Humulin S Kwikpen 100 Iu/Ml Solution For Injection
Package leaflet: Information for the user HUMULIN® S (Soluble) KwikPen™ 100 IU/ml solution for injection
(Insulin human)
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1. What Humulin S KwikPen is and what it is used for
2. What you need to know before you use Humulin S KwikPen
3. How to use Humulin S KwikPen
4. Possible side effects
5. How to store Humulin S KwikPen
6. Contents of the pack and other information
1. What Humulin S KwikPen is and what it is used for
Humulin S KwikPen is a pre-filled pen containing the active substance human insulin, which is used to treat diabetes. You get diabetes if your pancreas does not make enough insulin to control the level of glucose in your blood (blood sugar). Humulin S is used to control glucose in the long term. Humulin S is a rapidly acting insulin preparation.
Your doctor may tell you to use Humulin S KwikPen as well as a longer-acting insulin. Each kind of insulin comes with its own patient information leaflet to tell you about it. Do not change your insulin unless your doctor tells you to. Be very careful if you do change insulin. Each type of insulin has a different colour and symbol on the pack and the pen so that you can easily tell the difference.
2. What you need to know before you use Humulin S KwikPen Do not use Humulin S KwikPen:
- If you think hypoglycaemia (low blood sugar) is starting. Further in this leaflet it tells you how to deal with mild hypoglycaemia (see A in Section 4).
- If you are allergic to human insulin or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist or nurse before using Humulin S KwikPen
• If your blood sugar levels are well controlled by your current insulin therapy, you may not feel the warning symptoms when your blood sugar is falling too low. Warning signs are listed later in this leaflet. You must think carefully about when to have your
meals, how often to exercise and how much to do. You must also keep a close watch on your blood sugar levels by testing your blood glucose often.
• A few people who have had hypoglycaemia (low blood sugar) after switching from animal insulin to human insulin have reported that the early warning symptoms were less obvious or different. If you often have hypoglycaemia or have difficulty recognising the symptoms, please discuss this with your doctor.
• If you answer YES to any of the following questions, tell your diabetes specialist nurse, doctor or pharmacist.
- Have you recently become ill?
- Do you have trouble with your kidneys or liver?
- Are you exercising more than usual?
• The amount of insulin you need may also change if you drink alcohol.
• You should also tell your diabetes specialist nurse, doctor or pharmacist if you are planning to go abroad. The time difference between countries may mean that you have to have your injections and meals at different times to when you are at home.
• Some patients with long-standing type 2 diabetes mellitus and heart disease or previous stroke who were treated with pioglitazone and insulin experienced the development of heart failure. Inform your doctor as soon as possible, if you experience signs of heart failure such as unusual shortness of breath or rapid increase in weight or localised swelling (oedema).
Other medicines and Humulin S KwikPen
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
Your insulin needs may change if you are taking any of the following:
• steroids,
• thyroid hormone replacement therapy,
• oral hypoglycaemics (antidiabetic medication),
• acetylsalicylic acid (aspirin),
• growth hormone,
• octreotide, lanreotide,
• beta2 stimulants (for example ritodrine, salbutamol or terbutaline),
• beta-blockers,
• thiazides or some antidepressants (monoamine oxidase inhibitors),
• danazol,
• some angiotensin converting (ACE) inhibitors (for example captopril, enalapril) or angiotensin II receptor blockers.
Pregnancy, breast-feeding and fertility
The amount of insulin you need usually falls during the first three months of pregnancy and increases for the remaining six months. If you are breast-feeding, you may need to alter your insulin intake or diet.
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Driving and using machines
Your ability to concentrate and react may be reduced if you have hypoglycaemia (low blood sugar). Please remember this in all situations where you might put yourself and others at risk (e.g. driving a car or operating machinery). You should contact your diabetes specialist nurse or doctor about the advisability of driving if you have:
frequent episodes of hypoglycaemia
reduced or absent warning signs of hypoglycaemia.
3. How to use Humulin S KwikPen
Always check the pack and the label of the pre-filled pen for the name and type of the insulin when you get it from your pharmacy. Make sure you get the Humulin KwikPen that your doctor has told you to use.
