Innohep 10 000 Iu/Ml
Out of date information, search anotherPACKAGE LEAFLET: INFORMATION FOR THE USER
INNOHEP 10,000 lU/ml SYRINGE
(tinzaparin sodium)
The name of your medicine is Innohep 10,000 lU/ml Syringe but will be referred to as Innohep throughout this leaflet.
Please read all of this leaflet carefully before you start having this medicine.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If any of the side effects become serious, or you notice any side effects not listed in this leaflet please tell your doctor or pharmacist.
In this leaflet:
1. What Innohep is and what it is used for
2. Before you have Innohep
3. How to use Innohep
4. Possible side effects
5. How to store Innohep
6. Further information
1. What Innohep is and what it is used for
Innohep belongs to a group of medicines called anticoagulants. It is a type of heparin called a low molecular weight heparin.
Innohep changes the way your blood clots. This means your blood keeps flowing smoothly inside your blood vessels. These are the tubes that carry blood around your body and are called arteries and veins.
Innohep is used to help stop:
• Harmful blood clots forming in your veins following an operation. An example is a clot in a vein deep inside your body. This is usually in your leg (deep vein thrombosis or DVT for short).
• Harmful blood clots forming in the tubing of an artificial kidney machine during kidney dialysis (haemodialysis).
2. Before you have Innohep
Do not have Innohep
• If you are allergic (hypersensitive) to tinzaparin or any of the other ingredients in your medicine. You can find a list of these ingredients in section 6 of this leaflet.
• If you know that you have, or have ever had, a big drop in the clotting cells (platelets) in your blood, caused by having any type of heparin (reaction called heparin-induced thrombocytopenia).
• If you have any condition which makes you bleed severely, such as haemophilia.
• If you have very high blood pressure.
• If you have severe liver problems.
• If you have a stomach ulcer.
• If you know that you have a condition called endocarditis (an inflammation of the lining of the heart and heart valves).
• If you have had a brain haemorrhage (bleeding inside your brain).
• If you have an injury to your spine, head, eyes or ears.
• If you have recently had, or are about to have an operation involving your spine, head, eyes or ears.
• If you may be having a miscarriage.
Important: If you are having an epidural or spinal anaesthetic
You must remind your doctor that you are having Innohep before you receive any anaesthetic.
If you are pregnant please also read the section of this leaflet "Pregnancy and breast-feeding".
After you have the anaesthetic your doctor or nurse will make regular checks. This is to check if you are getting any major bleeding or bruising around your spine. This may cause paralysis that could be permanent.
Any signs this may be happening to you include tingling, weakness or numbness in your lower legs or body, back pain or problems in going to the toilet. This happens very rarely.
After you have the anaesthetic your doctor will tell you when you can take your medicine again.
Take special care with Innohep Before you have Innohep tell your doctor:
• If you have any condition which makes you more likely to bleed more easily. Ask your doctor if you are unsure.
• If you are allergic (hypersensitive) to heparin.
• If you are allergic to other low molecular weight heparins, such as enoxaparin or dalteparin.
• If you have kidney problems. Your doctor may need to adjust your dose.
• If you know you have a condition called diabetes mellitus.
• If you know you have a condition called metabolic acidosis.
• If you know you have any medical condition which may cause high levels of potassium in your blood (hyperkalaemia). Ask your doctor if you are unsure.
• If you are taking a medicine from the group called potassium-sparing diuretics, such as amiloride or spironolactone. These are commonly called water tablets.
• If you are taking another medicine that may affect your blood clotting.
For a list of these medicines see the section "Taking other medicines".
• If you have an artificial heart valve.

Your doctor may take a blood test before you start having this medicine, and while you are having it. This is to check the level of the clotting cells (platelets) and potassium in your blood.
This medicine may make you bleed more easily.
The doctor or nurse should take care when giving you any other injections or procedures.
This medicine must not be injected into your muscles.
Taking other medicines
Please tell your doctor or pharmacist if you are taking, or have recently taken any other medicines. This includes any medicines which you have bought without a prescription.
