Neoral 100 Mg/Ml Oral Solution
Package leaflet: Information for the patient
Neoral® 100 mg/ml Oral Solution
(ciclosporin)
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
What is in this leaflet
1. What Neoral is and what it is used for
2. What you need to know before you take Neoral
3. How to take Neoral
4. Possible side effects
5. How to store Neoral
6. Contents of the pack and other information
1. What Neoral is and what it is used for
What Neoral is
The name of your medicine is Neoral. It contains the active substance ciclosporin. This belongs to a group of medicines known as immunosuppressive agents.
These medicines are used to lower the body's immune reactions.
What Neoral is used for and how Neoral works
• If you have had an organ transplant, bone marrow and stem cell transplantation, the function of Neoral is to control your body's immune system. Neoral prevents rejection of transplanted organs by blocking the development of certain cells which would normally attack the transplanted tissue.
• If you have an autoimmune disease, in which your body's immune response attacks your body's own cells, Neoral stops this immune reaction. Such diseases include eye problems which threaten your vision (endogenous uveitis, including Behget's uveitis), severe cases of certain skin diseases (atopic dermatitis, or eczema and psoriasis), severe rheumatoid arthritis and a kidney disease called nephrotic syndrome.
2. What you need to know before you take Neoral
If you are taking Neoral following a transplant it will only be prescribed for you by a doctor with experience in transplants and/or autoimmune diseases.
The advice in this leaflet may vary depending on whether you are taking the medicine for a transplant or for an autoimmune disease.
Follow all your doctor's instructions carefully. They may differ from the general information contained in this leaflet.
Do not take Neoral:
- if you are allergic to ciclosporin or any of the other ingredients of this medicine (listed in section 6).
- with products containing Hypericum perforatum (St John's Wort).
- with products containing dabigatran etexilate (used to avoid blood clots after surgery) or bosentan and aliskiren (used to reduce high blood pressure).
Do not take Neoral and tell your doctor if the above applies to you. If you are not sure, talk to your doctor before taking Neoral.
Warnings and precautions
Before and during treatment with Neoral, tell your doctor straight away:
• if you have any signs of infection, such as fever or a sore throat. Neoral suppresses the immune system and may also affect your body's ability to fight against infection.
• if you have liver problems.
• if you have kidney problems. Your doctor will carry out regular blood tests and may change your dose if necessary.
• if you develop high blood pressure. Your doctor will check your blood pressure regularly and may give you a medicine to lower blood pressure if necessary.
• if you have low levels of magnesium in your body. Your doctor may give you magnesium supplements to take, especially just after your operation if you have had a transplant.
• if you have high levels of potassium in your blood.
• if you have gout.
• if you need to have a vaccination.
If any of the above applies to you before or during treatment with Neoral, tell your doctor straight away.
Sunlight and sun protection
Neoral suppresses your immune system. This increases your risk of developing cancers, particularly of the skin and lymphoid system. You should limit your exposure to sunlight and UV light by:
• Wearing appropriate protective clothing.
• Often applying a sunscreen with a high protection factor.
Talk to your doctor before taking Neoral:
• if you have or have had alcohol-related problems.
• if you have epilepsy.
• if you have any liver problems.
• if you are pregnant.
• if you are breast-feeding.
• if this medicine is being prescribed for a child.
If any of the above apply to you (or you are not sure), tell your doctor before taking Neoral. This is because this medicine contains alcohol (see section below “Neoral contains ethanol”).
Monitoring during your treatment with Neoral
Your doctor will check:
• the levels of ciclosporin in your blood, especially if you have had a transplant,
• your blood pressure before the start of your treatment and regularly during treatment,
• how well your liver and kidneys are working,
• your blood lipids (fats).
If you have any questions about how Neoral works or why this medicine has been prescribed for you, ask your doctor.
In addition if you are taking Neoral for a non-transplant disease (intermediary or posterior uveitis and Behget's uveitis, atopic dermatitis, severe rheumatoid arthritis or nephrotic syndrome), do not take Neoral:
• if you have kidney problems (except for nephrotic syndrome).
• if you have an infection which is not under control with medication.
• if you have any type of cancer.
• if you have high blood pressure (hypertension) which is not under control with medication. If you get high blood pressure during treatment and it cannot be controlled, Neoral should be stopped by your doctor.
Do not take Neoral if any of the above applies to you. If you are not sure, talk to your doctor or pharmacist before taking Neoral.
If you are being treated for Behget's uveitis, your doctor will monitor you particularly carefully if you have neurological symptoms (for example: increased forgetfulness, personality changes noticed over time, psychiatric or mood disorders, burning sensation in limbs, decreased sensation in limbs, tingling sensation in limbs, weakness of limbs, walking disturbances, headache with or without nausea and vomiting, vision disturbances including restricted movement of eyeball).
Your doctor will closely monitor you if you are elderly and are being treated for psoriasis or atopic dermatitis. If you have been prescribed Neoral to treat your psoriasis or atopic dermatitis, you must not be exposed to any UVB-rays or phototherapy during treatment.
Children and adolescents
Neoral should not be given to children for a non-transplant disease, except for treatment of nephrotic syndrome.
Elderly population (65 years of age and older)
There is limited experience with Neoral in elderly patients. Your doctor should monitor how well your kidneys work. If you are over 65 and have psoriasis or atopic dermatitis, you should only be treated with Neoral if your condition is particularly severe.