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure. To prevent the possible transmission of disease, each pen must be used by you only, even if the needle is changed.
Dosage
• Your doctor has told you which insulin to use, how much, when and how often to inject. These instructions are only for you. Follow them exactly and visit your diabetes clinic regularly.
• If you change your insulin type (for example from animal to human), you may have to take more or less than before. This might just be for the first injection or it may be a gradual change over several weeks or months.
• Inject Humulin S under the skin. You should only inject it into a muscle if your doctor has told you to.
Preparing Humulin S KwikPen
• Humulin S is already dissolved in water, so you do not need to mix it. But you must use it only if it looks like water. It must be clear, have no colour and no solid particles in it. Check each time you inject yourself.
Getting the KwikPen ready to use (Please see user manual)
• First wash your hands.
• Read the instructions on how to use your pre-filled insulin pen. Please follow the instructions carefully. Here are some reminders.
- Use a clean needle. (Needles are not included).
- Prime your KwikPen before each use. This checks that insulin comes out and clears the air bubbles from your KwikPen. There may still be some small air bubbles left in the KwikPen - these are harmless, but if the air bubble is too big, it may make the dose of your injection less accurate.
Injecting Humulin S KwikPen
• Before you make an injection, clean your skin as you have been instructed. Inject under the skin, as you were taught. Do not inject directly into a vein. After your injection, leave the needle in the skin for 5 seconds to make sure you have taken the whole dose. Do not rub the area you have just injected. Make sure you inject at least half an inch
(1 cm) from where you last injected and that you ‘rotate’ the places you inject, as you have been taught.
• You must not inject Humulin S KwikPen into a vein. Inject Humulin S KwikPen as your diabetes specialist nurse or doctor has taught you. Only your doctor can inject Humulin S KwikPen into a vein. He or she will only do this under special circumstances such as surgery or if you are ill and your glucose levels are too high.
After injecting
• As soon as you have done the injection, unscrew the needle from the KwikPen using the outer needle cap. This will keep the insulin sterile and prevent leaking. It will also
stop air going back into the KwikPen and the needle clogging up. Do not share your needles or your KwikPen. Replace the cap on the KwikPen.
Further injections
• Every time you use a KwikPen you must use a new needle. Before every injection, clear any air bubbles. You can see how much insulin is left by holding the KwikPen with the needle pointing down. The scale on the cartridge shows about how many units you have left.
• Do not mix any other insulin in your disposable KwikPen. Once the KwikPen is empty, do not use it again. Please get rid of it carefully - your diabetes specialist nurse or pharmacist will tell you how to do this.
If you use more Humulin S than you should
If you use more Humulin S than you should, your blood sugar may become low. Check your blood sugar (see A in section 4).
If you forget to use Humulin S KwikPen
If you use less Humulin S than you should, your blood sugar levels may increase. Check your blood sugar. Do not inject a double dose to make up for a forgotten dose.
If you stop using Humulin S KwikPen
If you use less Humulin S than you should, your blood sugar levels may become too high. Do not change your insulin unless your doctor tells you to.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Human insulin may cause hypoglycaemia (low blood sugar). See more information on hypoglycaemia below in the subsection “Common problems of diabetes”.
Possible side effects
Systemic allergy is very rare (affects less than 1 person in 10,000). The symptoms are as follows:
• fall in blood pressure • rash over the whole body
• difficulty in breathing • wheezing
• fast heart beat • sweating
If you think you are having this sort of insulin allergy with Humulin S, tell your doctor at once.
Local allergy is common (affects less than 1 person in 10). Some people get redness, swelling or itching around the area of the insulin injection. This usually clears up in anything from a few days to a few weeks. If this happens to you, tell your doctor.
Lipodystrophy (thickening or pitting of the skin) is uncommon (affects less than 1 person in 100). If you notice your skin thickening or pitting at the injection site, change your injection site and tell your doctor.
Oedema (e.g. swelling in arms, ankles; fluid retention) has been reported, particularly at the start of insulin therapy or during a change in therapy to improve control of your blood glucose.
