Ofloxacin 400Mg Tablets
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Ofloxacin 400 mg Tablets
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
Each film-coated tablet contains 400 mg of ofloxacin.
Excipients with known effect
Each tablet contains 211.2 mg lactose monohydrate
For the full list of excipients, see section 6.1.
3. PHARMACEUTICAL FORM
Film coated tablets
White, oval shaped film-coated tablets 18 mm length x 8 mm width, debossed “FXN 400” on one side and scoreline on the other.
4 CLINICAL PARTICULARS
4.1. Therapeutic Indications
Ofloxacin is indicated for the treatment of the following infections when
caused by sensitive organisms (see section 5.1.):
- upper and lower urinary tract infections;
- lower respiratory tract infections including pneumonia, bronchitis, and acute exacerbations of chronic bronchitis caused by gram-negative aerobic bacteria (Ofloxacin is not the first choice of medicinal product in pneumonia caused by Streptococcus pneumoniae, Mycoplasma pneumoniae or Chlamydia pneumoniae);
- uncomplicated urethral and cervical gonorrhoea;
- non-gonococcal urethritis and cervicitis;
- skin and soft tissue infections.
Consideration should be given to official guidance on the appropriate use of
anti-bacterial agents.
4.2 Posology and method of administration
Posology
General dosage recommendations:
The dose of ofloxacin should be determined by the type and severity of the infection.
The dosage range for adults is 200 mg to 800 mg daily.
Up to 400 mg may be given as a single dose, preferably in the morning. Generally, individual doses should be given at approximately equal intervals.
In individual cases it may be necessary to increase the dose to a maximum total dose of 800 mg daily, which should be given as 400 mg twice daily. This may be appropriate in infections due to pathogens known to have reduced or variable susceptibility to ofloxacin, in severe and/or complicated infections (e.g. of the respiratory or urinary tracts) or if the patient does not respond adequately.
|
Indications |
Single and daily doses |
Usual duration of therapy |
|
Uncomplicated lower urinary tract infections |
200 - 400 mg daily |
3 days |
|
Complicated infections of the kidneys and urinary tract |
400 mg daily, increasing if necessary, to 400 mg twice a day |
7-10 days |
|
Lower respiratory tract infections |
400mg daily, increasing, if necessary, to 400 mg twice a day |
7-10 days |
|
Uncomplicated gonorrhoea |
400 mg |
Single dose |
|
Non-gonococcal urethritis and cervicitis |
400 mg daily |
7-10 days |
|
Skin and soft tissue infections |
400 mg twice a day |
7-10 days |
Renal impairment:
In patients with impaired renal function, the following oral or I.V dosages are recommended:
|
Creatinine clearance |
Unit dose mg1 |
Number /24 hours |
Intervals hours |
|
50 - 20 ml/min |
100 - 200 |
1 |
24 |
|
< 20 ml/min2 |
100 |
1 |
24 |
|
Or haemodialysis |
or | ||
|
or peritoneal dialysis |
200 |
1 |
48 |
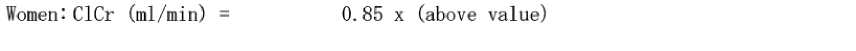
When creatinine clearance cannot be measured, it can be estimated with reference to the serum creatinine level using the following Cockcroft's formula for adults:
weight(kg) x (140 - age in years)
Men: CICr (ml/min) =
72 x serum creatinine (mg/dl)
or
weight (kg) x (140 - age in years)
CICr (ml/min)
0. 814 x serum creatinine (|omol/l)
Hepatic impairment (e.g. cirrhosis with ascites)
It is recommended that a maximum daily dose of 400 mg of ofloxacin be not exceeded, because of possible reduction of excretion.
Elderly:
Age in itself does not impose to adapt the dosage of ofloxacin. However, special attention to renal and liver function should be paid in elderly patients, and the dosage should be adapted accordingly(see section 4.4).
Paediatric population:
Ofloxacin is not indicated for use in children or growing adolescents.
Type and duration of treatment:
A daily dose of up to 400mg ofloxacin may be given as a single dose. In this case, it is preferable to administer ofloxacin in the morning.
Daily doses of more than 400mg must be divided into two separate doses and be given at approximately equal intervals.