Other medicines and Neoral
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
In particular tell your doctor or pharmacist if you are taking any of the following medicines before or during Neoral treatment:
• Medicines that may affect your potassium levels. These include medicines which contain potassium, potassium supplements, water tablets (diuretics) called potassium-sparing diuretics and some medicines which lower your blood pressure.
• Methotrexate. This is used to treat tumours, severe psoriasis and severe rheumatoid arthritis.
• Medicines which may increase or decrease the level of ciclosporin (the active substance of Neoral) in your blood. Your doctor might check the level of ciclosporin in your blood when starting or stopping treatment with other medicines.
- Medicines which may increase the level of ciclosporin in your blood include: antibiotics (such as erythromycin or azythromycin), anti-fungals (voriconazole, itraconazole), medicines used for heart problems or high blood pressure (diltiazem, nicardipine, verapamil, amiodarone), metoclopramide (used to stop sickness), oral contraceptives, danazol (used to treat menstrual problems), medicines used to treat gout (allopurinol), cholic acid and derivatives (used to treat gallstones), protease inhibitors used to treat HIV, imatinib (used to treat leukaemia or tumours), colchicine, telaprevir (used to treat hepatitis C).
- Medicines which may decrease the level of ciclosporin in your blood include: barbiturates (used to help you to sleep), some anti-convulsant medicines (such as carbamazepine or phenytoine), octreotide (used to treat acromegaly or neuroendocrine tumours in the gut), anti-bacterial medicines used to treat tuberculosis, orlistat (used to help weight loss), herbal medicines containing St. John's wort, ticlopidine (used after a stroke), certain medicines which lower blood pressure (bosentan), and terbinafine (an anti-fungal medicine used to treat infections of the toes and nails).
• Medicines which may affect your kidneys. These include: anti-bacterial medicines (gentamycin, tobramycin, ciprofloxacin), anti-fungal medicines which contain amphotericin B, medicines used for urinary tract infections which contain trimethoprim, medicines for cancer which contain melphalan, medicines used to lower the amount of acid in your stomach (acid secretion inhibitors of the H2-receptor antagonist type), tacrolimus, pain killers (non-steroid anti-inflammatory medicines such as diclofenac), fibric acid medicines (used to lower the amount of fat in the blood).
• Nifedipine. This is used to treat high blood pressure and heart pain. You might get swollen gums that might grow over your teeth if you are taking nifedipine during your treatment with ciclosporin.
• Digoxin (used to treat heart problems), medicines which lower cholesterol (HMG-CoA reductase inhibitors also called statins), prednisolone, etoposide (used to treat cancer), repaglinide (oral anti-diabetic medicine), immunosuppressives (everolimus, sirolimus), ambrisentan and specific anti-cancer medicines called anthracyclines (such as doxorubicin).
If any of the above applies to you (or you are not sure), talk to your doctor or pharmacist before taking Neoral.
Neoral with food and drink
Do not take Neoral with grapefruit or grapefruit juice. This is because these can affect how Neoral works.
Pregnancy and breast-feeding
Ask your doctor or pharmacist for advice before taking this medicine. Your doctor will discuss with you the potential risks of taking Neoral during pregnancy.
• Tell your doctor if you are pregnant or intend to become pregnant.
Experience with Neoral in pregnancy is limited. In general, Neoral should not be taken during pregnancy. If it is necessary for you to take this medicine, your doctor will discuss with you the benefits and potential risks of taking it during pregnancy.
• Tell your doctor if you are breast-feeding. Breast-feeding is not recommended during treatment with Neoral. This is because ciclosporin, the active substance, passes into breast milk. This may affect your baby.
Driving and using machines
Neoral contains alcohol. This may affect your ability to drive and use machines. Neoral contains ethanol
Neoral contains approximately 12.0 vol. % ethanol (alcohol), which corresponds to up to 500 mg per dose used in transplant patients. This is equivalent to nearly 15 ml beer or 5 ml wine per dose.
Alcohol may be harmful if you have alcohol-related problems, epilepsy, brain injury, liver problems or if you are pregnant or breast-feeding. It may also be harmful if this medicine is given to children.
Neoral contains castor oil
Neoral contains castor oil, which may cause stomach discomfort and diarrhoea.
3. How to take Neoral
Always take this medicine exactly as your doctor has told you. Check with your doctor if you are not sure.
Do not take more than the recommended dose.
The dose of this medicine will be carefully adjusted to your individual needs by your doctor. Too much of the medicine can affect your kidneys. You will have regular blood tests and visits to the hospital, especially after a transplant. This will give you the chance to talk to your doctor about your treatment and talk about any problems you may be having.
How much Neoral to take
Your doctor will work out the correct dose of Neoral for you. This depends on your body weight and what you are taking the medicine for. Your doctor will also tell you how often to take your medicine.
• In adults:
Organ, bone marrow and stem cell transplantation
- The total dose each day is usually between 2 mg and 15 mg per kilogram body weight. This is divided in two doses.
- Usually, higher doses are used before and just after your transplant. Lower doses are used once your transplanted organ or bone marrow has stabilised.
- Your doctor will adjust your dose to one that is ideal for you. To do this, your doctor may need to do some blood tests.
Endogenous uveitis
- The total dose each day is usually between 5 mg and 7 mg per kilogram body weight. This is divided in two doses.
Nephrotic syndrome
- The total dose each day for adults is usually 5 mg per kilogram body weight.
This is divided in two doses. In patients with kidney problems, the first dose taken each day should not be more than 2.5 mg per kilogram body weight.
Severe rheumatoid arthritis
- The total dose each day is usually between 3 mg per kilogram of your body weight and 5 mg per kilogram body weight. This is divided in two doses.
