart rhythms (such as quinidine, disopyramide, procainamide);
• medicines to treat symptoms of depression or mental disorders such as monoamine oxidase inhibitors (for example phenelzine and isocarboxazid), tricyclic antidepressants (for example amitriptyline and imipramine), or you have taken any of these types of medicine in the last two weeks;
• medicines used to treat psychiatric or mental disorders (phenothiazines or antipsychotics);
• other medicines containing steroids;
• antifungal medicines (such as ketaconazole or itraconazole);
• medicines used to treat viral infections including HIV (for example ritonavir, atazanavir, indinavir, nelfinavir or saquinavir);
• antibiotics (such as clarithromycin, telithromycin or furazolidone);
• medicine to treat Parkinson's disease (levodopa);
• medicine to treat an underactive thyroid gland (levothyroxine);
• medicine to treat Hodgkin's disease (procarbazine);
• medicine to induce labour (oxytocin).
If you are going to have an operation under a general anaesthetic, please tell the doctor at the hospital that you are using this inhaler.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant or are planning to have a baby ask your doctor or asthma nurse for advice about using your inhaler. Your doctor or asthma nurse will advise you if you should take this medicine.
Driving and using machines
This medicine is unlikely to affect your ability to drive or use machines.
Abriff inhaler contains ethanol (alcohol) and sodium cromoglicate
This medicine contains very small amounts of ethanol (alcohol),
i.e 1.00 mg per actuation (puff). It also contains a very small amount of sodium cromoglicate however patients who are currently taking cromoglicate (used to treat asthma, allergic rhinitis and allergic conjunctivitis) should continue as normal.
3. How to use Abriff inhaler
Always use this inhaler exactly as your doctor, pharmacist or asthma nurse has told you. Check with your doctor, pharmacist or asthma nurse if you are not sure. You should use your inhaler regularly i.e. two actuations (puffs) in the morning and two actuations (puffs) in the evening every day to get the most benefit from your inhaler, unless your doctor tells you otherwise or advises you to stop. Do not take more than the prescribed dose. Your doctor may have prescribed your inhaler for a different indication other than asthma/or at a different dose from that normally prescribed and as described in this leaflet. You should always use your inhaler exactly as your doctor or asthma nurse has advised. If you are not sure about how much to take or how often to use your inhaler please check with your doctor, pharmacist or asthma nurse.
Adults and adolescents over 12 years of age
The usual dose is two inhalations twice a day, that is two puffs (actuations) in the morning and two in the evening. Your doctor will prescribe the dose required to treat your asthma. Adolescents should not use the highest strength inhaler (Abriff 250 microgram /10 microgram).
Abriff inhaler should not be used in children under 12 years of age.
Instructions for use
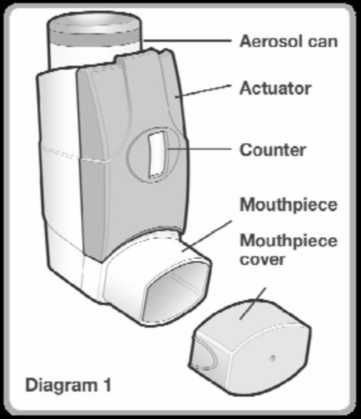
Read this leaflet very carefully prior to use and follow the instructions for use in the text and diagrams below. Your doctor, pharmacist or asthma nurse will show you how to use your inhaler properly. The medicine is contained in an aerosol can (see Diagram 1) which sits inside a plastic dispenser (also known as an actuator). The actuator also has a counter to tell you how many puffs (actuations) are left after it has been primed. The counter is also coloured coded. It starts off green then, when there are less than 50 puffs (actuations) left it changes to yellow and when there are less than 30 puffs (actuations) left it changes to red.
When this is getting near to zero, you should contact your doctor or asthma nurse for a replacement inhaler.
Do not use your inhaler when the counter reads zero.
Before you use your inhaler for the first time or if it hasn't been used for more than 3 days or if it has been exposed to freezing conditions
If your inhaler is new or it hasn't been used for more than 3 days then it must be 'primed' to ensure it works properly and gives you the correct dose.
If your inhaler has been exposed to freezing temperatures it must be allowed to warm at room temperature for 30 minutes then it must be 'primed' to ensure it works properly and gives you the correct dose.