Common problems of diabetes
A. Hypoglycaemia
Hypoglycaemia (low blood sugar) means there is not enough sugar in the blood. This can be caused if you:
• take too much Humulin S or other insulin;
• miss or delay meals or change your diet;
• exercise or work too hard just before or after a meal;
• have an infection or illness (especially diarrhoea or vomiting);
• have a change in your need for insulin; or
• have trouble with your kidneys or liver which gets worse.
Alcohol and some medicines can affect your blood sugar levels.
The first symptoms of low blood sugar usually come on quickly and include the following:
• tiredness • rapid heartbeat
• nervousness or shakiness • feeling sick
• headache • cold sweat
Until you become confident in recognising your warning symptoms, avoid situations such as driving a car, in which you or others would be put at risk by hypoglycaemia.
Do not use Humulin S if you think hypoglycaemia (low blood sugar) is starting.
If your blood sugar is low, eat glucose tablets, sugar or drink a sugary drink. Then eat fruit, biscuits, or a sandwich, as your doctor has advised you and have some rest. This will often get you over mild hypoglycaemia or a minor insulin overdose. If you get worse and your breathing is shallow and your skin gets pale, tell your doctor at once. A glucagon injection can treat quite severe hypoglycaemia. Eat glucose or sugar after the glucagon injection. If you do not respond to glucagon, you will have to go to hospital. Ask your doctor to tell you about glucagon.
B. Hyperglycaemia and diabetic ketoacidosis
Hyperglycaemia (too much sugar in the blood) means that your body does not have enough insulin. Hyperglycaemia can be brought about by:
• not taking your Humulin or other insulin;
• taking less insulin than your doctor tells you to;
• eating a lot more than your diet allows; or
• fever, infection or emotional stress.
Hyperglycaemia can lead to diabetic ketoacidosis. The first symptoms come on slowly over many hours or days. The symptoms include the following:
• feeling sleepy • no appetite
• flushed face • fruity smell on the breath
• thirst • feeling or being sick
Severe symptoms are heavy breathing and a rapid pulse. Get medical help immediately.
If hypoglycaemia (low blood sugar) or hyperglycaemia (high blood sugar) are not treated they can be very serious and cause headaches, nausea, vomiting, dehydration, unconsciousness, coma or even death.
Three simple steps to avoid hypoglycaemia or hyperglycaemia are:
• Always keep spare syringes and a spare vial of Humulin S.
• Always carry something to show you are diabetic.
• Always carry sugar with you.
C. Illness
If you are ill, especially if you feel sick or are sick, the amount of insulin you need may change. Even when you are not eating normally, you still need insulin. Test your urine or blood, follow your ‘sick rules’, and tell your diabetes specialist nurse or doctor.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via United Kingdom: Yellow Card Scheme, website: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Humulin S KwikPen
Keep this medicine out of the sight and reach of children.
Before the first use store your Humulin S KwikPen in a refrigerator (2°C - 8°C). Do not freeze. Keep your ‘in use’ Humulin S KwikPen at room temperature (below 30°C) for up to 28 days. Do not keep your ‘in use’ pen in the fridge. Do not put it near heat or in the sun.
Do not use this medicine after the expiry date which is stated on the label and the carton. The expiry date refers to the last day of that month.
Do not use this medicine if you notice it is coloured or it has solid particles in it. You must use it only if it looks like water. Check this each time you inject yourself.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help to protect the environment.
6. Contents of the pack and other information What Humulin S KwikPen contains
- The active substance is human insulin. Human insulin is made in the laboratory by a ‘recombinant DNA technology’ process. It has the same structure as the natural hormone made by the pancreas. It is therefore different from animal insulins.
- The other ingredients are metacresol, glycerol and water for injection. Sodium hydroxide or hydrochloric acid may have been used during manufacture to adjust the acidity.
What Humulin S KwikPen looks like and contents of the pack
Humulin S (Soluble) KwikPen 100 IU/ml, solution for injection is a sterile, clear, colourless, aqueous solution and contains 100 units of insulin in each millilitre (100 IU/ml).
Each Humulin S KwikPen contains 300 units (3 millilitres).
The Humulin S KwikPen comes in a pack of 5.
Not all pack sizes may be marketed.
