Itraconazole 10Mg/Ml Oral Solution
Out of date information, search another
Package leaflet: Information for the user Sporanox 10mg/ml Oral Solution
_(itraconazole)_
Your medicine is available as Sporanox 10mg/ml Oral Solution but will be referred to as Sporanox Oral Solution throughout the leaflet.
Read all of this leaflet carefully before you start taking your medicine:
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them even if their symptoms are the same as yours.
• If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
In this leaflet:
1. What Sporanox Oral solution is and what it is used for
2. Before you use Sporanox Oral Solution
3. How to use Sporanox Oral Solution
4. Possible side effects
5. How to store Sporanox Oral Solution
6. Further information
1. WHAT SPORANOX ORAL SOLUTION IS AND WHAT IT IS USED FOR
Sporanox is one of a group of medicines called "antifungals". These medicines are used to treat and stop you from getting infections caused by fungi including yeasts. You may be given Sporanox Oral Solution to:
• treat yeast infections of the mouth, throat or gullet if you have a poor immune system
• stop you from getting certain fungal infections if you have a poor immune system due to a major blood disorder or bone marrow transplantation.
2. BEFORE YOU USE SPORANOX ORAL SOLUTION Do not use Sporanox Oral Solution if you are:
• allergic (hypersensitive) to itraconazole or to any of the ingredients in Sporanox Oral Solution (listed in Section 6 Further information)
• pregnant, think you might be pregnant or could become pregnant (see the section on Pregnancy)
• taking any of the following medicines:
• terfenadine, astemizole or mizolastine (antihistamine for allergies)
• bepridil - used to treat angina (crushing chest pain)
• nisoldipine (used for high blood pressure)
• cisapride (used for stomach upsets)
• midazolam by mouth or triazolam (used to help you sleep or for anxiety)
• lovastatin, simvastatin or atorvastatin (used to lower cholesterol)
• pimozide and sertindole (for conditions affecting thoughts, feelings and/or behaviour)
• levacetylmethadol - for treatment of drug abuse (opioid dependency)
• dihydroergotamine, ergotamine and eletriptan (for migraine headaches)
• ergometrine (ergonovine) and methyl- ergometrine (methylergonovine) used after giving birth
• quinidine and dofetilide (for irregular heart beat rhythms).
Take special care with Sporanox Oral Solution
Stop taking Sporanox Oral Solution and see your doctor immediately if any of the following symptoms of severe liver problems appear during your course of treatment:
• Severe lack of appetite, feeling sick, being sick, unusual tiredness, abdominal (stomach) pain, unusually dark urine or pale stools.
Tell your doctor immediately:
• If you have any unusual feelings of tingling, numbness or weakness in your hands or feet whilst taking Sporanox Oral Solution.
• If you experience any hearing loss symptoms. In very rare cases patients taking Sporanox Oral Solution have reported temporary or permanent hearing loss
Tell your doctor if you have:
• had an allergic reaction to any other antifungal medicines
• a heart problem, including heart failure (also called congestive heart failure or CHF), Sporanox Oral Solution could make it worse. If your doctor decides to give you Sporanox Oral Solution, you should be told about the symptoms listed below to watch out for. If you get any of the following stop taking Sporanox Oral Solution and tell your doctor straight away. These may be signs of heart failure: - shortness of breath - unexpected weight gain - swelling of your legs or stomach - feel unusually tired - wake up short of breath at night
• a liver problem, such as jaundice (yellowing of the skin) as your dose of Sporanox Oral Solution may have to be changed. Your doctor should give you instructions on symptoms to watch out for.
If you have to take Sporanox Oral Solution continuously for more than one month, your doctor may want to check your liver by doing blood tests
• a kidney disorder as your dose of Sporanox Oral Solution may have to be changed.
Taking other medicines
There are some medicines that you should not take whilst taking Sporanox Oral Solution. These are listed under the heading "Do not use Sporanox Oral Solution if you are:"
Tell your doctor if you are using the following medicines as they may stop Sporanox Oral Solution from working properly:
• rifampicin, rifabutin and isoniazid (antibiotics used for tuberculosis)
• phenytoin, carbamazepine and phenobarbital (anti-epileptics)
• St John's wort Do not use Sporanox Oral Solution within 2 weeks of taking these medicines.