To prime the inhaler
• Remove the mouthpiece cover and shake the inhaler well.
• Point the mouthpiece away from you and release one puff (actuation) by pressing down on the aerosol can. This step should be performed 4 times.
Your inhaler should always be shaken immediately before use. Using your inhaler
If you feel you are getting breathless or wheezy while using Abriff inhaler, you should continue to use Abriff inhaler but go to see your doctor or asthma nurse as soon as possible, as you may need additional treatment.
Once your asthma is well controlled your doctor or asthma nurse may consider it appropriate to gradually reduce the dose of Abriff inhaler.
1. Remove the mouthpiece cover (see Diagram 2) and check that your inhaler is clean and free from any dust.
2. The inhaler should be shaken immediately before releasing each puff (actuation) to ensure the contents of your inhaler are evenly mixed.
3. Sit upright or stand. Breathe out as far as is comfortable and as slowly and as deeply as possible.
POM
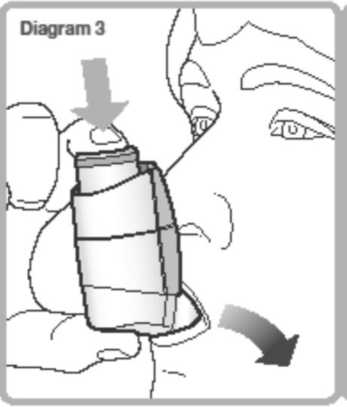
4. Hold your inhaler upright (as shown in Diagram 3) and put the mouthpiece in your mouth with your lips around it. Hold the inhaler with your thumb(s) on the base of the mouthpiece and forefinger/index finger(s) on the top of the inhaler. Do not bite the mouthpiece.
5. Breathe in slowly and deeply through your mouth and, at the same time, press down on the aerosol can to release one puff (actuation). Continue to breathe in steadily and deeply (ideally for about 4-5 seconds).

6. While holding your breath, remove the inhaler from your mouth. Continue to hold your breath for as long as is comfortable. Do not breathe out into the inhaler.
7. For the second puff (actuation), keep the inhaler in a vertical position then repeat steps 2 to 6.
8. Replace the mouthpiece cover.
You can practise in front of a mirror. If you see a 'mist' from the top of the inhaler or around your mouth when you use your inhaler then you may not have inhaled your medicine properly. Take another dose by repeating from Step 2 above.
Always rinse your mouth out, gargle with water or brush your teeth after you have taken your inhaler and spit out the residue. This may help prevent you developing a sore mouth and throat or a hoarse voice.
If you have weak hands it may be easier to hold the inhaler in both hands placing both index fingers on the aerosol can and both thumbs on the base of the inhaler.
If you have difficulty using your inhaler your doctor or asthma nurse may give you a device called an AeroChamber Plus® spacing device, to help you to breathe your medicine into your lungs properly. Your doctor, pharmacist or asthma nurse will advise you how to use the AeroChamber Plus spacing device with your inhaler. The AeroChamber Plus spacing device will come with instructions for use and with care and cleaning instructions which you must read carefully.
Caring for your inhaler
It is important that you follow these instructions carefully and clean your inhaler weekly. To clean your inhaler:
• Remove the mouthpiece cover.
• Do not remove the aerosol can from the actuator.
• Wipe the inside and outside of the mouthpiece and the actuator with a clean, dry cloth or tissue.
• Replace the mouthpiece cover.
• Do not put the metal canister into water.
If you use more Abriff inhaler than you should
It is important that you take your dose as stated on the pharmacist's label or as advised by your doctor or asthma nurse. You should not increase or decrease your dose without seeking medical advice.
If you take more of your medicine than you should, contact your doctor, pharmacist or asthma nurse for advice. You may suffer from severe chest pain (angina), high or low blood pressure, a headache, muscle cramps, difficulty in sleeping, nervousness, a dry mouth, a loss of appetite, seizures, fits or convulsions. You may feel shaky, light headed, faint, tired, sick or generally unwell. You may also notice changes in the rate of your heart beat and your blood may have low levels of potassium or an increase in the amount of sugar in your blood. You may also suffer from symptoms such as abdominal pain, being sick, weight loss, decreased level of consciousness (which could make you feel drowsy or confused) or a low blood sugar level.