Psoriasis and atopic dermatitis
- The total dose each day is usually between 2.5 mg per kilogram of your body weight and 5 mg per kilogram body weight. This is divided in two doses.
• In children:
Nephrotic syndrome
- The total dose each day for children is usually 6 mg per kilogram body weight. This is divided in two doses. In patients with kidney problems, the first dose taken each day should not be more than 2.5 mg per kilogram body weight. Follow your doctor's instructions exactly and never change the dose yourself, even if you feel well.
Switch from Sandimmun to Neoral
You may have already been taking another medicine called Sandimmun Soft Gelatin Capsules or Sandimmun Oral Solution. Your doctor may decide to change to this medicine, Neoral Oral Solution.
• These medicines all contain ciclosporin as the active ingredient.
• Neoral is a different, improved formulation of ciclosporin compared to Sandimmun. Ciclosporin is absorbed into your blood better with Neoral and absorption is less likely to be affected by taking the medicine with food. This means that the levels of ciclosporin in your blood stay more constant with Neoral than with Sandimmun.
If your doctor changes you from Sandimmun to Neoral:
• Do not go back to taking Sandimmun unless your doctor tells you to.
• Following your transfer from Sandimmun to Neoral, your doctor will monitor you more closely for a short time. This is because of the change in how ciclosporin is absorbed into your blood. Your doctor will make sure that you get the right dose for your individual needs.
• You may have some side effects. If this happens, tell your doctor or pharmacist. Your dose may need to be lowered. Never lower your dose yourself, unless a doctor has told you to.
If your doctor switches you from one oral formulation of ciclosporin to another
After you change from one oral formulation of ciclosporin to another:
• Your doctor will monitor you more closely for a short time.
• You may have some side effects. If this happens, tell your doctor or pharmacist. Your dose may need to be changed. Never change your dose yourself, unless a doctor has told you to.
When to take Neoral
Take Neoral at the same time every day. This is very important if you have had a transplant.
How to take Neoral
Your daily doses should always be taken in 2 divided doses.
- For initial use, follow steps 1 to 9.
- For subsequent use, follow steps 5 to 9.
1. Lift the flap in the centre of the metal sealing ring.
2. Tear off the sealing ring completely.
3. Take off the black stopper and throw it away.

5
6
7.
8.
Choose the syringe depending on how much medicine you need to measure:
- For 1 ml or less of medicine, use the 1 ml syringe.
- For more than 1 ml of medicine, use the 4 ml syringe.
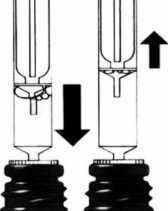
Push the nozzle of the syringe into the white stopper.

Pull up the plunger until you have drawn up the
correct amount of medicine.
- The lower part of the plunger ring needs to be in front of the mark on the syringe which shows the amount of medicine.
Push down and pull up the plunger a few times.
- This will get rid of any large air bubbles. It does not matter if there are a few tiny bubbles in the syringe. This will not affect the dose in any way.
Ensure that the correct amount of medicine is in the syringe.
Then, take the syringe out of the bottle
Push the medicine out of the syringe into a small glass containing liquid, preferably orange or apple juice.
- Make sure that the syringe does not touch the liquid in the glass.
- Stir and drink the whole contents of the glass straight away.

4.
Push the tube unit with the white stopper firmly into the neck of the bottle.


9
After use, wipe the syringe on the outside only with a dry tissue.
- Then, put the syringe back in its cover.
- Leave the white stopper and tube in the bottle.
- Close the bottle with the cap provided.

How long to take Neoral
Your doctor will tell you how long you need to take Neoral for. This depends on whether you are taking it after a transplant or for the treatment of a severe skin condition, rheumatoid arthritis, uveitis or nephrotic syndrome. For severe rash, the treatment usually lasts for 8 weeks.
Keep taking Neoral for as long as your doctor tells you.
If you have questions about how long to take Neoral, talk to your doctor or your pharmacist.
If you take more Neoral than you should
If you accidentally take too much of your medicine, tell your doctor immediately or go to your nearest hospital emergency unit. You may need medical attention.
If you forget to take Neoral
• If you forget to take a dose, take it as soon as you remember it. However, if it is almost time for your next dose, skip the missed dose. Then go on as before.
• Do not take a double dose to make up for a forgotten dose.
If you stop taking Neoral
Do not stop taking Neoral unless your doctor tells you to.
Keep taking Neoral even if you feel well. Stopping your treatment with Neoral may increase the risk of your transplanted organ being rejected.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Some side effects could be serious
Tell your doctor straight away if you notice any of the following serious side effects:
• Like other medicines that act on the immune system, ciclosporin may influence your body's ability to fight against infection and may cause tumours or other cancers, particularly of the skin. Signs of infection might be fever or sore throat.
• Changes in your sight, loss of coordination, being clumsy, memory loss, difficulty speaking or understanding what others say, and muscle weakness. These might be signs of an infection of the brain called progressive multifocal leukoencephalopathy.
• Brain problems with signs such as seizures, confusion, feeling disorientated, being less responsive, personality changes, feeling agitated, sleeplessness, changes to your sight, blindness, coma, paralysis of part or all of the body, stiff neck, loss of coordination with or without unusual speech or eye movements.
• Swelling at the back of the eye. This may be associated with blurred vision. It may also affect your sight because of the higher pressure inside your head (benign intracranial hypertension).
• Liver problems and damage with or without yellow skin and eyes, nausea, loss of appetite and dark urine.
