Humulin I Kwikpen (Isophane) 100 Iu/Ml Suspension For Injection
PACKAGE LEAFLET: INFORMATION FOR THE USER
HUMULIN® I (Isophane) KwikPen™ 100 IU/ml suspension for injection
(insulin, human)
Read all of this leaflet carefully before you start using this medicine.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your diabetes specialist nurse, doctor or pharmacist.
- This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your diabetes specialist nurse, doctor or pharmacist.
In this leaflet:
1. What Humulin I KwikPen is and what it is used for
2. Before you use Humulin I KwikPen
3. How to use Humulin I KwikPen
4. Possible side effects
5. How to store Humulin I KwikPen
6. Further information
1. WHAT HUMULIN I KWIKPEN IS AND WHAT IT IS USED FOR
Humulin I KwikPen is a pre-filled pen containing the active substance human insulin, which is used to treat diabetes. You get diabetes if your pancreas does not make enough insulin to control the level of glucose in your blood (blood sugar). Humulin I is used to control glucose in the long term. Its action is prolonged by the inclusion of protamine sulfate in the suspension.
Your doctor may tell you to use Humulin I KwikPen as well as a fast-acting insulin. Each kind of insulin comes with its own patient information leaflet to tell you about it. Do not change your insulin unless your doctor tells you to. Be very careful if you do change insulin. Each type of insulin has a different colour and symbol on the pack and the pen so that you can easily tell the difference.
2. BEFORE YOU USE HUMULIN I KWIKPEN
Do not use Humulin I KwikPen if you:
- think hypoglycaemia (low blood sugar) is starting. Further in this leaflet it tells you how to deal with mild hypoglycaemia (see A in Section 4).
- are allergic (hypersensitive) to human insulin or any of the other ingredients of Humulin I KwikPen (see Section 6).
Take special care with Humulin I KwikPen
• If your blood sugar levels are well controlled by your current insulin therapy, you may not feel the warning symptoms when your blood sugar is falling too low. Warning signs are listed later in this leaflet. You must think carefully about when to have your meals, how often to exercise and how much to do. You must also keep a close watch on your blood sugar levels by testing your blood glucose often.
• A few people who have had hypoglycaemia (low blood sugar) after switching from animal insulin to human insulin have reported that the early warning symptoms were less obvious or different. If you often have hypoglycaemia or have difficulty recognising the symptoms, please discuss this with your doctor.
• If you answer YES to any of the following questions, tell your diabetes specialist nurse, doctor or pharmacist.
- Have you recently become ill?
- Do you have trouble with your kidneys or liver?
- Are you exercising more than usual?
• The amount of insulin you need may also change if you drink alcohol.
• You should also tell your diabetes specialist nurse, doctor or pharmacist if you are planning to go abroad. The time difference between countries may mean that you have to have your injections and meals at different times to when you are at home.
• Some patients with long-standing type 2 diabetes mellitus and heart disease or previous stroke who were treated with pioglitazone and insulin experienced the development of heart failure. Inform your doctor as soon as possible, if you experience signs of heart failure such as unusual shortness of breath or rapid increase in weight or localised swelling (oedema).
Using other medicines
Please tell your doctor or diabetes specialist nurse, if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
Your insulin needs may change if you are taking any of the following:
• steroids,
• thyroid hormone replacement therapy,
• oral hypoglycaemics (antidiabetic medication),
• acetylsalicylic acid (aspirin),
• growth hormone,
• octreotide, lanreotide,
• beta2 stimulants (for example ritodrine, salbutamol or terbutaline),
• beta-blockers,
• thiazides or some antidepressants (monoamine oxidase inhibitors),
• danazol,
• some angiotensin converting (ACE) inhibitors (for example captopril, enalapril) or angiotensin II receptor blockers
Pregnancy and breast-feeding
Ask your doctor or diabetes specialist nurse for advice before taking any medicine.
The amount of insulin you need usually falls during the first three months of pregnancy and increases for the remaining six months. If you are breast-feeding, you may need to alter your insulin intake or diet.