The Humulin S in your KwikPen is the same as the Humulin S, which comes in separate Humulin S cartridges. The KwikPen simply has a built in cartridge. When the KwikPen is empty you cannot use it again.
Marketing Authorisation Holder and Manufacturer
Humulin S KwikPen is made by: Lilly France S.A.S., Rue du Colonel Lilly, 67640 Fegersheim, France.
The marketing authorisation is held by: Eli Lilly and Company Limited, Lilly House, Priestley Road, Basingstoke, Hampshire, RG24 9NL, U.K.
It is distributed in the Republic of Ireland by Eli Lilly and Company (Ireland) Limited, Hyde House, 65 Adelaide Road, Dublin 2, Ireland.
This medicinal product is authorised in the Member States of the EEA under the following names:
Huminsulin „Lilly“ Normal 100 I.E./ml - KwikPen (Austria)
Humuline Regular KwikPen (Belgium, Luxembourg)
Huminsulin Normal KwikPen (Germany)
Humulina Regular KwikPen (Spain)
Humulin S KwikPen (Ireland and UK)
Umuline Rapide KwikPen (France)
Humulin (Regular) KwikPen (Greece)
This leaflet was last revised in May 2016
If you would like a large-print version of this leaflet, please phone 01256 315000 (UK) or 01 661 4377 (Ireland)
Humulin® S KwikPen™ 100 IU/ml
PLEASE READ THIS USER MANUAL BEFORE USE
Read the User Manual before you start taking Humulin and each time you get another Humulin KwikPen 100 IU/ml. There may be new information. This information does not take the place of talking to your healthcare professional about your medical condition or your treatment.
Humulin KwikPen 100 IU/ml (“Pen”) is a disposable pre-filled pen containing 300 units (3 ml) of insulin. You can give yourself multiple doses using one Pen. The Pen dials 1 unit at a time. You can give from 1 to 60 units in a single injection. If your dose is more than 60 units, you will need to give yourself more than one injection. The plunger only moves a little with each injection, and you may not notice that it moves. The plunger will only reach the end of the cartridge when you have used all 300 units in the Pen.
Do not share your Pen with other people, even if the needle has been changed. Do not reuse or share needles with other people. You may give an infection to them or get an infection from them.
This Pen is not recommended for use by the blind or visually impaired without the help of someone trained to use the Pen.
KwikPen Parts
Cap Clip
Cartridge Holder
Label Dose Indicator
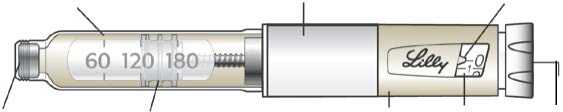
Pen Body Dose Dose Window Knob
Pen Cap Rubber Seal Plunger
Pen Needle Parts
(Needles Not Included)
Paper Tab
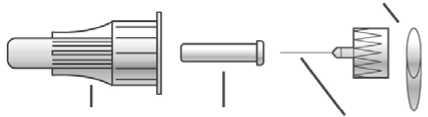
Outer Needle Inner Needle Needle
Shield Shield
How to recognise your Humulin KwikPen 100 IU/ml:
|
Humulin S | |
|
Pen Body colour: |
Beige |
|
Dose Knob: |
( ) |
|
Labels: |
White with Yellow-Gold Colour Bar |
Supplies needed to give your injection:
• Humulin KwikPen 100 IU/ml containing your insulin
• Humulin KwikPen 100 IU/ml compatible Needle (BD [Becton, Dickinson and Company] Pen Needles recommended)
• Alcohol swab
Preparing your Pen
• Follow the instructions for sanitary injection technique recommended by your healthcare professional.
• Check the Pen to make sure you are taking the right type of insulin. This is especially important if you use more than one type of insulin.
• Do not use your Pen past the expiration date printed on the Label or for more than 28 days after you first start using the Pen.
• Always use a new Needle for each injection to help prevent infections and blocked Needles.