• Kidney problems which may greatly reduce the amount of urine you produce.
• Low level of red blood cells or platelets. The signs include pale skin, feeling tired, being breathless, having dark urine (this is a sign of the breakdown of red blood cells), bruising or bleeding with no obvious reasons, feeling confused, feeling disorientated, being less alert and having kidney problems.
Other side effects include:
Very common side effects: These side effects may affect more than 1 in 10 people.
• Kidney problems.
• High blood pressure.
• Headache.
• Shaking of your body which you cannot control.
• Excessive growth of body and facial hair.
• High level of lipids in your blood.
If any of these affects you severely, tell your doctor.
Common side effects: These side effects may affect between 1 and 10 in every 100 people.
• Fits (seizures).
• Liver problems.
• High level of sugar in your blood.
• Tiredness.
• Loss of appetite.
• Nausea (feeling sick), vomiting, abdominal pain, constipation, diarrhoea.
• Excessive hair growth.
• Acne, hot flushes.
• Fever.
• Low level of white blood cells.
• Feeling numb or tingling.
• Pain in your muscles, muscle spasm.
• Stomach ulcer.
• Gum tissue overgrowing and covering your teeth.
• High level of uric acid or patassium in your blood, low levels of magnesium in your blood.
If any of these affects you severely, tell your doctor.
Uncommon side effects: These side effects may affect between 1 and 10 in every 1,000 people.
• Symptoms of brain disorders including sudden fits, mental confusion, sleeplessness, disorientation, disturbance of vision, unconsciousness, sense of weakness in the limbs, impaired movements.
• Rash.
• General swelling.
• Weight gain.
• Low level of red blood cells, low level of platelets in your blood which could increase the risk of bleeding.
If any of these affects you severely, tell your doctor.
Rare side effects: These side effects may affect between 1 and 10 in every
10.000 people.
• Nerve problems with numbness or tingling in fingers and toes.
• Inflammation of the pancreas with severe upper stomach pain.
• Muscle weakness, loss of muscle strength, pain in muscles of the legs or hands or anywhere in the body.
• Destruction of red blood cells, involving kidney problems with symptoms such as swelling of the face, stomach, hands and/or feet, decreased urination, breathing difficulty, chest pain, fits, unconsciousness.
• Changes in menstrual cycle, breast enlargement in men.
If any of these affects you severely, tell your doctor.
Very rare side effects: These side effects may affect between 1 and 10 in every
100.000 people.
• Swelling at the back of the eye which may be associated with an increase in pressure inside the head and eyesight disturbances.
If this affects you severely, tell your doctor.
Other side effects with frequency not known: Frequency cannot be estimated from the available data.
• Serious liver problems both with and without yellowing of the eyes or skin, nausea (feeling sick), loss of appetite, dark coloured urine, swelling of the face, feet, hands and/or the whole body.
• Bleeding underneath the skin or purple skin patched, sudden bleeding with no apparent cause.
• Migraine or severe headache often with feeling and being sick (nausea, vomiting) and being sensitive to light
• Pain in legs and feet
If any of these affects you severely, tell your doctor.
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
Additional side effects in children and adolescents
There are no additional side effects to be expected in children and adolescents
compared to adults.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Neoral
Keep out of the sight and reach of children.
Store at room temperature (15°C to 30°C). Do not store in the refrigerator.
Do not store below 20°C for more than 1 month.
This is because this product contains oils which can become solid at low temperatures. If the medicine is put in the refrigerator by mistake, let it reach room temperature before using it again. Flakes or small bits (sediments) in the medicine do not affect how the medicine works or how safe it is to use. The dose can be still be measured correctly with the syringe. The content of the bottle is stable for 2 months after opening. Use the solution within 2 months of opening the bottle.
Do not take Neoral after the expiry date which is printed on the outside of the pack.
If your doctor tells you to stop taking Neoral, please take any unused liquid back to your pharmacist to be destroyed. Do not throw it away with your normal household water or waste. This will help to protect the environment.
If your medicine gets discoloured or shows any other signs of deterioration, seek the advice of your pharmacist.
If any signs of damaging and tampering are present, return product to the store where it was sold to be checked.
6. Contents of the pack and other information
Each ml of oral solution contains 100 mg of ciclosporin. It also contains the following inactive ingredients: alpha-tocopherol, ethanol anhydrous, propylene glycol, corn oil, macrogolglycerol hydroxystearate / hydrogenated polyoxyl castor oil.
Neoral is available in a cardboard carton containing a 50 ml brown glass bottle with a rubber stopper and aluminium tear-off cap. A black polypropylene cap is provided for closure of bottle during the in use period. A 4 ml and 1 ml syringe is also provided in its own plastic case.
Manufactured by: Novartis s.r.o., Na Pankraci 1724/129, 140 00 Prague 4, Czech Republic.
Procured from within the EU & repackaged by Product Licence holder:
Kosei Pharma UK Ltd, 956 Buckingham Avenue, Slough Trading Estate, SL1 4NL, UK
Neoral 100mg/ml Oral Solution, pom
PL: 39352/0106
Leaflet date: 12/07/2016
If you would like any more information, or would like the leaflet in a different format, please contact Medical Information at Novartis Pharmaceuticals UK Ltd, telephone number 01276 698370.
Package leaflet: information for the patient
Ciclosporin 100 mg/ml Oral Solution
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
What is in this leaflet
1. What Ciclosporin is and what it is used for
2. What you need to know before you take Ciclosporin
3. How to take Ciclosporin
4. Possible side effects
5. How to store Ciclosporin
6. Contents of the pack and other information
1. What Ciclosporin is and what it is used for
What Ciclosporin is
The name of your medicine is Ciclosporin. It contains the active substance ciclosporin.