If you have taken more than the prescribed dose for a long period of time, you should talk to your doctor, pharmacist or asthma nurse for advice. This is because large doses may reduce the amount of steroid hormones produced normally by your adrenal glands (see section 4).
If you forget to use Abriff inhaler
If you forget to take a dose, take it as soon as you remember. However, if it is nearly time for your next dose, skip the missed dose. Do not take a double dose to make up for a forgotten dose.
If you stop using Abriff inhaler
It is very important that you take this inhaler every day as directed by your doctor even if you feel well as it will help to control your asthma. If you want to stop using your inhaler talk to your doctor first. Your doctor will tell you how to do this, usually by decreasing the dose gradually so that you do not trigger an asthma attack.
4. Possible side effects
Like all medicines, this inhaler can cause side effects, although not everybody gets them. Your doctor or asthma nurse will prescribe the lowest dose necessary to control your asthma which may reduce the possibility of side effects occurring.
All medicines can cause allergic reactions, although serious allergic reactions are reported rarely. Tell your doctor immediately if you get any sudden swelling of the eyelids, face, throat, tongue or lips, rash or itching especially those covering your whole body, symptoms such as dizziness, lightheadedness or fainting or any sudden changes in your breathing pattern such as increased wheezing or shortness of breath.
As with other inhalers, your breathing may worsen immediately after using your inhaler. You may notice an increase in wheezing and shortness of breath. If this happens stop using your Abriff inhaler and use your quick acting 'reliever' inhaler. Contact your doctor or asthma nurse straight away. Your doctor or asthma nurse will assess you and may start you on a different course of treatment. You should carry your 'reliever' inhaler with you at all times.
Uncommon: may affect up to 1 in 100 people
• Worsening of asthma.
• Headache.
• Shaking.
• An irregular heartbeat or palpitations.
• Dizziness.
• Difficulty sleeping.
• Alteration in voice/hoarse voice.
• Dry mouth, sore or irritated throat.
• Rash.
Rare: may affect up to 1 in 1000 people
• An increase in the amount of sugar in your blood. If you are diabetic you may need to check your blood sugar more often and adjust your usual diabetic treatment. Your doctor may need to monitor you more closely.
• Thrush or other fungal infections in the mouth and throat.
• Inflammation of the sinuses (sinusitis).
• Fast heartbeat.
• Chest pain associated with heart disease.
• Muscle spasms.
• Coughing or shortness of breath.
• Diarrhoea.
• Indigestion.
• Changes in taste.
• A feeling of dizziness or 'spinning'.
• Abnormal dreams.
• Agitation.
• Itchy skin.
• High blood pressure.
• A feeling of unusual weakness.
• Swelling of hands, ankles or feet.
Not Known Frequency cannot be estimated from the available data
• Sleeping problems, depression or feeling worried, aggression, anxiety, restlessness, nervousness, overexcitement or irritability. These effects are more likely to occur in children.
The following side effects are associated with formoterol fumarate but they have not been reported during clinical trials with this inhaler:
• Low blood levels of potassium which can cause muscle weakness, twitching or abnormal heart rhythm.
• An abnormal heart trace potentially leading to an abnormal heart rhythm (QTc interval prolongation).
• High levels of lactic acid in the blood.
• Feeling sick.
• Muscle pain.
Inhaled steroids can affect the normal production of steroid hormones in your body, particularly if you use high doses for a long time. The effects include:
• changes in bone mineral density (thinning of the bones);
• cataracts (clouding of the lens in the eye);
• glaucoma (increased pressure in the eye);
• bruising or thinning of the skin;
• an increased chance of catching an infection;
• slowing of the rate of growth of children and adolescents;
• a round (moon shaped) face;
• an effect on the adrenal gland (a small gland next to the kidney) which means you may have symptoms such as weakness, tiredness, difficulty in coping with stress, abdominal pain, loss of appetite, weight loss, headache, dizziness, very low blood pressure, diarrhoea, feeling or being sick or fits.
These effects are much less likely to happen with inhaled steroids than with steroid tablets.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Abriff inhaler
Keep out of the sight and reach of children.
Do not use this inhaler after the expiry date which is stated on the label, foil pouch and carton after EXP. The expiry date refers to the last day of that month.
Do not store above 25°C.
Do not refrigerate or freeze.