You must tell your doctor or pharmacist if you are taking any of the following medicines:
• Non-steroidal anti-inflammatory drugs, such as ibuprofen or diclofenac: for arthritis or aches or pains. You may be likely to bleed more easily.
• Salicylates, such as aspirin: for reducing pain and inflammation, or for stopping harmful blood clots forming. You may be likely to bleed more easily.
• Platelet aggregation inhibitors, such as clopidogrel: for stopping harmful blood clots forming. You may be likely to bleed more easily.
• Thrombolytic agents, such as streptokinase: for dissolving blood clots. You may be likely to bleed more easily.
• Vitamin K antagonists, such as warfarin: for stopping harmful blood clots. You may be likely to bleed more easily.
• Activated protein C: for getting rid of blood clots. You may be likely to bleed more easily.
• Dextrans: for increasing your blood volume. You may be likely to bleed more easily.
Pregnancy and breast-feeding
Please ask your doctor or pharmacist for advice before having Innohep:
• If you are pregnant, or think you are pregnant.
• If you are breast-feeding.
Tell your doctor if you become pregnant while having this medicine.
You must not have an epidural anaesthetic to help with your labour if you are having Innohep
Driving and using machines
Usually your medicine may have little effect on your ability to drive or use machines. However, you should check with your doctor if you feel any side effect that may stop you from driving or using machines.
Important information about some of the ingredients of Innohep
Innohep contains:
• Sodium. This medicine is nearly "sodium free". Your medicine contains less than 23 milligrams (mg) of sodium per dose.
Please ask your doctor if you are worried about any of the ingredients in this medicine.
3. Howto use Innohep
Innohep is usually given to you by a doctor or nurse. Innohep should not be mixed with any other injection.
How much Innohep to have
Your doctor will prescribe the right dose for you.
To prevent harmful blood clots forming in the tubing of an artificial kidney machine during kidney dialysis (haemodialysis)
Innohep will be given either into the artificial kidney machine or into your vein.
The usual dose depends on the length of dialysis.
To prevent harmful blood clots forming in your veins after an operation
Your doctor may decide that you or a carer may inject this medicine.
Your doctor or nurse will show you how to inject yourself with the syringe. Only inject yourself if you have been instructed how.
The usual dose depends on the type of operation you are having.
You will have one dose of Innohep before your operation. Then usually you will have one dose of Innohep once a day for 7 to 10 days afterwards. Your doctor will decide how long you should have Innohep.
How to inject Innohep
This section explains how to inject yourself with the Innohep syringe.
Warning: Only give this injection to yourself after you have received instructions from your doctor or nurse.
Always use Innohep exactly as your doctor has told you. You should check with your doctor or nurse if you are not sure about anything.
Where to inject
This injection goes under your skin. This may be called SC (subcutaneous). The usual place to inject yourself is on the left or right side of your tummy. Choose a place at least 5 cm (2 inches) from the belly button. Avoid the shaded area shown in the picture.

Choose a place away from any scars or bruises. You
should change the side you inject on each day. Pick a
place on the opposite side from where your last injection
went.
How to give the injection
1. Wash your hands thoroughly. Dry your hands well.
2. Decide where you are going to inject.
3. Put all the equipment you will need somewhere convenient to reach on a clean surface.
4. Check the expiry date on the syringe label. Do not use the injection after the expiry date. The expiry date is the last day of that month.
5. Look at the liquid inside the syringe. If you can see the liquid is cloudy or that it has any particles you must not use it.
6. Sit or lie in a comfortable position so you can see your skin where the injection will go. You may find using pillows or cushions will help.
7. Clean and dry the area of the skin as you have been told to do.
8. Bend the coloured lid on the plastic container all the way back. This will let you pull the syringe out. Only use one syringe for each injection.
Never keep an opened one for later.
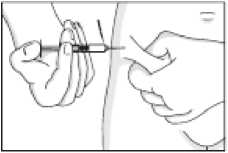
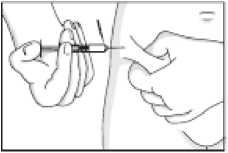
9. Bend the
orange coloured safety device down away from the cap on the needle.