Tell your doctor before taking any of the following medicines as the dose of Sporanox Oral Solution or other treatments may need to be altered:
• clarithromycin and erythromycin (antibiotics for infections)
• medicines that act on the heart and blood vessels (digoxin, disopyramide and calcium channel-blockers such as dihydropyridines, verapamil and cilostazol)
• drugs that slow down blood clotting or thin the blood, such as warfarin
• methylprednisolone, budesonide fluticasone and dexamethasone, medicines given by mouth and injection for inflammation, asthma and allergies
• ciclosporin, tacrolimus and rapamycin (also known as sirolimus), which are usually given after an organ transplant
• medicines used in HIV-infected patients, such as ritonavir, indinavir and saquinavir
• medicines for cancer (such as busulphan, docetaxel, trimetrexate and a group of medicines known as vinca alkaloids)
• alfentanil and fentanyl (for pain)
• buspirone, alprazolam, brotizolam and midazolam when given by injection into a vein (for anxiety or to help you sleep)
• reboxetine (for depression)
• loperamide (for diarrhoea)
• an antihistamine containing ebastine
• halofantrine (for malaria)
• repaglinide (for diabetes)
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines,
including medicines obtained without a prescription.
Using Sporanox Oral Solution with food and drink
Do not take Sporanox Oral Solution with food or drink as it reduces your body's ability to absorb the medicine. Always take Sporanox Oral Solution one hour before any food or drink as this helps the body absorb the medicine.
Children and the elderly
Sporanox Oral Solution is not normally given to children or the elderly. Your doctor may prescribe it in special cases.
Pregnancy
Do not take Sporanox Oral Solution if you are pregnant, unless your doctor has told you to. If you are of child bearing age and could become pregnant, you should use contraceptives to make sure that you do not become pregnant while you are taking your medicine. As Sporanox Oral Solution remains in the body for some time after you stop taking it, you should continue to use some form of contraception until your next period after your treatment with Sporanox Oral Solution has finished. If you do find that you are pregnant after starting a course of Sporanox Oral Solution, stop taking it and tell your doctor straight away. Before taking any medicine - always tell your doctor if you are pregnant, think you might be pregnant or are trying to become pregnant.
Breast-feeding
If you are breast-feeding do not take Sporanox Oral Solution, as small amounts of the medicine could be present in your breast milk.
Driving and using machines
Sporanox Oral Solution can sometimes cause dizziness, blurred/double vision or hearing loss. If you have these symptoms, do not drive or use machines.
Important information about some of the ingredients of Sporanox Oral Solution
Tell your doctor if you are intolerant to fructose (a type of sugar) as this is in sorbitol, one of the ingredients of Sporanox Oral Solution.
3. HOW TO USE SPORANOX ORAL SOLUTION
Always take Sporanox Oral Solution one hour before any food or drink as this helps the body absorb the medicine. You should swish the Sporanox Oral Solution around in your mouth for approximately 20 seconds before swallowing it. Do not rinse your mouth after swallowing the Sporanox Oral Solution. Always take Sporanox Oral Solution exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. A measuring cup graduated to indicate 10ml is provided. Ensure you fill the cup to the 10 ml mark.
How to take Sporanox Oral Solution
• Treatment of yeast infections of the mouth, throat or gullet
The usual dose is 2 measuring cups (20 ml) per day for one week. This may be taken either all at once or in two divided doses during the day. If after one week of using Sporanox Oral Solution your infection has not cleared, your doctor may decide to continue your treatment for one more week.
• Treatment of yeast infections of the mouth, throat or gullet, that have already been treated with another antifungal but have still not cleared
The usual dose is 1-2 measuring cups (10-20 ml) twice daily for two weeks. The treatment may be continued for an additional two weeks, if the infection does not clear in the initial two weeks of treatment. For patients on the higher dose of 400mg (4 measuring cups) daily, treatment should be limited to 14 days, if there are no signs of improvement during this time.
• Prevention of fungal infections
The dose is calculated according to your body weight (5mg per kg) given in two divided doses.
Your doctor will tell you exactly how much you should take.
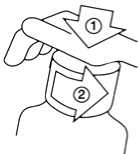
Directions for opening the bottle
The bottle comes with a child-proof cap, and should be opened as follows: push the plastic screw cap down, while turning it counter clockwise.