Driving and using machines
Your ability to concentrate and react may be reduced if you have hypoglycaemia (low blood sugar). Please remember this in all situations where you might put yourself and others at risk (e.g. driving a car or operating machinery). You should contact your diabetes specialist nurse or doctor about the advisability of driving if you have:
• frequent episodes of hypoglycaemia
• reduced or absent warning signs of hypoglycaemia.
3. HOW TO USE HUMULIN I KWIKPEN
Always check the pack and the label of the pre-filled pen for the name and type of the insulin when you get it from your pharmacy. Make sure you get the Humulin I KwikPen that your doctor has told you to use.
Always use Humulin I KwikPen exactly as your doctor has told you. You should check with your doctor if you are not sure.
Dosage
• You should normally inject Humulin I as your basal insulin. Your doctor has told you which insulin to use, how much, when and how often to inject. These instructions are only for you. Follow them exactly and visit your diabetes clinic regularly.
• If you change your insulin type (for example from animal to human), you may have to take more or less than before. This might just be for the first injection or it may be a gradual change over several weeks or months.
• Inject Humulin I under the skin. You should not administer it using a different administration route. Under no circumstances should Humulin I be given into a vein.
Preparing Humulin I KwikPen
• The KwikPen should be rotated in the palms of the hands 10 times and inverted 10 times immediately before use to resuspend insulin until it appears uniformly cloudy or milky. If not, repeat the above procedure until contents are mixed. Cartridges in the pen contain a small glass bead to assist mixing. Do not shake vigorously as this may cause frothing which may interfere with the correct measurement of the dose. The cartridges in the pen should be examined frequently and should not be used if clumps of material are present or if solid white particles stick to the bottom or sides of the cartridge, giving it a frosted appearance. Check each time you inject yourself.
Getting the KwikPen ready to use (Please see user manual)
• First wash your hands.
• Read the instructions on how to use your pre-filled insulin pen. Please follow the instructions carefully. Here are some reminders.
- Use a clean needle. (Needles are not included).
- Prime your KwikPen before each use. This checks that insulin comes out and clears the air bubbles from your KwikPen. There may still be some small air bubbles left in the KwikPen - these are harmless, but if the air bubble is too big, it may make the dose of your injection less accurate.
Injecting Humulin I
• Before you make an injection, clean your skin as you have been instructed. Inject under the skin, as you were taught. Do not inject directly into a vein. After your injection, leave the needle in the skin for 5 seconds to make sure you have taken the whole dose. Do not rub the area you have just injected. Make sure you inject at least half an inch (1 cm) from where you last injected and that you ‘rotate’ the places you inject, as you have been taught.
After injecting
• As soon as you have done the injection, unscrew the needle from the KwikPen using the outer needle cap. This will keep the insulin sterile and prevent leaking. It will also stop air going back into the KwikPen and the needle clogging up. Do not share your needles or your KwikPen. Replace the cap on the KwikPen.
Further injections
• Every time you use a KwikPen you must use a new needle. Before every injection, clear any air bubbles. You can see how much insulin is left by holding the KwikPen with the needle pointing down. The scale on the cartridge shows about how many units you have left.
• Do not mix any other insulin in your disposable pen. Once the KwikPen is empty, do not use it again. Please get rid of it carefully - your diabetes specialist nurse or pharmacist will tell you how to do this.
If you take more Humulin I than you need
If you take more Humulin I than you need, your blood sugar may become low. Check your blood sugar (see A in Section 4).
If you forget to use Humulin I KwikPen
If you take less Humulin I than you need, your blood sugar levels may increase. Check your blood sugar.
If you stop using Humulin I KwikPen
If you take less Humulin I than you need, your blood sugar levels may become too high. Do not change your insulin unless your doctor tells you to.
If you have any further questions on the use of this product, ask your diabetes specialist nurse, doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Humulin I can cause side effects, although not everybody gets them.
Human insulin may cause hypoglycaemia (low blood sugar). See more information on hypoglycaemia below in the subsection “Common problems of diabetes”.
Possible side effects
Systemic allergy is very rare (affects less than 1 person in 10,000). The symptoms are as follows:
• fall in blood pressure • rash over the whole body
• difficulty in breathing • wheezing
• fast heart beat • sweating
If you think you are having this sort of insulin allergy with Humulin I, tell your doctor at once.