10. Only pull the cap off the needle when you are ready to use the syringe. It is important to keep the needle clean. Do not let it touch anything.
11. You may notice a small air bubble in the syringe.
You do not need to remove this. The syringe is ready to use.
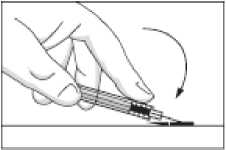
12. Hold the syringe in your writing hand like a pen.
13. Use your other hand to make a skin fold. Pinch your skin tight using your thumb and first finger. When you have made the skin fold keep holding on to it firmly.
14. It is important to hold your skin firmly until all the medicine has been injected. Hold the syringe upright with the needle pointing down. Push the needle down into the skin fold.
15. Press the plunger slowly down over 10-15 seconds.
All the liquid should come out of the syringe.
16. Pull the needle right out of your
skin. Then let go of the skin fold. The injection is complete.
17. Do not rub or massage the place where you have just put the injection. If you do this you may get a bruise.
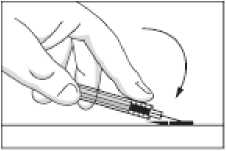
18. Bend the orange safety device back to its original position so it is now underneath the needle. Then with the safety device flat against a hard surface such as a table, push downwards until the needle clicks into the device. Now bend the safety device so that the needle and device are at a 45 degree angle to the syringe.
How to get rid of syringes safely
You should have a sharps bin. Put the used syringe carefully into your sharps bin as you have been told to do. Put the needle end in first. Keep it out of the reach and sight of children. When the bin is full give it to your nurse or pharmacist.
Never throw syringes into the household waste.
If you have more Innohepthan you should
Your doctor or nurse will usually give you this medicine, if you think you may have injected yourself with too much, or been given too much, tell your doctor or nurse straight away.
You may start to haemorrhage (bleed severely). Please read section 4 so you can spot any signs this may be happening to you.
You may be given another injection of a medicine called protamine sulphate.
If you have missed a dose of Innohep
Your doctor or nurse will usually give you this medicine. If you forget to inject yourself, or if you think that you have missed a dose, then tell your doctor or nurse.
If you have any further questions about using this medicine, please ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, Innohep can cause side effects, although not everybody gets them.
Important side effects to look out for You must get urgent medical help if you have any of the following symptoms. You may be getting an allergic reaction:
• You have difficulty breathing
• Your face or throat swell
• Your skin develops a severe rash
• Your skin develops blisters at the site of your injection
• Your skin peels.
You must get urgent medical help if you have any of the following symptoms after having an epidural or spinal anaesthetic. You may be developing paralysis:
• Tingling, weakness or numbness in your legs or lower body
• Back pain
• Problems in going to the toilet.
POM
You should tell your doctor straight away if you spot any of the following signs which mean you may be starting to bleed severely:
• Red or brown urine
• Black tarry stools
• Unusual bruising
• Bleeding from your nose, or mouth or any operation wound that will not stop.
Other possible side effects
The side effects most often reported are blood problems and skin reactions, especially where your injection has been given.
Very Common side effects (probably affect more than 1 in 10 people)
• Bleeding (haemorrhage). This may be more likely if you are taking a high dose of Innohep.
Common side effects (probably affect less than 1 in 10 people)
• Bruising, pain or irritation at the site of the injection
Uncommon side effects (probably affect less than 1 in 100 people)
• Rash
• Itchy skin
• Hives
• Headache
• Blood tests results may show changes in the way your liver is working
Side effects where the number of people affected is not known
• Changes in your blood test results. This may lead to bruising or bleeding more easily, because of a reaction in your blood. Your blood may form more harmful clots. A drop in the number of clotting cells (platelets) in your blood may give you these symptoms. Your doctor can explain this more.
• Changes in your blood test results. The amount of potassium may be increased. This is more likely to happen if you have severe kidney problems or diabetes. Your doctor can explain this more.