This belongs to a group of medicines known as immunosuppressive agents.
These medicines are used to lower the body's immune reactions.
What Ciclosporin is used for and how Ciclosporin works
* If you have had an organ transplant, bone marrow and stem cell transplantation, the function of Ciclosporin is to control your body's immune system. Ciclosporin prevents rejection of transplanted organs by blocking the development of certain cells which would normally attack the transplanted tissue.
• If you have an autoimmune disease, in which your body's immune response attacks your body's own cells, Ciclosporin stops this immune reaction. Such diseases include eye problems which threaten your vision (endogenous uveitis, including Behget's uveitis), severe cases of certain skin diseases (atopic dermatitis, or eczema and psoriasis), severe rheumatoid arthritis and a kidney disease called nephrotic syndrome.
2. What you need to know before you take Ciclosporin
If you are taking Ciclosporin following a transplant it will only be prescribed for you by a doctor with experience in transplants and/or autoimmune diseases.
The advice in this leaflet may vary depending on whether you are taking the medicine for a transplant or for an autoimmune disease.
Follow all your doctor's instructions carefully. They may differ from the general information contained in this leaflet.
Do not take Ciclosporin:
- if you are allergic to ciclosporin or any of the other ingredients of this medicine (listed in section 6).
- with products containing Hypericum perforatum (St John's Wort).
- with products containing dabigatran etexilate (used to avoid blood clots after surgery) or bosentan and aliskiren (used to reduce high blood pressure).
Do not take Ciclosporin and tell your doctor if the above applies to you. If you are not sure, talk to your doctor before taking Ciclosporin.
Warnings and precautions
Before and during treatment with Ciclosporin, tell your doctor straight away:
• if you have any signs of infection, such as fever or a sore throat. Ciclosporin suppresses the immune system and may also affect your body's ability to fight against infection.
• if you have liver problems.
• if you have kidney problems. Your doctor will carry out regular blood tests and may change your dose if necessary.
• if you develop high blood pressure. Your doctor will check your blood pressure regularly and may give you a medicine to lower blood pressure if necessary.
• if you have low levels of magnesium in your body. Your doctor may give you magnesium supplements to take, especially just after your operation if you have had a transplant.
• if you have high levels of potassium in your blood.
• if you have gout.
• if you need to have a vaccination.
If any of the above applies to you before or during treatment with Ciclosporin, tell your doctor straight away.
Sunlight and sun protection
Ciclosporin suppresses your immune system. This increases your risk of developing cancers, particularly of the skin and lymphoid system. You should limit your exposure to sunlight and UV light by:
• Wearing appropriate protective clothing.
• Often applying a sunscreen with a high protection factor.
Talk to your doctor before taking Ciclosporin:
• if you have or have had alcohol-related problems.
• if you have epilepsy.
• if you have any liver problems.
• if you are pregnant.
• if you are breast-feeding.
• if this medicine is being prescribed for a child.
If any of the above apply to you (or you are not sure), tell your doctor before taking Ciclosporin. This is because this medicine contains alcohol (see section below “Ciclosporin contains ethanol”).
Monitoring during your treatment with Ciclosporin
Your doctor will check:
• the levels of ciclosporin in your blood, especially if you have had a transplant,
• your blood pressure before the start of your treatment and regularly during treatment,
• how well your liver and kidneys are working,
• your blood lipids (fats).
If you have any questions about how Ciclosporin works or why this medicine has been prescribed for you, ask your doctor.
In addition if you are taking Ciclosporin for a non-transplant disease
(intermediary or posterior uveitis and Behget's uveitis, atopic dermatitis, severe rheumatoid arthritis or nephrotic syndrome), do not take Ciclosporin:
• if you have kidney problems (except for nephrotic syndrome).
• if you have an infection which is not under control with medication.
• if you have any type of cancer.
• if you have high blood pressure (hypertension) which is not under control with medication. If you get high blood pressure during treatment and it cannot be controlled, Ciclosporin should be stopped by your doctor.
Do not take Ciclosporin if any of the above applies to you. If you are not sure, talk to your doctor or pharmacist before taking Ciclosporin.
If you are being treated for Behget's uveitis, your doctor will monitor you particularly carefully if you have neurological symptoms (for example: increased forgetfulness, personality changes noticed over time, psychiatric or mood disorders, burning sensation in limbs, decreased sensation in limbs, tingling sensation in limbs, weakness of limbs, walking disturbances, headache with or without nausea and vomiting, vision disturbances including restricted movement of eyeball).
Your doctor will closely monitor you if you are elderly and are being treated for psoriasis or atopic dermatitis. If you have been prescribed Ciclosporin to treat your psoriasis or atopic dermatitis, you must not be exposed to any UVB-rays or phototherapy during treatment.
Children and adolescents
Ciclosporin should not be given to children for a non-transplant disease, except for treatment of nephrotic syndrome.
Elderly population (65 years of age and older)
There is limited experience with Ciclosporin in elderly patients. Your doctor should monitor how well your kidneys work. If you are over 65 and have psoriasis or atopic dermatitis, you should only be treated with Ciclosporin if your condition is particularly severe.
Other medicines and Ciclosporin
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
In particular tell your doctor or pharmacist if you are taking any of the following medicines before or during Ciclosporin treatment:
• Medicines that may affect your potassium levels. These include medicines which contain potassium, potassium supplements, water tablets (diuretics) called potassium-sparing diuretics and some medicines which lower your blood pressure.