Local allergy is common (affects less than 1 person in 10). Some people get redness, swelling or itching around the area of the insulin injection. This usually clears up in anything from a few days to a few weeks. If this happens to you, tell your doctor.
Lipodystrophy (thickening or pitting of the skin) is uncommon (affects less than 1 person in 100). If you notice your skin thickening or pitting at the injection site, change your injection site and tell your doctor.
Oedema (e.g. swelling in arms, ankles; fluid retention) has been reported, particularly at the start of insulin therapy or during a change in therapy to improve control of your blood glucose.
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
Common problems of diabetes
A. Hypoglycaemia
Hypoglycaemia (low blood sugar) means there is not enough sugar in the blood. This can be caused if you:
• take too much Humulin I or other insulin;
• miss or delay meals or change your diet;
• exercise or work too hard just before or after a meal;
• have an infection or illness (especially diarrhoea or vomiting);
• have a change in your need for insulin; or
• have trouble with your kidneys or liver which gets worse.
Alcohol and some medicines can affect your blood sugar levels.
The first symptoms of low blood sugar usually come on quickly and include the following:
• tiredness • rapid heartbeat
• nervousness or shakiness • feeling sick
• headache • cold sweat
Until you become confident in recognising your warning symptoms, avoid situations such as driving a car, in which you or others would be put at risk by hypoglycaemia.
Do not use Humulin I if you think hypoglycaemia (low blood sugar) is starting.
If your blood sugar is low, eat glucose tablets, sugar or drink a sugary drink. Then eat fruit, biscuits, or a sandwich, as your doctor has advised you and have some rest. This will often get you over mild hypoglycaemia or a minor insulin overdose. If you get worse and your breathing is shallow and your skin gets pale, tell your doctor at once. A glucagon injection can treat quite severe hypoglycaemia. Eat glucose or sugar after the glucagon injection. If you do not respond to glucagon, you will have to go to hospital. Ask your doctor to tell you about glucagon.
B. Hyperglycaemia and diabetic ketoacidosis
Hyperglycaemia (too much sugar in the blood) means that your body does not have enough insulin. Hyperglycaemia can be brought about by:
• not taking your Humulin I or other insulin;
• taking less insulin than your doctor tells you to;
• eating a lot more than your diet allows; or
• fever, infection or emotional stress.
Hyperglycaemia can lead to diabetic ketoacidosis. The first symptoms come on slowly over many hours or days. The symptoms include the following:
• feeling sleepy • no appetite
• flushed face • fruity smell on the breath
• thirst • feeling or being sick
Severe symptoms are heavy breathing and a rapid pulse. Get medical help immediately.
If hypoglycaemia (low blood sugar) or hyperglycaemia (high blood sugar) are not treated they can be very serious and cause headaches, nausea, vomiting, dehydration, unconsciousness, coma or even death.
Three simple steps to avoid hypoglycaemia or hyperglycaemia are:
• Always keep spare syringes and a spare vial of Humulin I.
• Always carry something to show you are diabetic.
• Always carry sugar with you.
C. Illness
If you are ill, especially if you feel sick or are sick, the amount of insulin you need may change. Even when you are not eating normally, you still need
insulin. Test your urine or blood, follow your ‘sick rules’, and tell your diabetes specialist nurse or doctor.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via Ireland: HPRA Pharmacovigilance, Earlsfort Terrace, IRL - Dublin 2, Tel: +353 1 6764971, Fax: +353 1 6762517, Website: www.hpra.ie, e-mail: medsafety@hpra.ie, United Kingdom: Yellow Card Scheme, Website: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. HOW TO STORE HUMULIN I KWIKPEN
Keep out of the reach and sight of children.
Before the first use, store your Humulin I KwikPen in a refrigerator (2°C - 8°C). Do not freeze. Keep your ‘in-use’ Humulin I KwikPen at room temperature (below 30°C) for up to 28 days. Do not keep your ‘in-use’ pen in the fridge. Do not put it near heat or in the sun.
Do not use Humulin I KwikPen after the expiry date which is stated on the label and the carton. The expiry date refers to the last day of that month.