• Problems with your heart if you have an artificial heart valve. This may be because you are not having the dose of Innohep that is right for you.
• Your bones may weaken and break more easily.
This is known as osteoporosis and has been seen in patients taking heparin for a long time.
• Prolonged, painful erections in men.
If any of the side effects become serious, or if you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
Reporting of side effects If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.aov.uk/vellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Innohep
Keep out of the sight and reach of children.
Innohep should not be used after the expiry date which is stamped on the pack. The expiry date refers to the last day of that month.
Do not store above 25°C.
Medicines should not be thrown away in waste water or in household waste. Please ask your pharmacist how to throw away any medicine you do not need anymore. If you do this you will help protect the environment.
If the medicine becomes discoloured or shows any other signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.
6. Further Information
What Innohep contains
• The active ingredient is tinzaparin sodium. Each syringe contains 4,500 III of tinzaparin sodium in
0.45ml.
• The other ingredients are sodium acetate, sodium hydroxide solution and water for injections.
You can find important information about some of the ingredients near the end of section 2, just before section 3.
What Innohep looks like and contents of the pack
Clear solution, colourless to straw coloured, free of particles liquid in a glass prefilled unit dose syringe with a protective grey cap, an orange safety device and a blue plunger within a plastic protective tube with blue plastic tamper evident seal contained with a carton. There are 2 or 10 syringes in a carton.
Manufacturer
Manufactured by Laboratoires LEO S.A., 39 Route de Chartres, F-28500 Vernouillet, Cedex, France.
Procured from within the EU and repackaged in the UK by the Product Licence holder: CD Pharma Ltd, Unit 3, Manor Point, Manor Way, Borehamwood, Hertfordshire WD6 1 EE.
PL 20492/0491 Innohep 10,000 lU/ml Syringe
Innohep is a trademark of Leo Pharma A/S. Date of Preparation: 28th May 2014
PACKAGE LEAFLET: INFORMATION FOR THE USER
TINZAPARIN SODIUM 10,000 lU/ml SYRINGE
The name of your medicine is Tinzaparin sodium 10,000 lU/ml Syringe but will be referred to as Tinzaparin sodium throughout this leaflet.
Please read all of this leaflet carefully before you start having this medicine.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If any of the side effects become serious, or you notice any side effects not listed in this leaflet please tell your doctor or pharmacist.
In this leaflet:
1. What Tinzaparin sodium is and what it is used for
2. Before you have Tinzaparin sodium
3. How to use Tinzaparin sodium
4. Possible side effects
5. How to store Tinzaparin sodium
6. Further information
1. What Tinzaparin sodium is and what it is used for
Tinzaparin sodium belongs to a group of medicines called anticoagulants. It is a type of heparin called a low molecular weight heparin.
Tinzaparin sodium changes the way your blood clots. This means your blood keeps flowing smoothly inside your blood vessels. These are the tubes that carry blood around your body and are called arteries and veins.
Tinzaparin sodium is used to help stop:
• Harmful blood clots forming in your veins following an operation. An example is a clot in a vein deep inside your body. This is usually in your leg (deep vein thrombosis or DVT for short).
• Harmful blood clots forming in the tubing of an artificial kidney machine during kidney dialysis (haemodialysis).
2. Before you have Tinzaparin sodium
Do not have Tinzaparin sodium
• If you are allergic (hypersensitive) to tinzaparin or any of the other ingredients in your medicine. You can find a list of these ingredients in section 6 of this leaflet.
• If you know that you have, or have ever had, a big drop in the clotting cells (platelets) in your blood, caused by having any type of heparin (reaction called heparin-induced thrombocytopenia).
• If you have any condition which makes you bleed severely, such as haemophilia.
• If you have very high blood pressure.
• If you have severe liver problems.
• If you have a stomach ulcer.
• If you know that you have a condition called endocarditis (an inflammation of the lining of the heart and heart valves).
• If you have had a brain haemorrhage (bleeding inside your brain).
• If you have an injury to your spine, head, eyes or ears.