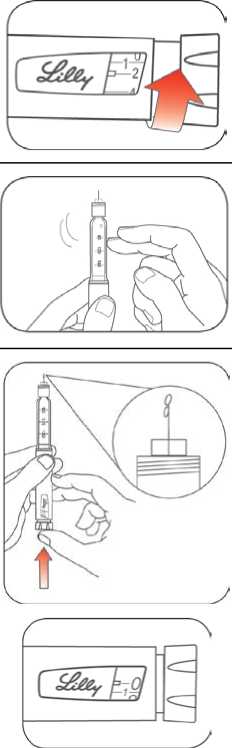
Step 1:
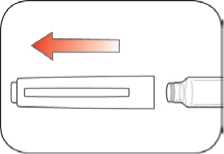
• Pull the Pen Cap straight off.
- Do not remove the Pen Label.
• Wipe the Rubber Seal with an alcohol swab.
Step 2:
• Check the appearance of the insulin.
- HUMULIN S should look clear and colourless. Do not use if it is cloudy, coloured, or has particles or clumps in it.
Step 3:
• Select a new Needle.
• Pull off the Paper Tab from the Outer Needle Shield.
Step 4:
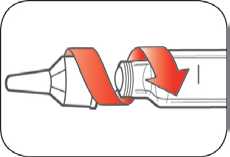
• Push the capped Needle straight onto the Pen and twist the Needle on until it is tight.
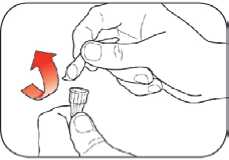
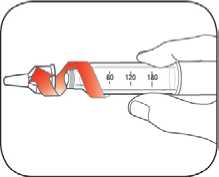
Step 5:
• Pull off the Outer Needle Shield. Do not throw it away.
• Pull off the Inner Needle Shield and throw it away.
Priming your Pen Prime before each injection.
• Priming your Pen means removing the air from the Needle and Cartridge that may collect during normal use and ensures that the Pen is working correctly.
• If you do not prime before each injection, you may get too much or too little insulin.
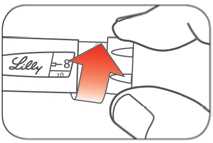
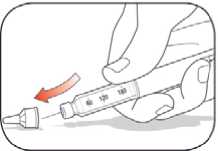
Step 6:
• To prime your Pen, turn the Dose Knob to select 2 units.
Step 7:
• Hold your Pen with the Needle
pointing up. Tap the Cartridge Holder gently to collect air bubbles at the top.
Step 8:
• Continue holding your Pen with Needle pointing up. Push the Dose Knob in until it stops, and “0” is seen in the Dose Window. Hold the Dose Knob in and count to 5 slowly.
You should see insulin at the tip of the Needle.
- If you do not see insulin, repeat the priming steps, but not more than 4 times.
- If you still do not see insulin, change the Needle and repeat the priming steps.
Small air bubbles are normal and will not affect your dose._
Selecting your dose
• You can give from 1 to 60 units in a single injection.
• If your dose is more than 60 units, you will need to give more than one injection.
- If you need help deciding how to divide up your dose, ask your healthcare professional.
- You should use a new Needle for each injection and repeat the priming step.
Step 9:
• Turn the Dose Knob to select the
number of units you need to inject.
The Dose Indicator should line up
with your dose.
- The Pen dials 1 unit at a time.
- The Dose Knob clicks as you turn it.
- DO NOT dial your dose by counting the clicks because you may dial the wrong dose.
- The dose can be corrected by turning the Dose Knob in either direction until the correct dose lines up with the Dose Indicator.
- The even numbers are printed on the dial.
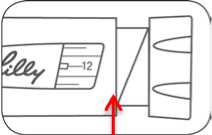
(Example: 12 units shown in the Dose Window)
- The odd numbers, after the number 1, are shown as full lines.
• Always check the number in the Dose Window to make sure you have dialed the correct dose.
(Example: 25 units shown in the Dose Window)
• The Pen will not let you dial more than the number of units left in the Pen.
• If you need to inject more than the number of units left in the Pen, you may either:
- inject the amount left in your Pen and then use a new Pen to give the rest of your dose, or
- get a new Pen and inject the full dose.
• It is normal to see a small amount of insulin left in the Pen that you cannot inject.
Giving your injection
• Inject your insulin as your healthcare professional has shown you.