If the inhaler is exposed to freezing conditions it must be allowed to warm at room temperature for 30 minutes then primed before use (see section 3 "How to use ...").
Do not use the inhaler if it has been removed from the foil pouch for more than 3 months, or if the dose indicator reads '0'.
Do not expose to temperatures higher than 50°C.
The aerosol can contains a pressurised liquid so do not puncture, break or burn the can even when apparently empty. Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. Contents of the pack and other information
What Abriff inhaler contains
Each metered dose (ex-valve) contains 125 microgram of fluticasone propionate and 5 microgram of formoterol fumarate dihydrate. This is equivalent to a delivered dose (ex-actuator) of approximately 115 microgram of fluticasone propionate and 4.5 microgram of formoterol fumarate dihydrate.
Also contains:
• sodium cromoglicate,
• anhydrous ethanol and
• apaflurane HFA 227 (propellant).
What Abriff inhaler looks like and the contents of the pack
These inhalers are small aerosol cans containing a white to off white liquid suspension in an aluminium pressurised canister in a white actuator with a grey integrated dose indicator and light grey mouthpiece cover. Supplied in a foil pouch.
There is one inhaler in a pack.
Each inhaler contains 120 puffs (actuations).
The device has a counter which tells you the number of blisters remaining. It counts down from 120 to 0. When the counter shows 0, your inhaler is empty and should be disposed of.
Manufactured by:
Bard Pharmaceuticals Limited, Cambridge Science Park, Milton Road, Cambridge,
CB4 0GW, UK.
Or
Mundipharma pharmaceuticals DC B.V.,
De Wel 20, NL-3871 M.V, Hoevelaken,
The Netherlands.
Procured from within the EU & repackaged by PL holder:
Kosei Pharma UK Limited, 956 Buckingham Avenue, Slough Trading Estate, Slough, SL1 4NL, UK
Abriff® 125 microgram /5 microgram per actuation pressurised inhalation, suspension
PL 39352/0333
Abriff® is a registered trademark of Mundipharma AG.
Leaflet date: 26/02/2016
Flutiform® 125 microgram /5 microgram per actuation pressurised inhalation, suspension
(fluticasone propionate/formoterol fumarate dihydrate)
Perform steps 2 to 5 below, slowly.

Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, pharmacist or asthma nurse.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects talk to your doctor, pharmacist or asthma nurse. This includes any possible side effects not listed in this leaflet. See section 4.
The name of your medicine is Flutiform® 125 microgram /
5 microgram per actuation pressurised inhalation, suspension, but will be referred to as Flutiform inhaler in this leaflet.
What is in this leaflet:
7. What Flutiform inhaler is and what it is used for
8. What you need to know before you use Flutiform inhaler
9. How to use Flutiform inhaler
10. Possible side effects
11. How to store Flutiform inhaler
12. Contents of the pack and other information
1. What Flutiform inhaler is and what it is used
Flutiform is an inhaler (a pressurised inhalation, suspension) which contains two active ingredients:
• Fluticasone propionate which belongs to a group of medicines called steroids. Steroids help to reduce swelling and inflammation in the lungs.
• Formoterol fumarate dihydrate which belongs to a group of medicines called long-acting beta2 agonists. Long-acting beta2 agonists are long-acting bronchodilators which help the airways in your lungs to stay open, making it easier for you to breathe.
Together these two active ingredients help to improve your breathing. It is advised that you should use this medicine every day as directed by your doctor or asthma nurse.
This medicine helps to prevent breathing problems such as asthma and helps to stop you becoming breathless and wheezy. However, it does not work if you are already having an asthma attack i.e. you are already breathless and wheezing.
You will need to use a fast acting 'reliever' medicine such as salbutamol if this happens.
2. What you need to know before you use Flutiform inhaler
Do not use Flutiform inhaler if you:
• are allergic to fluticasone propionate, formoterol fumarate or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist or asthma nurse before using this inhaler.