• If you have recently had, or are about to have an operation involving your spine, head, eyes or ears.
• If you may be having a miscarriage.
Important: If you are having an epidural or spinal anaesthetic
You must remind your doctor that you are having Tinzaparin sodium before you receive any anaesthetic.
If you are pregnant please also read the section of this leaflet "Pregnancy and breast-feeding".
After you have the anaesthetic your doctor or nurse will make regular checks. This is to check if you are getting any major bleeding or bruising around your spine. This may cause paralysis that could be permanent.
Any signs this may be happening to you include tingling, weakness or numbness in your lower legs or body, back pain or problems in going to the toilet. This happens very rarely.
After you have the anaesthetic your doctor will tell you when you can take your medicine again.
Take special care with Tinzaparin sodium Before you have Tinzaparin sodium tell your doctor:
• If you have any condition which makes you more likely to bleed more easily. Ask your doctor if you are unsure.
• If you are allergic (hypersensitive) to heparin.
• If you are allergic to other low molecular weight heparins, such as enoxaparin or dalteparin.
• If you have kidney problems. Your doctor may need to adjust your dose.
• If you know you have a condition called diabetes mellitus.
• If you know you have a condition called metabolic acidosis.
• If you know you have any medical condition which may cause high levels of potassium in your blood (hyperkalaemia). Ask your doctor if you are unsure.
• If you are taking a medicine from the group called potassium-sparing diuretics, such as amiloride or spironolactone. These are commonly called water tablets.
• If you are taking another medicine that may affect your blood clotting.
For a list of these medicines see the section "Taking other medicines".
• If you have an artificial heart valve.
Your doctor may take a blood test before you start having this medicine, and while you are having it. This is
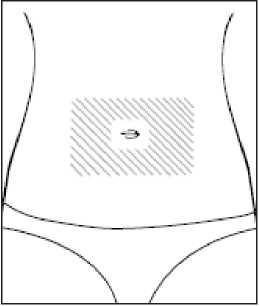
shown in the picture.
to check the level of the clotting cells (platelets) and potassium in your blood.
This medicine may make you bleed more easily.
The doctor or nurse should take care when giving you any other injections or procedures.
This medicine must not be injected into your muscles.
Taking other medicines
Please tell your doctor or pharmacist if you are taking, or have recently taken any other medicines. This includes any medicines which you have bought without a prescription.
You must tell your doctor or pharmacist if you are taking any of the following medicines:
• Non-steroidal anti-inflammatory drugs, such as ibuprofen or diclofenac: for arthritis or aches or pains. You may be likely to bleed more easily.
• Salicylates, such as aspirin: for reducing pain and inflammation, or for stopping harmful blood clots forming. You may be likely to bleed more easily.
• Platelet aggregation inhibitors, such as clopidogrel: for stopping harmful blood clots forming. You may be likely to bleed more easily.
• Thrombolytic agents, such as streptokinase: for dissolving blood clots. You may be likely to bleed more easily.
• Vitamin K antagonists, such as warfarin: for stopping harmful blood clots. You may be likely to bleed more easily.
• Activated protein C: for getting rid of blood clots. You may be likely to bleed more easily.
• Dextrans: for increasing your blood volume. You may be likely to bleed more easily.
Pregnancy and breast-feeding
Please ask your doctor or pharmacist for advice before having Tinzaparin sodium:
• If you are pregnant, or think you are pregnant.
• If you are breast-feeding.
Tell your doctor if you become pregnant while having this medicine.
You must not have an epidural anaesthetic to help with your labour if you are having Tinzaparin sodium
Driving and using machines
Usually your medicine may have little effect on your ability to drive or use machines. However, you should check with your doctor if you feel any side effect that may stop you from driving or using machines.
Important information about some of the ingredients of Tinzaparin sodium
Tinzaparin sodium contains:
• Sodium. This medicine is nearly "sodium free". Your medicine contains less than 23 milligrams (mg) of sodium per dose.
Please ask your doctor if you are worried about any of the ingredients in this medicine.