If you take too much Sporanox Oral Solution
If you, or anyone else, take more Sporanox Oral Solution than you were told to, contact your doctor or local hospital without delay.
If you forget to take Sporanox Oral Solution
If you forget to take your medicine, take the next dose as usual and continue your medicine as directed by your doctor. Do not take a double dose. If you have any further questions on the use of Sporanox Oral Solution, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Sporanox Oral Solution can cause side effects, although not everybody gets them.
Medicines can cause serious allergic reactions. Stop taking Sporanox Oral Solution and contact
your doctor immediately if you have:
• any sudden wheeziness, difficulty in breathing, swelling of the face, rash, itching (especially affecting the whole body) or a severe skin disorder (widespread rashes with peeling skin and blisters in the mouth, eyes and genitals, or rashes with small pustules or blisters).
• severe lack of appetite, feeling sick, being sick, unusual tiredness, abdominal (stomach) pain, unusually dark urine, or pale stools. These may be symptoms of severe liver problems. You should also let your doctor know immediately if you have any of the side effects below:
• Symptoms that resemble heart failure such as shortness of breath, unexpected weight gain, swelling of the legs, unusual fatigue (tiredness), repeated waking at night
• A tingling sensation, sensitivity to light, numbness or weakness in the limbs
• Blurred vision/double vision, ringing in your ears, lose the ability to control your urine or increased need to urinate (pass water)
• If you experience any hearing loss symptoms
Other side effects include:
Common side effects (occur in less than 1 in 10 patients) are:
• headache
• stomach ache, feeling sick (nausea), being sick (vomiting), diarrhoea, unpleasant taste
• increases in specific liver function tests (hepatic enzyme increased)
• rash
• fever or high temperature
• shortness of breath
Uncommon side effects (occur in less than 1 in 100 patients) are:
• certain blood disorders which may increase the risk of bleeding, bruising or infections
• muscle weakness (possible symptom of low blood levels of potassium)
• dizziness
• indigestion, constipation
• inflammation of the liver (hepatitis), yellowing of the skin (jaundice)
• itching
• general swelling
The following side effects have been reported in patients taking Sporanox Oral Solution with unknown frequency:
• excess of triglycerides in the blood
• hair loss
• muscle pain, painful joints
• menstrual disorders
• erectile dysfunction
• severe upper stomach pain, often with nausea and vomiting due to inflammation of the pancreas (pancreatitis)
If any of these side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. HOW TO STORE SPORANOX ORAL SOLUTION
Keep out of the sight and reach of children.
Do not store above 25°C.
Do not use the Sporanox Oral Solution after the expiry date printed on the packaging. The expiry date refers to the last day of that month.
The Sporanox Oral Solution should not be used for longer than 1 month after the bottle has first been opened. Always return any left over medicine to your pharmacist. Only keep it if your doctor tells you to.
If your medicine appears to be discoloured or show any other signs of deterioration please return to your pharmacist who will advise you further.
If your doctor tells you to stop taking the medicine, please take them back to the pharmacist for safe disposal. Only keep the medicine if your doctor tells you to.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. FURTHER INFORMATION
What Sporanox Oral Solution contains
• The active ingredient is itraconazole. Each ml contains 10mg itraconazole.
• The other ingredients are hydroxypropyl- p-cyclodextrin, hydrochloric acid, propylene glycol, sodium hydroxide, sodium saccharin dihydrate, sorbitol, cherry flavour 1, cherry flavour 2, caramel and purified water.
What Sporanox Oral Solution looks like and the contents of the pack
Sporanox Oral Solution is clear, yellow to slightly amber solution.
Your medicine is available in a amber glass bottle in packs of 150ml.
Manufacturer
Manufactured by: JANSSEN Pharmaceutica N.V., Turnhoutseweg 30, B-2340 Beerse, Belgium.
Procured from within the EU and repackaged by: Doncaster Pharmaceuticals Group Ltd., Kirk Sandall, Doncaster, DN3 1QR.
Product Licence holder: Landmark Pharma Ltd., 7 Regents Drive, Prudhoe, Northumberland, NE42 6PX.