• Change (rotate) your injection site for each injection.
Do not try to change your dose while injecting.
Step 10:
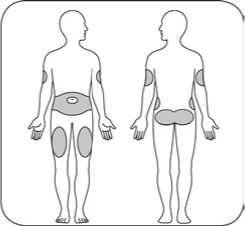
• Choose your injection site.
Humulin is injected under the skin (subcutaneously) of your stomach area, buttocks, upper legs or upper arms.
• Wipe your skin with an alcohol swab, and let your skin dry before you inject your dose.
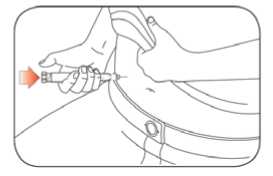
Step 11:
• Insert the Needle into your skin.
• Push the Dose Knob all the way in.

• Continue to hold the Dose Knob in and slowly count to 5 before removing the Needle.
Do not try to inject your insulin by turning the Dose Knob. You will NOT receive your insulin by turning the Dose Knob.
Step 12:
• Pull the Needle out of your skin.
- A drop of insulin at the Needle tip is normal. It will not affect your dose.
• Check the number in the Dose Window
- If you see “0” in the Dose window, you have received the full amount you dialed.
- If you do not see “0” in the Dose window, do not redial. Insert the needle into your skin and finish your injection.
- If you still do not think you received the full amount you dialed for your injection, do not start over or repeat that injection. Monitor your blood glucose as instructed by your healthcare professional.
- If you normally need to give 2 injections for your full dose, be sure to give your second injection.
The plunger only moves a little with each
injection, and you may not notice that it
moves.
If you see blood after you take the Needle out of your skin, press the injection site lightly with a piece of gauze or an alcohol swab. Do not rub the area.
After your injection

Step 13:
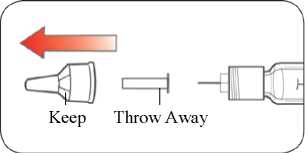
• Carefully replace the Outer Needle Shield.
Step 14:
• Unscrew the capped Needle and dispose of it as described below (see Disposing of Pens and Needles section).
• Do not store the Pen with the
Needle attached to prevent leaking, blocking the Needle, and air from entering the Pen._
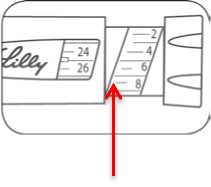
Step 15:
• Replace the Pen Cap by lining up the Cap Clip with the Dose Indicator and pushing straight on.
Disposing of Pens and Needles
• Put used Needles in a sharps container or a hard plastic container with a secure lid. Do not throw needles directly into your household trash.
• The used Pen may be discarded in your household trash after you have removed the Needle.
• Do not recycle the filled sharps container.
• Ask your healthcare professional about options to dispose of the sharps container properly.
• The directions regarding needle handling are not intended to replace local, healthcare professional or institutional policies.
Storing your Pen Unused Pens
• Store unused Pens in the refrigerator at 2°C to 8°C.
• Do not freeze Humulin. Do not use if it has been frozen.
• Unused Pens may be used until the expiration date printed on the Label, if the Pen has been kept in the refrigerator.
In-use Pen
• Store the Pen you are currently using at room temperature (up to 30°C) and away from heat and light.
• Throw away the Pen you are using after 28 days, even if it still has insulin left in it. General information about the safe and effective use of your Pen
• Keep your Pen and Needles out of the sight and reach of children.
• Do not use your Pen if any part looks broken or damaged.
• Always carry an extra Pen in case yours is lost or damaged.
Troubleshooting
• If you cannot remove the Pen Cap, gently twist the cap back and forth, and then pull the cap straight off.
• If the Dose Knob is hard to push:
- Pushing the Dose Knob more slowly will make it easier to inject.
- Your Needle may be blocked. Put on a new Needle and prime the Pen.
- You may have dust, food, or liquid inside the Pen. Throw the Pen away and get a new Pen.
If you have any questions or problems with your Humulin KwikPen, call your healthcare professional for help or contact your local Lilly affiliate.
Document Revision Date: May 2016
14