3. How to use Tinzaparin sodium
Tinzaparin sodium is usually given to you by a doctor or nurse.
Tinzaparin sodium should not be mixed with any other injection.
How much Tinzaparin sodium to have
Your doctor will prescribe the right dose for you.
To prevent harmful blood clots forming in the tubing of an artificial kidney machine during kidney dialysis (haemodialysis)
Tinzaparin sodium will be given either into the artificial kidney machine or into your vein.
The usual dose depends on the length of dialysis.
To prevent harmful blood clots forming in your veins after an operation
Your doctor may decide that you or a carer may inject this medicine.
Your doctor or nurse will show you how to inject yourself with the syringe. Only inject yourself if you have been instructed how.
The usual dose depends on the type of operation you are having.
You will have one dose of Tinzaparin sodium before your operation. Then usually you will have one dose of Tinzaparin sodium once a day for 7 to 10 days afterwards. Your doctor will decide how long you should have Tinzaparin sodium.
How to inject Tinzaparin sodium
This section explains how to inject yourself with the Tinzaparin sodium syringe.
Warning: Only give this injection to yourself after you have received instructions from your doctor or nurse.
Always use Tinzaparin sodium exactly as your doctor has told you. You should check with your doctor or nurse if you are not sure about anything.
Where to inject
This injection goes under your skin. This may be called SC (subcutaneous). The usual place to inject yourself is on the left or right side of your tummy. Choose a place at least 5 cm (2 inches) from the belly button. Avoid the shaded area

Choose a place away from any scars or bruises. You
should change the side you inject on each day. Pick a
place on the opposite side from where your last injection
went.
How to give the injection
1. Wash your hands thoroughly. Dry your hands well.
2. Decide where you are going to inject.
3. Put all the equipment you will need somewhere convenient to reach on a clean surface.
4. Check the expiry date on the syringe label. Do not use the injection after the expiry date. The expiry date is the last day of that month.
5. Look at the liquid inside the syringe. If you can see the liquid is cloudy or that it has any particles you must not use it.
6. Sit or lie in a comfortable position so you can see your skin where the injection will go. You may find using pillows or cushions will help.
7. Clean and dry the area of the skin as you have been told to do.
8. Bend the coloured lid on the plastic container all the way back. This will let you pull the syringe out. Only use one syringe for each injection.
Never keep an opened one for later.
9. Bend the
orange coloured safety device down away from the cap on the needle.
1 0. Only pull the cap off the needle when you are ready to use the syringe. It is important to keep the needle clean. Do not let it touch anything.
11. You may notice a small air bubble in the syringe.
You do not need to remove this. The syringe is ready to use.
12. Hold the syringe in your writing hand like a pen.
13. Use your other hand to make a skin fold. Pinch your skin tight using your thumb and first finger. When you have made the skin fold keep holding on to it firmly.
14. It is important to hold your skin firmly until all the medicine has been injected. Hold the syringe upright with the needle pointing down. Push the needle
down into the skin fold.
15. Press the plunger slowly down over 10-15 seconds.
All the liquid should come out of the syringe.
16. Pull the needle right out of your skin. Then let go of the skin fold. The injection is complete.
17. Do not rub or massage the place where you have just put the injection. If you do this you may get a bruise.
18. Bend the orange safety device back to its original position so it is now underneath the needle. Then with the safety device flat against a hard surface such as a table, push downwards until the needle clicks into the device. Now bend the safety device so that the needle and device are at a 45 degree angle to the syringe.
How to get rid of syringes safely
You should have a sharps bin. Put the used syringe carefully into your sharps bin as you have been told to do. Put the needle end in first. Keep it out of the reach and sight of children. When the bin is full give it to your nurse or pharmacist.
Never throw syringes into the household waste.
If you have more Tinzaparin sodium than you should
Your doctor or nurse will usually give you this medicine, if you think you may have injected yourself with too much, or been given too much, tell your doctor or nurse straight away.
You may start to haemorrhage (bleed severely). Please read section 4 so you can spot any signs this may be happening to you.