Do not use Humulin I KwikPen, if clumps of material are present or if solid white particles stick to the bottom or sides of the cartridge, giving it a frosted appearance. Check this each time you inject yourself.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. FURTHER INFORMATION
What Humulin I KwikPen contains
The active substance is human insulin. Human insulin is made in the laboratory by a ‘recombinant DNA technology’ process. It has the same structure as the natural hormone made by the pancreas. It is therefore different from animal insulins. The human insulin in Humulin I is available in a suspension together with protamine sulfate.
The other ingredients are protamine sulfate, metacresol, phenol, glycerol, dibasic sodium phosphate 7H2O, zinc oxide and water for injection. Sodium hydroxide or hydrochloric acid may have been used during manufacture to adjust the acidity.
What Humulin I KwikPen looks like and contents of the pack
Humulin I (Isophane) KwikPen 100 IU/ml suspension for injection is a white, sterile suspension and contains 100 units of insulin in each millilitre (100 IU/ml).
Each Humulin I KwikPen contains 300 units (3 millilitres).
The Humulin I KwikPen comes in a pack of 5.
The Humulin I in your KwikPen is the same as the Humulin I, which comes in separate Humulin I cartridges. The KwikPen simply has a built in cartridge. When the KwikPen is empty you cannot use it again.
Marketing Authorisation Holder and Manufacturer
Humulin I KwikPen is made by:
Lilly France S.A.S., Rue du Colonel Lilly, 67640 Fegersheim, France.
The marketing authorisation is held by: Eli Lilly and Company Limited, Lilly House, Priestley Road, Basingstoke, Hampshire, RG24 9NL, U.K.
It is distributed in the Republic of Ireland by Eli Lilly and Company (Ireland) Limited, Hyde House, 65 Adelaide Road, Dublin 2, Ireland.
This medicinal product is authorised in the Member States of the EEA under the following names:
Huminsulin „Lilly“ Basal 100 I.E./ml - KwikPen (Austria)
Humuline-KwikPen NPH (Belgium, Luxembourg, The Netherlands)
Humulin N KwikPen (Estonia, Latvia, Lithuania, Poland, Romania)
Huminsulin Basal (NPH) 100 KwikPen (Germany)
Humulin NPH KwikPen (Denmark, Finland, Iceland, Norway, Slovenia, Sweden) Humulin (NPH) KwikPen (Greece)
Humulina NPH KwikPen 100 (Spain)
Humulin I KwikPen (Ireland, UK)
Umuline NPH KwikPen (France)
This leaflet was last approved in March 2015.
If you would like a large-print version of this leaflet, please phone 01256 315000 (UK) or 01 661 4377 (Ireland)
RA040FSAA02
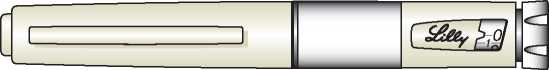
USER MANUAL
KwikPen™
Insulin delivery device
PLEASE READ THESE INSTRUCTIONS BEFORE USE
The KwikPen™ is designed for ease of use. It is a disposable pen containing 3 mL (300 units) of U-100 insulin. You can inject from 1 to 60 units of insulin in one injection. You can dial your dose one unit at a time. If you dial too many units, you can correct the dose without wasting any insulin.
Before using KwikPen, read the entire manual completely and follow the directions carefully. If you do not follow these directions completely, you may get too much or too little insulin.
Your KwikPen must be used only for your injections. Do not share your pen or your needles as this may risk transmission of infectious agents. Use a new needle for each injection.
DO NOT USE your pen if any part appears broken or damaged.
Always carry an extra pen in case yours is lost or damaged.
This pen is not recommended for use by the blind or visually impaired persons without the assistance of a person trained in the proper use of the product.
Important Notes
• Prime every time. The pen must be primed to a stream of insulin before each injection to make sure the pen is ready to dose.
• If you do not prime to a stream, you may get too much or too little insulin.
Frequently Asked Questions about Priming
• Why should I prime my pen before each dose?
1. Ensures that the pen is ready to dose.
2. Confirms that a stream of insulin comes out of the tip of the needle when you push the Dose Knob in.
3. Removes air that may collect in the needle or insulin cartridge during normal use.
• What should I do if I cannot completely push in the Dose Knob when priming KwikPen?