Duration of treatment is dependent on the severity of the infection and the response to treatment.
The usual durations of treatment are stated in the table.
In some instances, a minimum of 5 days treatment may be sufficient.
Treatment should not exceed 2 months duration.
Method of administration
Ofloxacin Tablets should be swallowed with sufficent amount of liquids They may be taken on an empty stomach or with meals. Concomitant administration with antacids should be avoided (see section 4.5).
4.3 Contraindications
Ofloxacin must not be used
• in patients hypersensitive to ofloxacin, other quinolones, or any of the excipients
• in patients with history of epilepsy or with any existing central nervous system disorder that is associated with a lower seizure threshold
• in patients with history of tendon disorders related to fluoroquinolone administration
• in children or adolescents in the growth phase3
• during pregnancy3
• in breast-feeding women3
*because, judging from animal experiments, a risk of damage to the growth-plate cartilage in the growing organism cannot be entirely excluded.
Ofloxacin should not be given to patients with latent or actual defects in glucose-6-phosphate dehydrogenase activity because they are prone to haemolytic reactions when treated with quinolone antibacterial agents.
4.4 Special warnings and precautions for use
• Methicillin-resistant S. aureus are very likely to possess co-resistance to fluoroquinolones, including ofloxacin. Therefore ofloxacin is not recommended for the treatment of known or suspected MRSA infections unless laboratory results have confirmed susceptibility of the organism to ofloxacin (and commonly recommended antibacterial agents for the treatment of MRSA-infections are considered inappropriate).
• Severe bullous reactions Cases of severe bullous skin reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis have been reported with ofloxacin (see section 4.8). Patients should be advised to contact their doctor immediately prior to continuing treatment if skin and/or mucosal reactions occur.
• Hypersensitivity and allergic reactions have been reported for fluoroquinolones after first administration. Anaphylactic and anaphylactoid reactions can progress to life-threatening shock, even after the first administration. In these cases ofloxacin should be discontinued and suitable treatment (e.g treatment for shock) should be initiated. The physician should inform the patient of this risk.
• Ofloxacin is not the drug of first choice for pneumonia caused by Pneumococci or Mycoplama, or angina tonsillaris caused by P-haemolytic Streptococci.
• Clostridium difficile-associated disease
Diarrhoea, particularly if severe, persistent and/or bloody, during or upto 10 weeks after treatment with Ofloxacin Tablets, may be a symptom of Clostridium difficile enterocolitis, the most severe form being pseudomembraneous colitis (CDAD). CDAD may range in severity from mild to life threatening, the most severe form of which is pseudomembranous colitis (see section 4.8). It is therefore important to consider this diagnosis in patients who develop serious diarrhoea during or after treatment with ofloxacin. If pseudo-membranous colitis is suspected, ofloxacin must be stopped immediately.
Appropriate specific antibiotic therapy must be started without delay (e.g. oral vancomycin, oral teicoplanin or metronidazole). Medicinal products that inhibit peristalsis are contra-indicated in such cases.
• Patients predisposed to seizures
Quinolones may lower the seizure threshold and may trigger seizures. Ofloxacin is contraindicated in patients with a history of epilepsy (see section 4.3) and, as with other quinolones, ofloxacin should be used with extreme caution in patients predisposed to seizures.
Such patients may be patients with pre-existing central nervous system lesions, concomitant treatment with fenbufen and similar non-steroidal antiinflammatory drugs or with drugs which lower the cerebral seizure threshold, such as theophylline (see section 4.5).
In case of convulsive seizures, treatment with ofloxacin should be discontinued. 4 sometimes bilateral, may occur within 48 hours of starting treatment with ofloxacin and have been reported up to several months after discontinuation of. The risk of tendonitis and tendon rupture is increased in patients aged over 60 years and in patients using corticosteroids. The daily dose should be adjusted in elderly patients based on creatinine clearance (see section 4.2). Close monitoring of these patients is therefore necessary if they are prescribed ofloxacin. All patients should consult their physician if they experience symptoms of tendonitis. Elderly patients are more prone to tendonitis. The risk of tendon rupture may be increased by co-administration of corticosteroids. If tendonitis is suspected, treatment with ofloxacin must be halted immediately and appropriate treatment (e.g. immobilisation) must be initiated for the affected tendon (see sections 4.3 and 4.8).