Before treatment with this inhaler tell your doctor, pharmacist or asthma nurse if you have:
• tuberculosis (TB) now or in the past. Symptoms include a persistent cough often with blood streaked phlegm, fever, tiredness, loss of appetite, loss of weight and night sweats;
• an infection of the lungs or chest;
• heart problems such as problems with the blood flow to your heart or narrowing of one of your heart valves (the aortic valve), heart failure which can cause shortness of breath or ankle swelling, a condition where the heart muscle is enlarged (hypertrophic obstructive cardiomyopathy), an irregular heart beat (cardiac arrhythmias) or if you have been told that your heart trace is abnormal (prolongation of the QTc interval);
• an abnormal bulging of a blood vessel wall (an aneurysm);
• diabetes;
• high blood pressure;
• an overactive thyroid gland which can cause increased appetite, weight loss or sweating (thyrotoxicosis);
• low blood levels of potassium which can cause muscle weakness, twitching or abnormal heart rhythm (hypokalaemia);
• poor adrenal gland function (if your adrenal gland is not working properly you may have symptoms such as headaches, weakness, tiredness, abdominal pain, loss of appetite, weight loss, dizziness, very low blood pressure, diarrhoea, feeling or being sick or fits) or a tumor of the adrenal gland (phaeochromocytoma);
• liver problems.
If you are going to have an operation or are extremely stressed, please tell your doctor as you may need additional steroid treatment to control your asthma.
Other medicines and Flutiform inhaler
Tell your doctor, pharmacist or asthma nurse if you are taking, have recently taken or might take any other medicines. If you use this inhaler with some other medicines the effect of this inhaler or the other medicine may be altered.
Tell your doctor, pharmacist or asthma nurse if you are taking:
• medicines known as beta-blockers (such as atenolol to treat blood pressure, sotalol to treat an irregular heart beat, metoprolol to treat a fast heart beat or timolol eye drops to treat glaucoma);
• certain other medicines used to treat asthma or breathing conditions (such as theophylline or aminophylline);
• medicines containing adrenaline or related substances (including other beta-agonists like salbutamol or beta-antagonists including atenolol, metoprolol, propranolol, timolol). Additional long-acting beta2 agonists should not be used together with this inhaler. If your asthma becomes worse between doses of Flutiform inhaler then you should use your quick acting 'reliever' inhaler for immediate relief;
• medicines to treat allergic reactions (antihistamines);
• medicines to treat high blood pressure or fluid build up by increasing the amount of urine produced (diuretics);
• medicines used to treat heart failure (such as digoxin);
• medicines to treat abnormal heart rhythms (such as quinidine, disopyramide, procainamide);
• medicines to treat symptoms of depression or mental disorders such as monoamine oxidase inhibitors (for example phenelzine and isocarboxazid), tricyclic antidepressants (for example amitriptyline and imipramine), or you have taken any of these types of medicine in the last two weeks;
• medicines used to treat psychiatric or mental disorders (phenothiazines or antipsychotics);
• other medicines containing steroids;
• antifungal medicines (such as ketaconazole or itraconazole);
• medicines used to treat viral infections including HIV (for example ritonavir, atazanavir, indinavir, nelfinavir or saquinavir);
• antibiotics (such as clarithromycin, telithromycin or furazolidone);
• medicine to treat Parkinson's disease (levodopa);
• medicine to treat an underactive thyroid gland (levothyroxine);
• medicine to treat Hodgkin's disease (procarbazine);
• medicine to induce labour (oxytocin).
If you are going to have an operation under a general anaesthetic, please tell the doctor at the hospital that you are using this inhaler.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant or are planning to have a baby ask your doctor or asthma nurse for advice about using your inhaler. Your doctor or asthma nurse will advise you if you should take this medicine.
Driving and using machines
This medicine is unlikely to affect your ability to drive or use machines.
Flutiform inhaler contains ethanol (alcohol) and sodium cromoglicate
This medicine contains very small amounts of ethanol (alcohol), i.e 1.00 mg per actuation (puff). It also contains a very small amount of sodium cromoglicate however patients who are currently taking cromoglicate (used to treat asthma, allergic rhinitis and allergic conjunctivitis) should continue as normal.
3. How to use Flutiform inhaler
Always use this inhaler exactly as your doctor, pharmacist or asthma nurse has told you. Check with your doctor, pharmacist or asthma nurse if you are not sure. You should use your inhaler regularly i.e. two actuations (puffs) in the morning and two actuations (puffs) in the evening every day to get the most benefit from your inhaler, unless your doctor tells you otherwise or advises you to stop. Do not take more than the prescribed dose. Your doctor may have prescribed your inhaler for a different indication other than asthma/or at a different dose from that normally prescribed and as described in this leaflet. You should always use your inhaler exactly as your doctor or asthma nurse has advised. If you are not sure about how much to take or how often to use your inhaler please check with your doctor, pharmacist or asthma nurse.
