Hypoloc 5Mg Tablets
Package leaflet: Information for the user
HYPOLOC 5 mg tablets Nebivolol
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects talk to your doctor or pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1. What Hypoloc is and what it is used for
2. What you need to know before you take Hypoloc
3. How to take Hypoloc
4. Possible side effects
5. How to store Hypoloc
6. Contents of the pack and other information
1. What Hypoloc is and what it is used for
Hypoloc contains nebivolol, a cardiovascular drug belonging to the group of selective betablocking agents (i.e. with a selective action on the cardiovascular system). It prevents increased heart rate, controls heart pumping strength. It also exerts a dilating action on blood vessels, which contributes as well to lower blood pressure.
It is used to treat raised blood pressure (hypertension).
Hypoloc is also used to treat mild and moderate chronic heart failure in patients aged 70 or over, in addition to other therapies.
2. What you need to know before you take Hypoloc Do not take Hypoloc
• if you are allergic to nebivolol or any of the other ingredients of this medicine (listed in section 6).
• if you have one or more of the following disorders:
- low blood pressure
- serious circulation problems in the arms or legs
- very slow heartbeat (less than 60 beats per minute)
- certain other serious heart rhythm problems (e.g. 2nd and 3rd degree atrioventricular block, heart conduction disorders).
- heart failure, which has just occurred or which has recently become worse, or you are receiving treatment for circulatory shock due to acute heart failure by intravenous drip feed to help your heart work
- asthma or wheezing (now or in the past)
- untreated phaeochromocytoma, a tumour located on top of the kidneys (in the adrenal glands)
- liver function disorder
- a metabolic disorder (metabolic acidosis), for example, diabetic ketoacidosis.
Warnings and precautions
Talk to your doctor or pharmacist before taking Hypoloc.
Inform your doctor if you have or develop one of the following problems:
- abnormally slow heartbeat
- a type of chest pain due to spontaneously occurring heart cramp called Prinzmetal angina
- untreated chronic heart failure
- 1st degree heart block (a kind of light heart conduction disorder that affects heart rhythm)
- poor circulation in the arms or legs, e.g. Raynaud’s disease or syndrome, cramp-like pains when walking
- prolonged breathing problems
- diabetes: This medicine has no effect on blood sugar, but it could conceal the warning signs of a low sugar level (e.g. palpitations, fast heartbeat).
- overactive thyroid gland: This medicine may mask the signs of an abnormally fast heart rate due to this condition
- allergy: This medicine may intensify your reaction to pollen or other substances you are allergic to
- psoriasis (a skin disease - scaly pink patches) or if you have ever had psoriasis
- if you have to have surgery, always inform your anaesthetist that you are on Hypoloc before being anaesthetised.
If you have serious kidney problems do not take Hypoloc for heart failure and tell your doctor.
You will be regularly monitored at the beginning of your treatment for chronic heart failure by an experienced physician (see section 3).
This treatment should not be stopped abruptly unless clearly indicated and evaluated by your doctor (see section 3).
Children and adolescents
Because of the lack of data on the use of the product in children and adolescents, Hypoloc is not recommended for use in them.
Other medicines and Hypoloc
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
Always tell your doctor if you are using or receiving any of the following medicines in addition to Hypoloc:
- Medicines for controlling the blood pressure or medicines for heart problems (such as amiodarone, amlodipine, cibenzoline, clonidine, digoxin, diltiazem, disopyramide, felodipine, flecainide, guanfacin, hydroquinidine, lacidipine, lidocaine, methyldopa, mexiletine, moxonidine, nicardipine, nifedipine, nimodipine, nitrendipine, propafenone, quinidine, rilmenidine, verapamil).
- Sedatives and therapies for psychosis (a mental illness) e.g. barbiturates (also used for epilepsy), phenothiazine (also used for vomiting and nausea) and thioridazine.
- Medicines for depression e.g. amitriptyline, paroxetine, fluoxetine.
- Medicines used for anaesthesia during an operation.
- Medicines for asthma, blocked nose or certain eye disorders such as glaucoma (increased pressure in the eye) or dilation (widening) of the pupil.
- Baclofen (an antispasmodic drug); Amifostine (a protective medicine used during cancer treatment)
All these drugs as well as nebivolol may influence the blood pressure and/or heart function.
- Medicines for treating excessive stomach acid or ulcers (antacid drug), e.g. cimetidine: you should take Hypoloc during a meal and the antacid drug between meals.