1. Attach a new needle.
2. Prime the pen.
• What should I do if I see an air bubble in the cartridge? You need to prime the pen. Remember, do not store the pen with the needle attached as this may cause air bubbles to collect in the insulin cartridge. A small air bubble will not affect your dose and you can continue to take your dose as usual.
Important Notes
• Read and follow the directions provided in the insulin package leaflet.
• Check the label on your pen before each injection for the expiration date and to make sure you are using the correct type of insulin. Do not remove the pen label.
Note: The colour of your KwikPen Dose Knob matches the insulin-specific colour band shown on the Pen Label. In this user manual, the Dose Knob is shown in grey. The Pen Body is beige to indicate that it contains a Humulin family of products.
Dose Knob Colour-code key:
|
o |
© |
O |
|
Humulin I |
Humulin M3 |
Humulin S |
• Your healthcare professional has prescribed the most appropriate type of insulin for you. Any changes in insulin therapy should be made only under medical supervision.
• KwikPen is recommended for use with Becton, Dickinson and Company (BD) pen needles.
• Be sure the needle is completely attached to the pen before use.
• Keep these directions for future reference.
Frequently Asked Questions about Preparing KwikPen
• What should my insulin look like? Some insulins are cloudy while others are clear, be sure to refer to your insulin package leaflet for the appearance of your specific insulin.
• What do I do if my dose is higher than 60 units? If your dose is higher than 60 units of insulin, multiple injections will be required or you may contact your healthcare professional.
• Why should I use a new needle for each injection? If needles are reused, you may get
the wrong amount of insulin, a clogged needle, a jammed pen, or an infection, because sterility is not ensured.
• What should I do if I am not sure how much insulin remains in my cartridge? Hold the pen with the needle end pointing down. The scale on the clear Cartridge Holder shows an estimate of the number of units remaining. These numbers should NOT be used for measuring an insulin dose.
• What should I do, if I can't remove the Pen Cap? Pull the cap straight off. If you are
having difficulty removing the cap, gently twist the cap back and forth to realign, and then pull the cap straight off.
Injecting Your Dose
Important Notes
• Follow the instructions for sanitary injection technique recommended by your healthcare professional.
• Make sure you receive your complete dose by pushing and holding the dose knob in and count to 5 slowly before removing the needle. If insulin is leaking from the pen you may not have held it in your skin long enough.
• A drop of insulin at the needle tip is normal. It will not affect your dose.
• The pen will not allow you to dial more than the number of units left in the pen.
• If you do not think you received your full dose, do not take another dose. Call your healthcare professional for assistance.
• If your dose is greater than the number of units left in the pen, you may either inject the amount remaining in your current pen and then use a new pen to complete your dose, OR inject the full dose with a new pen.
• Do not attempt to inject your insulin by turning the Dose Knob. You will NOT receive your insulin by turning the Dose Knob. You must PUSH the Dose Knob straight in for the dose to be delivered.
• Do not attempt to change the dose while injecting.
• The directions regarding needle handling are not intended to replace local, healthcare professional and/or institutional policies.
• Remove the needle after completing each injection.
Frequently Asked Questions about Injecting Your Dose
• Why is it difficult to push the Dose Knob when I try to inject?
1. Your needle may be clogged. Try attaching a new needle. When you do this you may see insulin come out of the needle. Then prime the pen.
2. Pressing the Dose Knob quickly may make the Dose Knob harder to push.
Pressing the Dose Knob more slowly may make it easier.
3. Using a larger diameter needle will make it easier to push the Dose Knob during your injection. See your healthcare professional to determine which needle size is best for you.
4. If the Dose Knob continues to be difficult to push after following the steps above, you may need a new pen.
• What should I do if my KwikPen is jammed? Your pen is jammed if it is difficult to inject a dose or dial a dose. To clear the jam:
1. Attach a new needle. When you do this you may see insulin come out of the needle.
2. Prime the pen.
3. Dial your dose and inject.
Do not attempt to lubricate your pen as this may damage the mechanism.
The Dose Knob may become harder to push, if foreign material (dirt, dust, food, insulin, or other liquids) get inside the pen. Avoid getting foreign material inside the pen.
• Why is insulin leaking from the needle after I finished my dose? You may have removed the needle from your skin too quickly.