POM
PL No: 21828/0625
Sporanox® is a registered trademark of Johnson & Johnson. Latest revision date: 14.01.15
Itraconazole 10mg/ml Oral Solution
Package leaflet: Information for the user
Your medicine is available as Itraconazole 10mg/ml Oral Solution but will be referred to as Itraconazole Oral Solution throughout the leaflet.
Read all of this leaflet carefully before you start taking your medicine:
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them even if their symptoms are the same as yours.
• If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
In this leaflet:
1. What Itraconazole Oral solution is and what it is used for
2. Before you use Itraconazole Oral Solution
3. How to use Itraconazole Oral Solution
4. Possible side effects
5. How to store Itraconazole Oral Solution
6. Further information
1. WHAT ITRACONAZOLE ORAL SOLUTION IS AND WHAT IT IS USED FOR
Itraconazole is one of a group of medicines called "antifungals". These medicines are used to treat and stop you from getting infections caused by fungi including yeasts. You may be given Itraconazole Oral Solution to:
• treat yeast infections of the mouth, throat or gullet if you have a poor immune system
• stop you from getting certain fungal infections if you have a poor immune system due to a major blood disorder or bone marrow transplantation.
2. BEFORE YOU USE ITRACONAZOLE ORAL SOLUTION Do not use Itraconazole Oral Solution if you are:
• allergic (hypersensitive) to itraconazole or to any of the ingredients in Itraconazole Oral Solution (listed in Section 6 Further information)
• pregnant, think you might be pregnant or could become pregnant (see the section on Pregnancy)
• taking any of the following medicines:
• terfenadine, astemizole or mizolastine (antihistamine for allergies)
• bepridil - used to treat angina (crushing chest pain)
• nisoldipine (used for high blood pressure)
• cisapride (used for stomach upsets)
• midazolam by mouth or triazolam (used to help you sleep or for anxiety)
• lovastatin, simvastatin or atorvastatin (used to lower cholesterol)
• pimozide and sertindole (for conditions affecting thoughts, feelings and/or behaviour)
• levacetylmethadol - for treatment of drug abuse (opioid dependency)
• dihydroergotamine, ergotamine and eletriptan (for migraine headaches)
• ergometrine (ergonovine) and methyl- ergometrine (methylergonovine) used after giving birth
• quinidine and dofetilide (for irregular heart beat rhythms).
Take special care with Itraconazole Oral Solution
Stop taking Itraconazole Oral Solution and see your doctor immediately if any of the following symptoms of severe liver problems appear during your course of treatment:
• Severe lack of appetite, feeling sick, being sick, unusual tiredness, abdominal (stomach) pain, unusually dark urine or pale stools.
Tell your doctor immediately:
• If you have any unusual feelings of tingling, numbness or weakness in your hands or feet whilst taking Itraconazole Oral Solution.
• If you experience any hearing loss symptoms. In very rare cases patients taking Itraconazole Oral Solution have reported temporary or permanent hearing loss
Tell your doctor if you have:
• had an allergic reaction to any other antifungal medicines
• a heart problem, including heart failure (also called congestive heart failure or CHF), Itraconazole Oral Solution could make it worse. If your doctor decides to give you Itraconazole Oral Solution, you should be told about the symptoms listed below to watch out for. If you get any of the following stop taking Itraconazole Oral Solution and tell your doctor straight away. These may be signs of heart failure: - shortness of breath - unexpected weight gain - swelling of your legs or stomach - feel unusually tired - wake up short of breath at night
• a liver problem, such as jaundice (yellowing of the skin) as your dose of Itraconazole Oral Solution may have to be changed. Your doctor should give you instructions on symptoms to watch out for. If you have to take Itraconazole Oral Solution continuously for more than one month, your doctor may want to check your liver by doing blood tests
• a kidney disorder as your dose of Itraconazole Oral Solution may have to be changed.
Taking other medicines
There are some medicines that you should not take whilst taking Itraconazole Oral Solution. These
are listed under the heading "Do not use Itraconazole Oral Solution if you are:"
Tell your doctor if you are using the following medicines as they may stop Itraconazole Oral
Solution from working properly:
• rifampicin, rifabutin and isoniazid (antibiotics used for tuberculosis)
• phenytoin, carbamazepine and phenobarbital (anti-epileptics)
• St John's wort Do not use Itraconazole Oral Solution within 2 weeks of taking these medicines.