Hypoloc with food and drink
Please refer to section 3.
Pregnancy and breast-feeding
Hypoloc should not be used during pregnancy, unless clearly necessary.
It is not recommended for use while breast-feeding.
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby,
ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
This medicine may cause dizziness or fatigue. If affected, do not drive or operate machinery.
Hypoloc contains lactose
This product contains lactose. If you have been told by your doctor that you have an intolerance
to some sugars, contact your doctor before taking this medicine.
3. How to take Hypoloc
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
Hypoloc may be taken before, during or after the meal, but, alternatively, you can take it independently of meals. The tablet is best taken with some water.
Treatment of raised blood pressure (hypertension)
- The usual dose is 1 tablet per day. The dose should be taken preferably at the same time of the day.
- Elderly patients and patients with a kidney disorder will usually start with ^ (half) tablet daily.
- The therapeutic effect on blood pressure becomes evident after 1-2 weeks of treatment. Occasionally, the optimal effect is reached only after 4 weeks.
Treatment of chronic heart failure
- Your treatment will be started and closely supervised by an experienced physician.
- Your doctor will start your treatment with H (quarter) tablet per day. This may be increased after 1-2 weeks to ^ (half) tablet per day, then to 1 tablet per day and then to 2 tablets per day until the correct dose is reached for you. Your doctor will prescribe the dose that is right for you at each step and you should closely follow his/her instructions.
- The maximum recommended dose is 2 tablets (10mg) a day.
- You will need to be under the close supervision for 2 hours by an experienced physician when you start treatment and every time your dose is increased
- Your doctor may reduce your dose if necessary
- You should not stop treatment abruptly as this can make your heart failure worse.
- Patients with serious kidney problems should not take this medicine.
- Take your medicine once daily, preferably at about the same time of day.
If you have been told by your doctor to take H (quarter) or ^ (half) tablet daily, please refer to the instructions below on how to break Hypoloc 5 mg cross-scored tablets.
• Place the tablets onto a flat, hard surface (e.g. a table or worktop), with the cross score facing
up.
• Break the tablet by pushing it with the index fingers of both hands placed along one breakmark (Diagrams 1 and 2).
• Tablet quarters are obtained by breaking the halves in the same way (Diagrams 3 and 4).
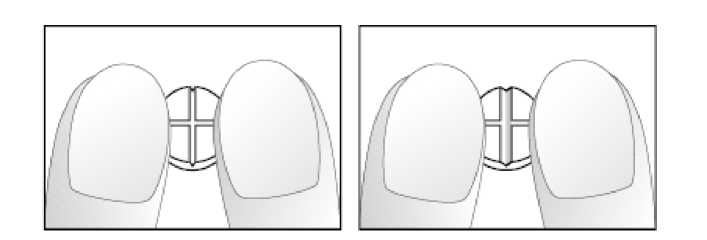
Diagrams 1 and 2: Easy breaking of the Nebivolol 5 mg cross-scored tablet in half.
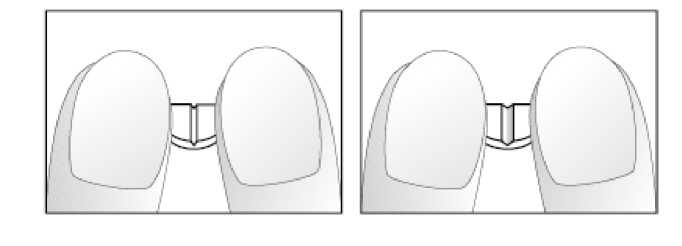
Diagrams 3 and 4: Easy breaking of half of the Nebivolol 5 mg cross-scored tablet into quarters.
- Your doctor may decide to combine Hypoloc tablets with other medicines to treat your condition.
Do not use in children or adolescents.
If you take more Hypoloc than you should
If you accidentally take an overdose of this medicine, tell your doctor of pharmacist immediately. The most frequent symptoms and signs of a Hypoloc overdose are very slow heart beat (bradycardia), low blood pressure with possible fainting (hypotension), breathlessness such as in asthma (bronchospasm), and acute heart failure.
You can take activated charcoal (which is available at your pharmacy) while you wait for the arrival of the doctor.
If you forget to take Hypoloc
If you forget a dose of Hypoloc, but remember a little later on that you should have taken it, take that day’s dose as usual. However, if a long delay has occurred (e.g. several hours), so that the next due dose is near, skip the forgotten dose and take the next, scheduled, normal dose at the usual time. Do not take a double dose. Repeated skipping, however, should be avoided.