You may be given another injection of a medicine called protamine sulphate.
If you have missed a dose of Tinzaparin sodium
Your doctor or nurse will usually give you this medicine. If you forget to inject yourself, or if you think that you have missed a dose, then tell your doctor or nurse.
If you have any further questions about using this medicine, please ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, Tinzaparin sodium can cause side effects, although not everybody gets them.
Important side effects to look out for You must get urgent medical help if you have any of the following symptoms. You may be getting an allergic reaction:
• You have difficulty breathing
• Your face or throat swell
• Your skin develops a severe rash
• Your skin develops blisters at the site of your injection
• Your skin peels.
You must get urgent medical help if you have any of the following symptoms after having an epidural or spinal anaesthetic. You may be developing paralysis:
• Tingling, weakness or numbness in your legs or lower body
• Back pain
• Problems in going to the toilet.

You should tell your doctor straight away if you spot any of the following signs which mean you may be starting to bleed severely:
• Red or brown urine
• Black tarry stools
• Unusual bruising
• Bleeding from your nose, or mouth or any operation wound that will not stop.
Other possible side effects
The side effects most often reported are blood problems and skin reactions, especially where your injection has been given.
Very Common side effects (probably affect more than 1 in 10 people)
• Bleeding (haemorrhage). This may be more likely if you are taking a high dose of Tinzaparin sodium.
Common side effects (probably affect less than 1 in 10 people)
• Bruising, pain or irritation at the site of the injection
Uncommon side effects (probably affect less than 1 in 100 people)
• Rash
• Itchy skin
• Hives
• Headache
• Blood tests results may show changes in the way your liver is working
Side effects where the number of people affected is not known
• Changes in your blood test results. This may lead to bruising or bleeding more easily, because of a reaction in your blood. Your blood may form more harmful clots. A drop in the number of clotting cells (platelets) in your blood may give you these symptoms. Your doctor can explain this more.
• Changes in your blood test results. The amount of potassium may be increased. This is more likely to happen if you have severe kidney problems or diabetes. Your doctor can explain this more.
• Problems with your heart if you have an artificial heart valve. This may be because you are not having the dose of Tinzaparin sodium that is right for you.
• Your bones may weaken and break more easily.
This is known as osteoporosis and has been seen in patients taking heparin for a long time.
• Prolonged, painful erections in men.
If any of the side effects become serious, or if you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
Reporting of side effects If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.aov.uk/vellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Tinzaparin sodium
Keep out of the sight and reach of children.
Tinzaparin sodium should not be used after the expiry date which is stamped on the pack. The expiry date refers to the last day of that month.
Do not store above 25°C.
Medicines should not be thrown away in waste water or in household waste. Please ask your pharmacist how to throw away any medicine you do not need anymore. If you do this you will help protect the environment.
If the medicine becomes discoloured or shows any other signs of deterioration, you should seek the advice of your pharmacist who will tell you what to do.
6. Further Information
What Tinzaparin sodium contains
• The active ingredient is tinzaparin sodium. Each syringe contains 4,500 III of tinzaparin sodium in 0.45ml.
• The other ingredients are sodium acetate, sodium hydroxide solution and water for injections.
You can find important information about some of the ingredients near the end of section 2, just before section 3.
What Tinzaparin sodium looks like and contents of the pack
Clear solution, colourless to straw coloured, free of particles liquid in a glass prefilled unit dose syringe with a protective grey cap and a blue plunger within a plastic protective tube with blue plastic tamper evident seal contained with a carton.
There are 2 or 10 syringes in a carton.
Manufacturer
Manufactured by Laboratoires LEO S.A., 39 Route de Chartres, F-28500 Vernouillet, Cedex, France.
Procured from within the EU and repackaged in the UK by the Product Licence holder: CD Pharma Ltd, Unit 3, Manor Point, Manor Way, Borehamwood, Hertfordshire WD6 1 EE.
PL 20492/0491 Tinzaparin sodium 10,000 lU/ml
Date of Preparation: 28th May 2014