• Patients with renal impairment
Since ofloxacin is mainly excreted by the kidneys, the dose of ofloxacin should be adjusted in patients with renal impairment (see section 4.2).
• Patients with history of psychotic disorder
Psychotic reactions have been reported in patients receiving fluoroquinolones, including ofloxacin. In some cases these have progressed to suicidal thoughts or self-endangering behavior including suicide attempt, sometimes after a single dose of ofloxacin (see section 4.8). In the event that a patient develops these reactions, ofloxacin should be discontinued and appropriate measures instituted.
Ofloxacin should be used with caution in patients with a history of psychotic disorder or in patients with psychiatric disease.
Patients with hepatic impairment
Ofloxacin should be used with caution in patients with impaired liver function, as liver damage may occur. Cases of fulminant hepatitis potentially leading to liver failure (including fatal cases) have been reported with fluoroquinolones. Patients should be advised to stop treatment and contact their doctor if signs and symptoms of hepatic disease develop such as anorexia, jaundice, dark urine, pruritis or tender abdomen (see section 4.8).
• Patients treated with vitamin K antagonists
Due to possible increase in coagulation tests (PT/INR) and/or bleeding in patients treated with fluoroquinolones, including ofloxacin, in combination with a vitamin K antagonist (e.g.warfarin), coagulation tests should be monitored when these drugs are given concomitantly (see section 4.5). 5
Deterioration of myasthenia gravis may occur during ofloxacin use.
• Prevention of photosensitisation
Photosensitisation has been reported with ofloxacin (see section 4.8). It is recommended that patients should avoid strong sunlight or artificial UV radiation (e.g sunray lamp, solarium), during treatment and for 48 hours following treatment discontinuation in order to prevent photosensitisation
• Superinfection
As with other antibiotics, the use of ofloxacin, especially if prolonged, may result in overgrowth of non-susceptible organisms, especially enterococci, resistant strains of some organisms or candida. Repeated evaluation of the patient’s condition is essential. If secondary infection occurs during therapy, appropriate and alternative treatment should be given.
• Cardiac disorders
QT interval prolongation
Very rare cases of QT interval prolongation have been reported in patients taking fluoroquinolones. Caution should be taken when using fluoroquinolones, including ofloxacin, in patients with known risk factors for prolongation of the QT interval such as, for example:
• Elderly patients and women may be more sensitive to QTc-prolonging medications. Therefore, caution should be taken when using fluoroquinolones, including ofloxacin, in these populations.
• uncorrected electrolyte imbalance (e.g. hypokalaemia, hypomagnesaemia)
• congenital long QT syndrome
• acquired QT prolongation
• cardiac disease (e.g. heart failure, myocardial infarction, bradycardia)
• concomitant use of drugs that are known to prolong the QT interval (e.g. Class IA and III antiarrhythmics, tricyclic antidepressants, macrolides, antipsychotics).
(See also section 4.2, section 4.5, section 4.8 and section 4.9).
• Dysglycaemia
As with all quinolones,disturbances in blood glucose, including both hypoglycaemia and hyperglycaemia have been reported, usually in diabetic patients receiving concomitant treatment with an oral hypoglycaemic agent (e.g., glibenclamide) or with insulin. Cases of hypoglycaemic coma have been reported. In diabetic patients, careful monitoring of blood glucose is recommended (see section 4.8)
Peripheral neuropathy
Sensory or sensorimotor peripheral neuropathy has been reported in patients receiving fluoroquinolones, including ofloxacin, which can be rapid in its onset. Ofloxacin should be discontinued if the patient experiences symptoms of neuropathy in order to prevent the development of an irreversible condition (see section 4.8).
• Patients with glucose-6-phosphate-dehydrogenase deficiency
Patients with a latent or diagnosed glucose-6-phosphate-dehydrogenase deficiency may be predisposed to haemolytic reactions if they are treated with quinolones.
Therefore, if ofloxacin has to be used in these patients, potential occurrence of haemolysis should be monitored.
Ofloxacin should therefore be administered with caution in such patients.
• Vision disorders:
If vision becomes impaired or any effects on the eyes are experienced, an eye specialist should be consulted immediately (see sections 4.7 and 4.8).