Adults and adolescents over 12 years of age
The usual dose is two inhalations twice a day, that is two puffs (actuations) in the morning and two in the evening. Your doctor will prescribe the dose required to treat your asthma. Adolescents should not use the highest strength inhaler (Flutiform 250 microgram /10 microgram).
Flutiform inhaler should not be used in children under 12 years of age.
Instructions for use
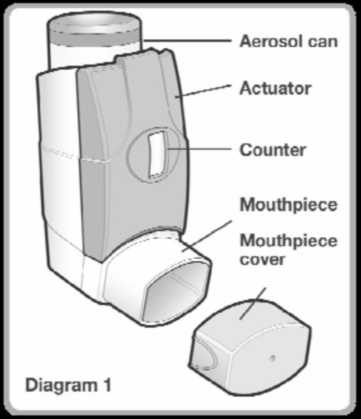
Read this leaflet very carefully prior to use and follow the instructions for use in the text and diagrams below. Your doctor, pharmacist or asthma nurse will show you how to use your inhaler properly. The medicine is contained in an aerosol can (see Diagram 1) which sits inside a plastic dispenser (also known as an actuator). The actuator also has a counter to tell you how many puffs (actuations) are left after it has been primed. The counter is also coloured coded. It starts off green then, when there are less than 50 puffs (actuations) left it changes to yellow and when there are less than 30 puffs (actuations) left it changes to red.
When this is getting near to zero, you should contact your doctor or asthma nurse for a replacement inhaler.
Do not use your inhaler when the counter reads zero.
Before you use your inhaler for the first time or if it hasn't been used for more than 3 days or if it has been exposed to freezing conditions
If your inhaler is new or it hasn't been used for more than 3 days then it must be 'primed' to ensure it works properly and gives you the correct dose.
If your inhaler has been exposed to freezing temperatures it must be allowed to warm at room temperature for 30 minutes then it must be 'primed' to ensure it works properly and gives you the correct dose.
To prime the inhaler
• Remove the mouthpiece cover and shake the inhaler well.
• Point the mouthpiece away from you and release one puff (actuation) by pressing down on the aerosol can. This step should be performed 4 times.
Your inhaler should always be shaken immediately before use. Using your inhaler
If you feel you are getting breathless or wheezy while using Flutiform inhaler, you should continue to use Flutiform inhaler but go to see your doctor or asthma nurse as soon as possible, as you may need additional treatment.
Once your asthma is well controlled your doctor or asthma nurse may consider it appropriate to gradually reduce the dose of Flutiform inhaler.
1. Remove the mouthpiece cover (see Diagram 2) and check that your inhaler is clean and free from any dust.
2. The inhaler should be shaken immediately before releasing each puff (actuation) to ensure the contents of your inhaler are evenly mixed.
3. Sit upright or stand. Breathe out as far as is comfortable and as slowly and as deeply as possible.
POM
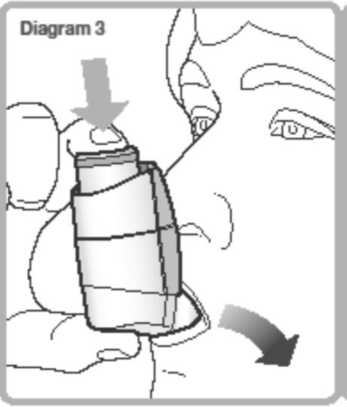
4. Hold your inhaler upright (as shown in Diagram 3) and put the mouthpiece in your mouth with your lips around it. Hold the inhaler with your thumb(s) on the base of the mouthpiece and forefinger/index finger(s) on the top of the inhaler. Do not bite the mouthpiece.
5. Breathe in slowly and deeply through your mouth and, at the same time, press down on the aerosol can to release one puff (actuation). Continue to breathe in steadily and deeply (ideally for about 4-5 seconds).

6. While holding your breath, remove the inhaler from your mouth. Continue to hold your breath for as long as is comfortable. Do not breathe out into the inhaler.