• Methotrexate. This is used to treat tumours, severe psoriasis and severe rheumatoid arthritis.
• Medicines which may increase or decrease the level of ciclosporin (the active substance of Ciclosporin) in your blood. Your doctor might check the level of ciclosporin in your blood when starting or stopping treatment with other medicines.
- Medicines which may increase the level of ciclosporin in your blood include: antibiotics (such as erythromycin or azythromycin), anti-fungals (voriconazole, itraconazole), medicines used for heart problems or high blood pressure (diltiazem, nicardipine, verapamil, amiodarone), metoclopramide (used to stop sickness), oral contraceptives, danazol (used to treat menstrual problems), medicines used to treat gout (allopurinol), cholic acid and derivatives (used to treat gallstones), protease inhibitors used to treat HIV, imatinib (used to treat leukaemia or tumours), colchicine, telaprevir (used to treat hepatitis C).
- Medicines which may decrease the level of ciclosporin in your blood include: barbiturates (used to help you to sleep), some anti-convulsant medicines (such as carbamazepine or phenytoine), octreotide (used to treat acromegaly or neuroendocrine tumours in the gut), anti-bacterial medicines used to treat tuberculosis, orlistat (used to help weight loss), herbal medicines containing St. John's wort, ticlopidine (used after a stroke), certain medicines which lower blood pressure (bosentan), and terbinafine (an anti-fungal medicine used to treat infections of the toes and nails).
• Medicines which may affect your kidneys. These include: anti-bacterial medicines (gentamycin, tobramycin, ciprofloxacin), anti-fungal medicines which contain amphotericin B, medicines used for urinary tract infections which contain trimethoprim, medicines for cancer which contain melphalan, medicines used to lower the amount of acid in your stomach (acid secretion inhibitors of the H2-receptor antagonist type), tacrolimus, pain killers (non-steroid anti-inflammatory medicines such as diclofenac), fibric acid medicines (used to lower the amount of fat in the blood).
• Nifedipine. This is used to treat high blood pressure and heart pain. You might get swollen gums that might grow over your teeth if you are taking nifedipine during your treatment with ciclosporin.
• Digoxin (used to treat heart problems), medicines which lower cholesterol (HMG-CoA reductase inhibitors also called statins), prednisolone, etoposide (used to treat cancer), repaglinide (oral anti-diabetic medicine), immunosuppressives (everolimus, sirolimus), ambrisentan and specific anti-cancer medicines called anthracyclines (such as doxorubicin).
If any of the above applies to you (or you are not sure), talk to your doctor or pharmacist before taking Ciclosporin.
Ciclosporin with food and drink
Do not take Ciclosporin with grapefruit or grapefruit juice. This is because these can affect how Ciclosporin works.
Pregnancy and breast-feeding
Ask your doctor or pharmacist for advice before taking this medicine. Your doctor will discuss with you the potential risks of taking Ciclosporin during pregnancy.
• Tell your doctor if you are pregnant or intend to become pregnant.
Experience with Ciclosporin in pregnancy is limited. In general, Ciclosporin should not be taken during pregnancy. If it is necessary for you to take this medicine, your doctor will discuss with you the benefits and potential risks of taking it during pregnancy.
• Tell your doctor if you are breast-feeding. Breast-feeding is not recommended during treatment with Ciclosporin. This is because ciclosporin, the active substance, passes into breast milk. This may affect your baby.
Driving and using machines
Ciclosporin contains alcohol. This may affect your ability to drive and use machines.
Ciclosporin contains ethanol
Ciclosporin contains approximately 12.0 vol. % ethanol (alcohol), which corresponds to up to 500 mg per dose used in transplant patients. This is equivalent to nearly 15 ml beer or 5 ml wine per dose.
Alcohol may be harmful if you have alcohol-related problems, epilepsy, brain injury, liver problems or if you are pregnant or breast-feeding. It may also be harmful if this medicine is given to children.
Ciclosporin contains castor oil
Ciclosporin contains castor oil, which may cause stomach discomfort and diarrhoea.
3. How to take Ciclosporin
Always take this medicine exactly as your doctor has told you. Check with your doctor if you are not sure.
Do not take more than the recommended dose.
The dose of this medicine will be carefully adjusted to your individual needs by your doctor. Too much of the medicine can affect your kidneys. You will have regular blood tests and visits to the hospital, especially after a transplant. This will give you the chance to talk to your doctor about your treatment and talk about any problems you may be having.
How much Ciclosporin to take
Your doctor will work out the correct dose of Ciclosporin for you. This depends on your body weight and what you are taking the medicine for. Your doctor will also tell you how often to take your medicine.
• In adults:
Organ, bone marrow and stem cell transplantation
- The total dose each day is usually between 2 mg and 15 mg per kilogram body weight. This is divided in two doses.
- Usually, higher doses are used before and just after your transplant. Lower doses are used once your transplanted organ or bone marrow has stabilised.
- Your doctor will adjust your dose to one that is ideal for you. To do this, your doctor may need to do some blood tests.
Endogenous uveitis
- The total dose each day is usually between 5 mg and 7 mg per kilogram body weight. This is divided in two doses.
Nephrotic syndrome
- The total dose each day for adults is usually 5 mg per kilogram body weight. This is divided in two doses. In patients with kidney problems, the first dose taken each day should not be more than 2.5 mg per kilogram body weight.