• Interference with laboratory tests:
Determination of opiates or porphyrins in urine may give false-positive results during treatment with ofloxacin. It may be necessary to confirm positive opiate or porphyrin screens by more specific methods.
• Patients with rare hereditary disorders
Patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption should not take this medicine.
During prolonged therapy (more than two weeks and up to two months), regular monitoring of haematological parameters and blood chemistry is recommended.
4.5 Interaction with other medicinal products and other forms of interaction
Antacids, Sucralfate, Metal Cations:
Antacids containing aluminium (including sucralfate) and magnesium hydroxides, aluminium phosphate, zinc, iron, are liable to reduce the absorption of ofloxacin tablets. Ofloxacin should be administered approximately 2 hours apart from antacids.
Theophylline, fenbufen or similar non-steroidal anti-inflammatory drugs:
No pharmacokinetic interactions of ofloxacin were found with theophylline in a clinical study. However, a pronounced lowering of the cerebral seizure
threshold may occur when quinolones are given concurrently with theophylline, nonsteroidal anti-inflammatory drugs, or other agents, which lower the seizure threshold. However, ofloxacin does not cause any relevant changes in theophylline plasma concentrations.
Drugs known to prolong QT interval:
Ofloxacin, like other fluoroquinolones, should be used with caution in patients receiving drugs known to prolong the QT interval (e.g. Class IA and III antiarrhythmics, tricyclic antidepressants, macrolides, antipsychotics) (see section 4.4)..
Vitamin K antagonists:
Increased coagulation tests (PT/INR) and/or bleeding, which may be severe, have been reported in patients treated with ofloxacin in combination with a vitamin K antagonist (e.g. warfarin). Coagulation tests should be monitored in patients treated with vitamin K antagonists (see section 4.4) because of a possible increase in the effect of coumarin derivatives.
Glibenclamide:
Ofloxacin may cause a slight increase in serum concentrations of glibenclamide administered concurrently; it is therefore recommended that patients treated with this combination should be closely monitored as hypoglycaemia is more likely to occur.
Probenecid, cimetidine, furosemide, or methotrexate:
Probenecid decreased the total clearance of ofloxacin by 24%, and increased AUC by 16%. The proposed mechanism is a competition or inhibition for active transport at the renal tubular excretion. Caution should be exercised when ofloxacin is coadministered with drugs that affect the tubular renal secretion such as probenecid, cimetidine, furosemide and methotrexate.
4.6 Fertility, pregnancy and lactation Pregnancy
Based on a limited amount of human data, the use of fluoroquinolones in the first trimester of pregnancy has not been associated with an increased risk of major malformations or other adverse effects on pregnancy outcome. Animal studies have shown damage to the joint cartilage in immature animals but no teratogenic effects. Therefore ofloxacin should not be used during pregnancy (see section 4.3: Contraindications).
The safety of this medicinal product for use in human pregnancy has not been established. Reproduction studies performed in rats and rabbits did not reveal any evidence of teratogenicity, impairment of fertility or impairment of peri-and post-natal development. However, as with other quinolones, ofloxacin has been shown to cause arthropathy in immature animals.
Breast-feeding
Studies in rats have indicated that ofloxacin is secreted in milk.
Ofloxacin is excreted into human breast milk in small amounts. Because of the potential for arthropathy and other serious toxicity in the nursing infant, breast-feeding should be discontinued during treatment with ofloxacin (see section 4.3:).
4.7 Effects on ability to drive and use machines
Some adverse reactions (e.g. dizziness/vertigo, drowsiness, visual disturbances) may impair the patients ability to concentrate and react, and therefore may constitute a risk in situations where these abilities are of special importance (e.g. driving a car or operating machinery), patients should know how they react to ofloxacin before they drive or operate machinery. These effects may be enhanced by alcohol.
4.8 Undesirable effects
The overall frequency of adverse reactions from the clinical trial data base is about 7%. The commonest events involved the gastrointestinal system (about 5.0%) and the nervous system (about 2.0%).
The frequencies of adverse events are ranked according to the following: very common (> 1/10), common (> 1/100 to < 1/10), uncommon (> 1/1000 to < 1/100), rare (> 1/10 000 to < 1/1000), very rare (< 1/10, 000), not known (cannot be estimated from the available data) including isolated reports.