7. For the second puff (actuation), keep the inhaler in a vertical position then repeat steps 2 to 6.
8. Replace the mouthpiece cover.
You can practise in front of a mirror. If you see a 'mist' from the top of the inhaler or around your mouth when you use your inhaler then you may not have inhaled your medicine properly. Take another dose by repeating from Step 2 above.
Always rinse your mouth out, gargle with water or brush your teeth after you have taken your inhaler and spit out the residue. This may help prevent you developing a sore mouth and throat or a hoarse voice.
If you have weak hands it may be easier to hold the inhaler in both hands placing both index fingers on the aerosol can and both thumbs on the base of the inhaler.
If you have difficulty using your inhaler your doctor or asthma nurse may give you a device called an AeroChamber Plus® spacing device, to help you to breathe your medicine into your lungs properly. Your doctor, pharmacist or asthma nurse will advise you how to use the AeroChamber Plus spacing device with your inhaler. The AeroChamber Plus spacing device will come with instructions for use and with care and cleaning instructions which you must read carefully.
Caring for your inhaler
It is important that you follow these instructions carefully and clean your inhaler weekly. To clean your inhaler:
• Remove the mouthpiece cover.
• Do not remove the aerosol can from the actuator.
• Wipe the inside and outside of the mouthpiece and the actuator with a clean, dry cloth or tissue.
• Replace the mouthpiece cover.
• Do not put the metal canister into water.
If you use more Flutiform inhaler than you should
It is important that you take your dose as stated on the pharmacist's label or as advised by your doctor or asthma nurse. You should not increase or decrease your dose without seeking medical advice.
If you take more of your medicine than you should, contact your doctor, pharmacist or asthma nurse for advice. You may suffer from severe chest pain (angina), high or low blood pressure, a headache, muscle cramps, difficulty in sleeping, nervousness, a dry mouth, a loss of appetite, seizures, fits or convulsions. You may feel shaky, light headed, faint, tired, sick or generally unwell. You may also notice changes in the rate of your heart beat and your blood may have low levels of potassium or an increase in the amount of sugar in your blood. You may also suffer from symptoms such as abdominal pain, being sick, weight loss, decreased level of consciousness (which could make you feel drowsy or confused) or a low blood sugar level.
If you have taken more than the prescribed dose for a long period of time, you should talk to your doctor, pharmacist or asthma nurse for advice. This is because large doses may reduce the amount of steroid hormones produced normally by your adrenal glands (see section 4).
If you forget to use Flutiform inhaler If you forget to take a dose, take it as soon as you remember. However, if it is nearly time for your next dose, skip the missed dose. Do not take a double dose to make up for a forgotten dose.
If you stop using Flutiform inhaler
It is very important that you take this inhaler every day as directed by your doctor even if you feel well as it will help to control your asthma. If you want to stop using your inhaler talk to your doctor first. Your doctor will tell you how to do this, usually by decreasing the dose gradually so that you do not trigger an asthma attack.
4. Possible side effects
Like all medicines, this inhaler can cause side effects, although not everybody gets them. Your doctor or asthma nurse will prescribe the lowest dose necessary to control your asthma which may reduce the possibility of side effects occurring.
All medicines can cause allergic reactions, although serious allergic reactions are reported rarely. Tell your doctor immediately if you get any sudden swelling of the eyelids, face, throat, tongue or lips, rash or itching especially those covering your whole body, symptoms such as dizziness, lightheadedness or fainting or any sudden changes in your breathing pattern such as increased wheezing or shortness of breath.
As with other inhalers, your breathing may worsen immediately after using your inhaler. You may notice an increase in wheezing and shortness of breath. If this happens stop using your Flutiform inhaler and use your quick acting 'reliever' inhaler. Contact your doctor or asthma nurse straight away. Your doctor or asthma nurse will assess you and may start you on a different course of treatment. You should carry your 'reliever' inhaler with you at all times.
Uncommon: may affect up to 1 in 100 people
• Worsening of asthma.
• Headache.
• Shaking.
• An irregular heartbeat or palpitations.
• Dizziness.
• Difficulty sleeping.
• Alteration in voice/hoarse voice.
• Dry mouth, sore or irritated throat.
• Rash.