If you stop taking Hypoloc
You should always consult with your doctor before stopping Hypoloc treatment, whether you are taking it for high blood pressure or chronic heart failure.
You should not stop Hypoloc treatment abruptly as this can temporarily make your heart failure worse. If it is necessary to stop Hypoloc treatment for chronic heart failure, the daily dose should be decreased gradually, by halving the dose, at weekly intervals.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
When Hypoloc is used for the treatment of raised blood pressure, the possible side effects are:
Common side effects (may affect up to 1 in 10 people):
- headache
- dizziness
- tiredness
- an unusual itching or tingling feeling
- diarrhoea
- constipation
- nausea
- shortness of breath
- swollen hands or feet.
Uncommon side effects (may affect up to 1 in 100 people):
- slow heartbeat or other heart complaints
- low blood pressure
- cramp-like leg pains on walking
- abnormal vision
- impotence
- feelings of depression
- digestive difficulties (dyspepsia), gas in stomach or bowel, vomiting
- skin rash, itchiness
- breathlessness such as in asthma, due to sudden cramps in the muscles around the airways (bronchospasm)
- nightmares.
Very rare side effects (may affect up to 1 in 10,000 people):
- fainting
- worsening of psoriasis (a skin disease - scaly pink patches).
The following side effects have been reported only in some isolated cases during Hypoloc treatment:
- whole-body allergic reactions, with generalised skin eruption (hypersensitivity reactions);
- rapid-onset swelling, especially around the lips, eyes, or of the tongue with possible sudden difficulty breathing (angioedema);
- kind of skin rash notable for pale red, raised, itchy bumps of allergic or non allergic causes (urticaria).
In a clinical study for chronic heart failure, the following side effects were seen:
Very common side effects (may affect more than 1 in 10 people):
- slow heart beat
- dizziness
Common side effects (may affect up to 1 in 10 people):
- worsening of heart failure
- low blood pressure (such as feeling faint when getting up quickly)
- inability to tolerate this medicine
- a kind of light heart conduction disorder that affects heart rhythm (1st degree AV-block)
- swelling of the lower limbs (such as swollen ankles).
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme. Website: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Hypoloc
Keep this medicine out of the sight and reach of children.
This medicinal product does not require any special storage conditions. Do not use this medicine after the expiry date which is stated on the carton label and blister foil after EXP. The expiry date refers to the last day of that month.
Do not throw any medicine via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help to protect the environment.
6. Contents of the pack and other information What Hypoloc contains
- The active substance is nebivolol. Each tablet contains 5 mg nebivolol (as nebivolol hydrochloride): 2.5 mg of d-nebivolol and 2.5 mg of l-nebivolol.
- The other ingredients are: lactose monohydrate, polysorbate 80 (E433), hypromellose (E464), maize starch, croscarmellose sodium (E468), microcrystalline cellulose (E460), silica colloidal anhydrous (E551), magnesium stearate (E572).
What Hypoloc looks like and contents of the pack
Hypoloc is available as white, round, cross-scored tablets in packs of 7, 14, 28, 30, 50, 56, 90, 100, 500 tablets. Tablets are provided in blister packs (PVC/aluminium blister).
(Not all pack sizes may be marketed)
Marketing Authorisation Holder and Manufacturer
Marketing Authorisation Holder
Menarini International Operations Luxembourg S.A.
1, Avenue de la Gare L-1611 Luxembourg Luxembourg
Manufacturer
Berlin-Chemie AG
Glienicker Weg 125, 12489 Berlin, Germany or
Menarini - von Heyden GmbH
Leipziger Strasse 7-13, 01097 - Dresden, Germany
or
Qualiphar N.V.
Rijksweg 9, 2880 Bornem, Belgium
Marketed by
A. Menarini Farmaceutica Internazionale SRL
This medicinal product is authorised in the Member States of the EEA under the following names:
Austria: Hypoloc Belgium: Nobiten Cyprus: Lobivon Denmark: Hypoloc Finland: Hypoloc France: Temerit Germany: Nebilet
Greece: Lobivon Ireland: Hypoloc Italy: Nebilox Iceland: Hypoloc Luxembourg: Nobiten Norway: Hypoloc Portugal: Nebilet Spain: Lobivon Sweden: Hypoloc The Netherlands: Nebilet United Kingdom: Hypoloc
This leaflet was last revised in 12/2014.
8