Tell your doctor before taking any of the following medicines as the dose of Itraconazole Oral Solution or other treatments may need to be altered:
• clarithromycin and erythromycin (antibiotics for infections)
• medicines that act on the heart and blood vessels (digoxin, disopyramide and calcium channel-blockers such as dihydropyridines, verapamil and cilostazol)
• drugs that slow down blood clotting or thin the blood, such as warfarin
• methylprednisolone, budesonide fluticasone and dexamethasone, medicines given by mouth and injection for inflammation, asthma and allergies
• ciclosporin, tacrolimus and rapamycin (also known as sirolimus), which are usually given after an organ transplant
• medicines used in HIV-infected patients, such as ritonavir, indinavir and saquinavir
• medicines for cancer (such as busulphan, docetaxel, trimetrexate and a group of medicines known as vinca alkaloids)
• alfentanil and fentanyl (for pain)
• buspirone, alprazolam, brotizolam and midazolam when given by injection into a vein (for anxiety or to help you sleep)
• reboxetine (for depression)
• loperamide (for diarrhoea)
• an antihistamine containing ebastine
• halofantrine (for malaria)
• repaglinide (for diabetes)
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines obtained without a prescription.
Using Itraconazole Oral Solution with food and drink
Do not take Itraconazole Oral Solution with food or drink as it reduces your body's ability to absorb the medicine. Always take Itraconazole Oral Solution one hour before any food or drink as this helps the body absorb the medicine.
Children and the elderly
Itraconazole Oral Solution is not normally given to children or the elderly. Your doctor may prescribe it in special cases.
Pregnancy
Do not take Itraconazole Oral Solution if you are pregnant, unless your doctor has told you to. If you are of child bearing age and could become pregnant, you should use contraceptives to make sure that you do not become pregnant while you are taking your medicine. As Itraconazole Oral Solution remains in the body for some time after you stop taking it, you should continue to use some form of contraception until your next period after your treatment with Itraconazole Oral Solution has finished.
If you do find that you are pregnant after starting a course of Itraconazole Oral Solution, stop taking it and tell your doctor straight away. Before taking any medicine - always tell your doctor if you are pregnant, think you might be pregnant or are trying to become pregnant.
Breast-feeding
If you are breast-feeding do not take Itraconazole Oral Solution, as small amounts of the medicine could be present in your breast milk.
Driving and using machines
Itraconazole Oral Solution can sometimes cause dizziness, blurred/double vision or hearing loss. If you have these symptoms, do not drive or use machines.
Important information about some of the ingredients of Itraconazole Oral Solution
Tell your doctor if you are intolerant to fructose (a type of sugar) as this is in sorbitol, one of the ingredients of Itraconazole Oral Solution.
3. HOW TO USE ITRACONAZOLE ORAL SOLUTION
Always take Itraconazole Oral Solution one hour before any food or drink as this helps the body absorb the medicine. You should swish the Itraconazole Oral Solution around in your mouth for approximately 20 seconds before swallowing it. Do not rinse your mouth after swallowing the Itraconazole Oral Solution. Always take Itraconazole Oral Solution exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. A measuring cup graduated to indicate 10ml is provided. Ensure you fill the cup to the 10 ml mark.
How to take Itraconazole Oral Solution
• Treatment of yeast infections of the mouth, throat or gullet
The usual dose is 2 measuring cups (20 ml) per day for one week. This may be taken either all at once or in two divided doses during the day. If after one week of using Itraconazole Oral Solution your infection has not cleared, your doctor may decide to continue your treatment for one more week.
• Treatment of yeast infections of the mouth, throat or gullet, that have already been treated with another antifungal but have still not cleared
The usual dose is 1-2 measuring cups (10-20 ml) twice daily for two weeks. The treatment may be continued for an additional two weeks, if the infection does not clear in the initial two weeks of treatment. For patients on the higher dose of 400mg (4 measuring cups) daily, treatment should be limited to 14 days, if there are no signs of improvement during this time.
• Prevention of fungal infections
The dose is calculated according to your body weight (5mg per kg) given in two divided doses. Your doctor will tell you exactly how much you should take.
Directions for opening the bottle
The bottle comes with a child-proof cap, and should be opened as follows: push the plastic screw cap down, while turning it counter clockwise.