Severe rheumatoid arthritis
- The total dose each day is usually between 3 mg per kilogram of your body weight and 5 mg per kilogram body weight. This is divided in two doses.
Psoriasis and atopic dermatitis
- The total dose each day is usually between 2.5 mg per kilogram of your body weight and 5 mg per kilogram body weight. This is divided in two doses.
• In children:
Nephrotic syndrome
- The total dose each day for children is usually 6 mg per kilogram body weight. This is divided in two doses. In patients with kidney problems, the first dose taken each day should not be more than 2.5 mg per kilogram body weight. Follow your doctor's instructions exactly and never change the dose yourself, even if you feel well.
Switch from Sandimmun to Ciclosporin
You may have already been taking another medicine called Sandimmun Soft Gelatin Capsules or Sandimmun Oral Solution. Your doctor may decide to change to this medicine, Ciclosporin Oral Solution.
• These medicines all contain ciclosporin as the active ingredient.
• Ciclosporin is a different, improved formulation of ciclosporin compared to Sandimmun. Ciclosporin is absorbed into your blood better with Ciclosporin and absorption is less likely to be affected by taking the medicine with food. This means that the levels of ciclosporin in your blood stay more constant with Ciclosporin than with Sandimmun.
If your doctor changes you from Sandimmun to Ciclosporin:
• Do not go back to taking Sandimmun unless your doctor tells you to.
• Following your transfer from Sandimmun to Ciclosporin, your doctor will monitor you more closely for a short time. This is because of the change in how ciclosporin is absorbed into your blood. Your doctor will make sure that you get the right dose for your individual needs.
• You may have some side effects. If this happens, tell your doctor or pharmacist. Your dose may need to be lowered. Never lower your dose yourself, unless a doctor has told you to.
If your doctor switches you from one oral formulation of ciclosporin to another
After you change from one oral formulation of ciclosporin to another:
• Your doctor will monitor you more closely for a short time.
• You may have some side effects. If this happens, tell your doctor or pharmacist. Your dose may need to be changed. Never change your dose yourself, unless a doctor has told you to.
When to take Ciclosporin
Take Ciclosporin at the same time every day. This is very important if you have had a transplant.
How to take Ciclosporin
Your daily doses should always be taken in 2 divided doses.
- For initial use, follow steps 1 to 9.
- For subsequent use, follow steps 5 to 9.
Starting a new bottle of Ciclosporin Oral Solution
Measuring your dose
1. Lift the flap in the centre of the metal sealing ring.
2.
Tear off the sealing ring completely.

5
6
Choose the syringe depending on how much medicine you need to measure:
- For 1 ml or less of medicine, use the 1 ml syringe.
- For more than 1 ml of medicine, use the 4 ml syringe.
Push the nozzle of the syringe into the white stopper.


7.
Pull up the plunger until you have drawn up the
correct amount of medicine.
- The lower part of the plunger ring needs to be in front of the mark on the syringe which shows the amount of medicine.

7. Take off the black stopper and throw it away.

8.
Push down and pull up the plunger a few times.
- This will get rid of any large air bubbles. It does not matter if there are a few tiny bubbles in the syringe. This will not affect the dose in any way.
Ensure that the correct amount of medicine is in the syringe.
Then, take the syringe out of the bottle

Push the medicine out of the syringe into a small glass containing liquid, preferably orange or apple juice.
- Make sure that the syringe does not touch the liquid in the glass.
- Stir and drink the whole contents of the glass straight away.
8.
Push the tube unit with the white stopper firmly into the neck of the bottle.



9
After use, wipe the syringe on the outside only with a dry tissue.
- Then, put the syringe back in its cover.
- Leave the white stopper and tube in the bottle.
- Close the bottle with the cap provided.

How long to take Ciclosporin
Your doctor will tell you how long you need to take Ciclosporin for. This depends on whether you are taking it after a transplant or for the treatment of a severe skin condition, rheumatoid arthritis, uveitis or nephrotic syndrome. For severe rash, the treatment usually lasts for 8 weeks.
Keep taking Ciclosporin for as long as your doctor tells you.
If you have questions about how long to take Ciclosporin, talk to your doctor or your pharmacist.
If you take more Ciclosporin than you should
If you accidentally take too much of your medicine, tell your doctor immediately or go to your nearest hospital emergency unit. You may need medical attention.
If you forget to take Ciclosporin
• If you forget to take a dose, take it as soon as you remember it. However, if it is almost time for your next dose, skip the missed dose. Then go on as before.
• Do not take a double dose to make up for a forgotten dose.
If you stop taking Ciclosporin
Do not stop taking Ciclosporin unless your doctor tells you to.
Keep taking Ciclosporin even if you feel well. Stopping your treatment with Ciclosporin may increase the risk of your transplanted organ being rejected.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Some side effects could be serious
Tell your doctor straight away if you notice any of the following serious side effects:
• Like other medicines that act on the immune system, ciclosporin may influence your body's ability to fight against infection and may cause tumours or other cancers, particularly of the skin. Signs of infection might be fever or sore throat.
• Changes in your sight, loss of coordination, being clumsy, memory loss, difficulty speaking or understanding what others say, and muscle weakness. These might be signs of an infection of the brain called progressive multifocal leukoencephalopathy.
• Brain problems with signs such as seizures, confusion, feeling disorientated, being less responsive, personality changes, feeling agitated, sleeplessness, changes to your sight, blindness, coma, paralysis of part or all of the body, stiff neck, loss of coordination with or without unusual speech or eye movements.