1. Make sure you see a 0 in the Dose Window.
2. For the next dose, push and hold the Dose Knob in and count to 5 slowly before removing the needle.
• What should I do if my dose is dialled and the Dose Knob is accidentally pushed in without a needle attached?
1. Dial back to zero.
2. Attach a new needle.
3. Prime the pen.
4. Dial your dose and inject.
• What should I do if I dial a wrong dose (too high or too low)? Turn the Dose Knob backward or forward to correct the dose.
• What should I do if I see insulin leaking from the pen needle while dialling the dose or correcting the dose? Do not inject the dose because you may not get your complete dose. Dial the pen down to zero and prime the pen again (see Routine Use section "Priming KwikPen" steps 2B through 2D). Dial your dose and inject.
• What should I do if my full dose cannot be dialled? The pen will not allow you to dial a dose greater than the number of insulin units remaining in the cartridge. For example, if you need 31 units and only 25 units remain in the cartridge you will not be able to dial past 25. Do not attempt to dial past this point. If a partial dose remains in the pen you may either:
1. Give the partial dose and then give the remaining dose using a new pen.
or
2. Give the full dose with a new pen.
• Why can I not dial the dose to use the small amount of insulin that remains in my cartridge? The pen is designed to deliver at least 300 units of insulin. The pen design prevents the cartridge from being completely emptied because the small amount of insulin that remains cannot be delivered accurately.
Important Notes
• Before the first use store your pen in a refrigerator (2°C - 8°C). Do not use a pen if it has been frozen.
• Keep your pen in use at room temperature and away from heat and light.
• Do not store the pen with the needle attached. If the needle is left on, insulin may leak from the pen, insulin may dry inside the needle causing the needle to clog, or air bubbles may form in the cartridge.
• Refer to the package leaflet for complete insulin storage instructions.
• After first use the pen should not be used beyond the time specified in the insulin package leaflet.
• Dispose of used needles in a closable, puncture-resistant container, or as directed by your healthcare professional.
• Dispose of used pens as instructed by your healthcare professional and without the needle attached.
• Do not recycle the filled sharps container.
• Ask your healthcare professional about options available in your area to throw away the sharps container properly.
• The directions regarding needle handling are not intended to replace local, healthcare professional, or institutional policies.
• Keep the pen out of the reach of children.
If you have any questions or problems with your KwikPen, contact your healthcare
professional for assistance.
Make sure you have the following items:
□ KwikPen □ New Pen Needle □ Alcohol Swab
KwikPen and Needle* Assembly *sold separately
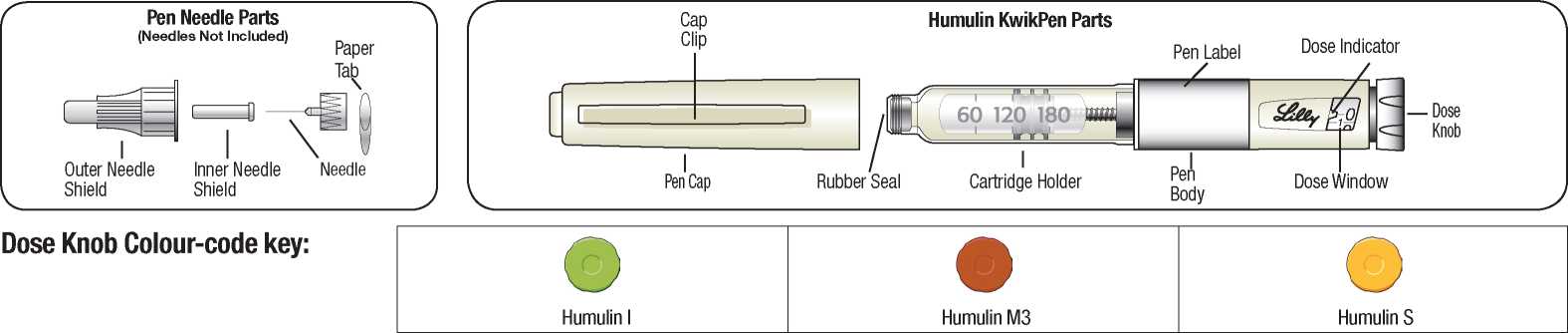
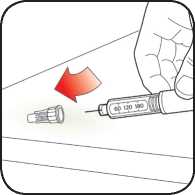
Pull Pen Cap straight off to remove. Do not twist the cap. Do not remove the Pen Label.