If you take too much Itraconazole Oral Solution
If you, or anyone else, take more Itraconazole Oral Solution than you were told to, contact your doctor or local hospital without delay.
If you forget to take Itraconazole Oral Solution
If you forget to take your medicine, take the next dose as usual and continue your medicine as directed by your doctor. Do not take a double dose. If you have any further questions on the use of Itraconazole Oral Solution, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Itraconazole Oral Solution can cause side effects, although not everybody gets
them.
Medicines can cause serious allergic reactions. Stop taking Itraconazole Oral Solution and contact
your doctor immediately if you have:
• any sudden wheeziness, difficulty in breathing, swelling of the face, rash, itching (especially affecting the whole body) or a severe skin disorder (widespread rashes with peeling skin and blisters in the mouth, eyes and genitals, or rashes with small pustules or blisters).
• severe lack of appetite, feeling sick, being sick, unusual tiredness, abdominal (stomach) pain, unusually dark urine, or pale stools. These may be symptoms of severe liver problems. You should also let your doctor know immediately if you have any of the side effects below:
• Symptoms that resemble heart failure such as shortness of breath, unexpected weight gain, swelling of the legs, unusual fatigue (tiredness), repeated waking at night
• A tingling sensation, sensitivity to light, numbness or weakness in the limbs
• Blurred vision/double vision, ringing in your ears, lose the ability to control your urine or increased need to urinate (pass water)
• If you experience any hearing loss symptoms
Other side effects include:
Common side effects (occur in less than 1 in 10 patients) are:
• headache
• stomach ache, feeling sick (nausea), being sick (vomiting), diarrhoea, unpleasant taste
• increases in specific liver function tests (hepatic enzyme increased)
• rash
• fever or high temperature
• shortness of breath
Uncommon side effects (occur in less than 1 in 100 patients) are:
• certain blood disorders which may increase the risk of bleeding, bruising or infections
• muscle weakness (possible symptom of low blood levels of potassium)
• dizziness
• indigestion, constipation
• inflammation of the liver (hepatitis), yellowing of the skin (jaundice)
• itching
• general swelling
The following side effects have been reported in patients taking Itraconazole Oral Solution with unknown frequency:
• excess of triglycerides in the blood
• hair loss
• muscle pain, painful joints
• menstrual disorders
• erectile dysfunction
• severe upper stomach pain, often with nausea and vomiting due to inflammation of the pancreas (pancreatitis)
If any of these side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. HOW TO STORE ITRACONAZOLE ORAL SOLUTION
Keep out of the sight and reach of children.
Do not store above 25°C.
Do not use the Itraconazole Oral Solution after the expiry date printed on the packaging. The expiry date refers to the last day of that month.
The Itraconazole Oral Solution should not be used for longer than 1 month after the bottle has first been opened. Always return any left over medicine to your pharmacist. Only keep it if your doctor tells you to.
If your medicine appears to be discoloured or show any other signs of deterioration please return to your pharmacist who will advise you further.
If your doctor tells you to stop taking the medicine, please take them back to the pharmacist for safe disposal. Only keep the medicine if your doctor tells you to.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. FURTHER INFORMATION
What Itraconazole Oral Solution contains
• The active ingredient is itraconazole. Each ml contains 10mg itraconazole.
• The other ingredients are hydroxypropyl- p-cyclodextrin, hydrochloric acid, propylene glycol, sodium hydroxide, sodium saccharin dihydrate, sorbitol, cherry flavour 1, cherry flavour 2, caramel and purified water.
What Itraconazole Oral Solution looks like and the contents of the pack
Itraconazole Oral Solution is clear, yellow to slightly amber solution.
Your medicine is available in an amber glass bottle in packs of 150ml.
Manufacturer
Manufactured by: JANSSEN Pharmaceutica N.V., Turnhoutseweg 30, B-2340 Beerse, Belgium.
Procured from within the EU and repackaged by: Doncaster Pharmaceuticals Group Ltd., Kirk Sandall, Doncaster, DN3 1QR.
Product Licence holder: Landmark Pharma Ltd., 7 Regents Drive, Prudhoe, Northumberland, NE42 6PX.
POM
PL No: 21828/0625
Latest revision date: 14.01.15
Page 2 of 2