Rare: may affect up to 1 in 1000 people
• An increase in the amount of sugar in your blood. If you are diabetic you may need to check your blood sugar more often and adjust your usual diabetic treatment. Your doctor may need to monitor you more closely.
• Thrush or other fungal infections in the mouth and throat.
• Inflammation of the sinuses (sinusitis).
• Fast heartbeat.
• Chest pain associated with heart disease.
• Muscle spasms.
• Coughing or shortness of breath.
• Diarrhoea.
• Indigestion.
• Changes in taste.
• A feeling of dizziness or 'spinning'.
• Abnormal dreams.
• Agitation.
• Itchy skin.
• High blood pressure.
• A feeling of unusual weakness.
• Swelling of hands, ankles or feet.
Not Known Frequency cannot be estimated from the available data
• Sleeping problems, depression or feeling worried, aggression, anxiety, restlessness, nervousness, overexcitement or irritability. These effects are more likely to occur in children.
The following side effects are associated with formoterol fumarate but they have not been reported during clinical trials with this inhaler:
• Low blood levels of potassium which can cause muscle weakness, twitching or abnormal heart rhythm.
• An abnormal heart trace potentially leading to an abnormal heart rhythm (QTc interval prolongation).
• High levels of lactic acid in the blood.
• Feeling sick.
• Muscle pain.
Inhaled steroids can affect the normal production of steroid hormones in your body, particularly if you use high doses for a long time. The effects include:
• changes in bone mineral density (thinning of the bones);
• cataracts (clouding of the lens in the eye);
• glaucoma (increased pressure in the eye);
• bruising or thinning of the skin;
• an increased chance of catching an infection;
• slowing of the rate of growth of children and adolescents;
• a round (moon shaped) face;
• an effect on the adrenal gland (a small gland next to the kidney) which means you may have symptoms such as weakness, tiredness, difficulty in coping with stress, abdominal pain, loss of appetite, weight loss, headache, dizziness, very low blood pressure, diarrhoea, feeling or being sick or fits.
These effects are much less likely to happen with inhaled steroids than with steroid tablets.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Abriff inhaler
Keep out of the sight and reach of children.
Do not use this inhaler after the expiry date which is stated on the label, foil pouch and carton after EXP. The expiry date refers to the last day of that month.
Do not store above 25°C.
Do not refrigerate or freeze.
If the inhaler is exposed to freezing conditions it must be allowed to warm at room temperature for 30 minutes then primed before use (see section 3 "How to use ...").
Do not use the inhaler if it has been removed from the foil pouch for more than 3 months, or if the dose indicator reads '0'.
Do not expose to temperatures higher than 50°C.
The aerosol can contains a pressurised liquid so do not puncture, break or burn the can even when apparently empty. Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. Contents of the pack and other information
What Flutiform inhaler contains
Each metered dose (ex-valve) contains 125 microgram of fluticasone propionate and 5 microgram of formoterol fumarate dihydrate. This is equivalent to a delivered dose (ex-actuator) of approximately 115 microgram of fluticasone propionate and 4.5 microgram of formoterol fumarate dihydrate.
Also contains:
• sodium cromoglicate,
• anhydrous ethanol and
• apaflurane HFA 227 (propellant).
What Flutiform inhaler looks like and the contents of the pack
These inhalers are small aerosol cans containing a white to off white liquid suspension in an aluminium pressurised canister in a white actuator with a grey integrated dose indicator and light grey mouthpiece cover. Supplied in a foil pouch.
There is one inhaler in a pack.
Each inhaler contains 120 puffs (actuations).
The device has a counter which tells you the number of blisters remaining. It counts down from 120 to 0. When the counter shows 0, your inhaler is empty and should be disposed of.
Manufactured by:
Bard Pharmaceuticals Limited, Cambridge Science Park, Milton Road, Cambridge,
CB4 0GW, UK.
Or
Mundipharma pharmaceuticals DC B.V.,
De Wel 20, NL-3871 M.V, Hoevelaken,
The Netherlands.
Procured from within the EU & repackaged by PL holder:
Kosei Pharma UK Limited, 956 Buckingham Avenue, Slough Trading Estate, Slough, SL1 4NL, UK
Flutiform® 125 microgram /5 microgram per actuation pressurised inhalation, suspension
PL 39352/0333
Flutiform® is a registered trademark of Jagotec AG.
Leaflet date: 26/02/2016