Be sure to check your insulin for:
• Type
• Expiration date
• Appearance
Caution: Always read the Pen Label to ensure you are using the correct insulin type.

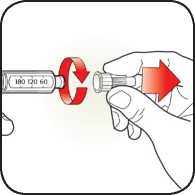
For Cloudy Insulin only:
Gently roll the pen 10 times.
AND
Invert the pen 10 times. Mixing is important to make sure you get the right dose. The insulin should look evenly mixed.
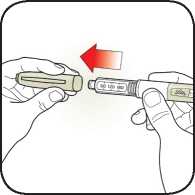
Select a new needle.
Remove paper tab from Outer Needle Shield.
Use an alcohol swab to wipe the Rubber Seal on the end of the Cartridge Holder.
Caution: If you do not prime to a stream before each injection, you may get too much or too little insulin.

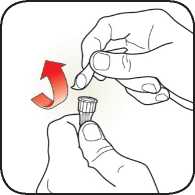
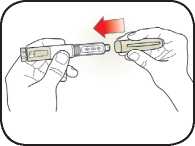
Pull off Outer Needle Shield. Do not throw away.
Pull off Inner Needle Shield and throw away.
Knob.

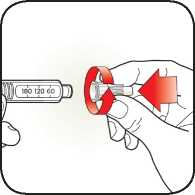
Point pen up.
Tap Cartridge Holder to collect air at top.
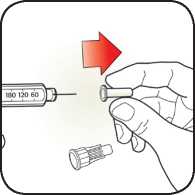
Push capped needle straight onto the pen.
Screw needle on until secure.

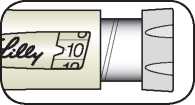
With needle pointed up, push Dose Knob in until it stops and 0 is seen in the Dose Window.
Hold Dose Knob in and count to 5 slowly.
Priming is complete when a stream of insulin appears from the needle tip.
If a stream of insulin does not appear, repeat priming steps 2B through 2D up to four times.
Note: If you do not see a stream of insulin from the needle tip and dialling the pen is more difficult, change the needle and prime the pen.
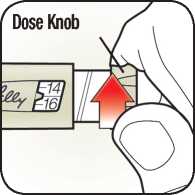
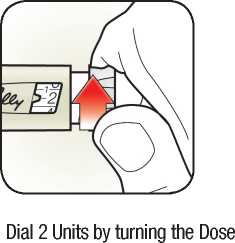
Turn Dose Knob to the number of units you need to inject. If you dial too many units, you can correct the dose by dialling backwards.
Example: 10 units shown.
Example: 15 units shown.
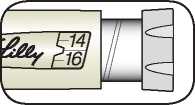
The even numbers are printed on the dial. The odd numbers, after the number one, are shown as full lines.
Manual revision date: July 2013. RA040FSM02

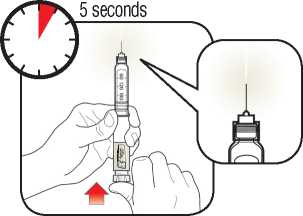
Insert needle into skin using injection technique recommended by your healthcare professional.
Place your thumb on the Dose Knob and push firmly until the Dose Knob stops moving.
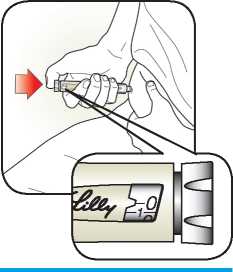
To deliver the full dose, hold Dose Knob in and count to 5 slowly.

Remove needle from skin.
Note: Check to make sure you see 0 in the Dose Window to confirm you received the complete dose.
Note: The pen will not allow you to dial more than the number of units left in the pen. If you do not think you received your full dose, do not take another dose.
Carefully replace the Outer Needle Shield.
Note: Remove the needle after each injection to keep air out of the cartridge. Do not store the pen with the needle attached.
Unscrew the capped needle and throw away as directed by your healthcare professional.
Replace Pen Cap by aligning the Cap Clip with the Dose Window and pushing straight on.