• Swelling at the back of the eye. This may be associated with blurred vision. It may also affect your sight because of the higher pressure inside your head (benign intracranial hypertension).
• Liver problems and damage with or without yellow skin and eyes, nausea, loss of appetite and dark urine.
• Kidney problems which may greatly reduce the amount of urine you produce.
• Low level of red blood cells or platelets. The signs include pale skin, feeling tired, being breathless, having dark urine (this is a sign of the breakdown of red blood cells), bruising or bleeding with no obvious reasons, feeling confused, feeling disorientated, being less alert and having kidney problems.
Other side effects include:
Very common side effects: These side effects may affect more than 1 in 10 people.
• Kidney problems.
• High blood pressure.
• Headache.
• Shaking of your body which you cannot control.
• Excessive growth of body and facial hair.
• High level of lipids in your blood.
If any of these affects you severely, tell your doctor.
Common side effects: These side effects may affect between 1 and 10 in every 100 people.
• Fits (seizures).
• Liver problems.
• High level of sugar in your blood.
• Tiredness.
• Loss of appetite.
• Nausea (feeling sick), vomiting, abdominal pain, constipation, diarrhoea.
• Excessive hair growth.
• Acne, hot flushes.
• Fever.
• Low level of white blood cells.
• Feeling numb or tingling.
• Pain in your muscles, muscle spasm.
• Stomach ulcer.
• Gum tissue overgrowing and covering your teeth.
• High level of uric acid or patassium in your blood, low levels of magnesium in your blood.
If any of these affects you severely, tell your doctor.
Uncommon side effects: These side effects may affect between 1 and 10 in every 1,000 people.
• Symptoms of brain disorders including sudden fits, mental confusion, sleeplessness, disorientation, disturbance of vision, unconsciousness, sense of weakness in the limbs, impaired movements.
• Rash.
• General swelling.
• Weight gain.
• Low level of red blood cells, low level of platelets in your blood which could increase the risk of bleeding.
If any of these affects you severely, tell your doctor.
Rare side effects: These side effects may affect between 1 and 10 in every
10.000 people.
• Nerve problems with numbness or tingling in fingers and toes.
• Inflammation of the pancreas with severe upper stomach pain.
• Muscle weakness, loss of muscle strength, pain in muscles of the legs or hands or anywhere in the body.
• Destruction of red blood cells, involving kidney problems with symptoms such as swelling of the face, stomach, hands and/or feet, decreased urination, breathing difficulty, chest pain, fits, unconsciousness.
• Changes in menstrual cycle, breast enlargement in men.
If any of these affects you severely, tell your doctor.
Very rare side effects: These side effects may affect between 1 and 10 in every
100.000 people.
• Swelling at the back of the eye which may be associated with an increase in pressure inside the head and eyesight disturbances.
If this affects you severely, tell your doctor.
Other side effects with frequency not known: Frequency cannot be estimated from the available data.
• Serious liver problems both with and without yellowing of the eyes or skin, nausea (feeling sick), loss of appetite, dark coloured urine, swelling of the face, feet, hands and/or the whole body.
• Bleeding underneath the skin or purple skin patched, sudden bleeding with no apparent cause.
• Migraine or severe headache often with feeling and being sick (nausea, vomiting) and being sensitive to light.
• Pain in legs and feet
If any of these affects you severely, tell your doctor.
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
Additional side effects in children and adolescents
There are no additional side effects to be expected in children and adolescents compared to adults.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard.
By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Ciclosporin
Keep out of the sight and reach of children.
Store at room temperature (15°C to 30°C). Do not store in the refrigerator.
Do not store below 20°C for more than 1 month.
This is because this product contains oils which can become solid at low temperatures. If the medicine is put in the refrigerator by mistake, let it reach room temperature before using it again. Flakes or small bits (sediments) in the medicine do not affect how the medicine works or how safe it is to use. The dose can be still be measured correctly with the syringe. The content of the bottle is stable for 2 months after opening. Use the solution within 2 months of opening the bottle.
Do not take Ciclosporin after the expiry date which is printed on the outside of the pack.
If your doctor tells you to stop taking Ciclosporin, please take any unused liquid back to your pharmacist to be destroyed. Do not throw it away with your normal household water or waste. This will help to protect the environment.
If your medicine gets discoloured or shows any other signs of deterioration, seek the advice of your pharmacist.
If any signs of damaging and tampering are present, return product to the store where it was sold to be checked.
6. Contents of the pack and other information
Each ml of oral solution contains 100 mg of ciclosporin. It also contains the following inactive ingredients: alpha-tocopherol, ethanol anhydrous, propylene glycol, corn oil, macrogolglycerol hydroxystearate / hydrogenated polyoxyl castor oil.
Ciclosporin is available in a cardboard carton containing a 50 ml brown glass bottle with a rubber stopper and aluminium tear-off cap. A black polypropylene cap is provided for closure of bottle during the in use period. A 4 ml and 1 ml syringe is also provided in its own plastic case.
Manufactured by: Novartis s.r.o., Na Pankraci 1724/129, 140 00 Prague 4,
Czech Republic.
Procured from within the EU & repackaged by Product Licence holder:
Kosei Pharma UK Ltd, 956 Buckingham Avenue, Slough Trading Estate, SL1 4NL, UK
Ciclosporin 100mg/ml Oral Solution,
PL: 39352/0106 -
Leaflet date: 12/07/2016
If you would like any more information, or would like the leaflet in a different format, please contact Medical Information at Novartis Pharmaceuticals UK Ltd, telephone number 01276 698370.