The information given below is based on data from clinical studies and on extensive post marketing experience.
|
System organ class |
common (> 1/100, to < 1/10) |
Uncommon (> 1/1000 to < 1/100) |
rare(> 1/10 000 to < 1/1000) |
very rare (<1/10, 000) |
Not known (cannot be estimated from the available data) |
|
Infections and infestations |
fungal infection, pathogen resistance | ||||
|
Blood and lymphatic system disorders |
anaemia, haemolytic anaemia, leucopenia, eosinophilia, thrombocytop e-nia, |
agranulocytosis, bone marrow failure, bone marrow failure may lead to pancytopenia |
|
Immune system disorders |
anaphylactic reaction*, anaphylactoid reaction*, angioedema* |
anaphylactic shock*, anaphylactoid shock* | |||
|
Metabolism and nutrition disorders |
anorexia |
Hypoglycaemia in diabetics treated with Hypoglycaemic agents (see section 4.4) Hyperglycaemia Hypoglycaemic coma | |||
|
Psychiatric disorders |
restlessness, sleep disorder, agitation, insomnia |
psychotic disorder (for eg. hallucination), anxiety, confusional state, nightmares, depression |
abnormal dreams, psychotic behaviour |
psychotic disorders and depression with self-endangering behaviour including suicidal ideation or suicide attempt (see section 4.4) Nervousness | |
|
Nervous system disorders |
headache, dizziness |
somnolence, paraesthesia, dysgeusia, parosmia |
peripheral sensory neuropathy*, peripheral sensory motor neuropathy*, convulsion*, extrapyramidal symptoms or other disorders of muscular coordination. |
Tremor, Dyskinesia, Ageusia, Syncope | |
|
Eye disorders |
eye irritation |
visual disturbances (e.g. double vision, blurred vision) |
allergic conjunctivitis |
Uveitis | |
|
Ear and labyrinth disorders |
vertigo |
tinnitus, hearing loss |
Hearing impaired | ||
|
Cardiac disorders |
Tachycardia |
ventricular arrhythmias, torsades de pointes (reported predominantly in |
|
patients with risk factors for QT prolongation), ECG QT prolonged (see section 4.4 and 4.9) | |||||
|
Vascular disorders |
Hypotension |
circulatory collapse, flushing, vasculitis | |||
|
Respiratory, thoracic and mediastinal disorders |
cough, nasopharyngiti s |
dyspnoea, bronchospasm |
allergic pneumonitis, severe dyspnoea | ||
|
Gastro intestinal disorders |
nausea, vomiting, diarrhoea, abdominal pain |
enterocolitis, sometimes haemorrhagic |
Pseudomemb ra-nous colitis* |
Dyspepsia, Flatulence, Constipation, Pancreatitis | |
|
Hepatobiliary disorders |
hepatic enzymed increased (ALAT, ASAT, LDH, gamma-GT and/or alkaline phosphatase), blood bilirubin increased |
Jaundice cholestatic |
Hepatitis, which may be severe* Severe liver injury, including cases with acute liver failure, sometimes fatal, have been reported with ofloxacin, primarily in patients with underlying liver disorders (see section 4.4). | ||
|
Skin and subcutaneous tissue disorders |
rash, pruritus |
urticaria, hot flushes, hyperhidrosis, pustular rash |
toxic epidermal necrolysis, photosensitivit y reaction*, drug eruption, vascular purpura, vasculitis, which can lead in exceptional cases to skin necrosis, vesiculobullou s rash, angioedema, erythema |
Stevens-Johnson syndrome, acute generalised exanthemous pustulosis, drug rash Stomatitis; Exfoliative dermatitis |
|
multiforme | |||||
|
Musculoskele tal and connective tissue disorders |
tendonitis |
arthralgia, myalgia, Tendon rupture (e.g. Achilles tendon) which may occur within 48 hours of treatment start and may be bilateral, |
muscle weakness, rhabdomyolysis and/or myopathy, muscle tear, muscle rupture, Ligament rupture, Arthritis | ||
|
Renal and urinary disorders |
serum creatinine increased |
renal function disorder, acute renal failure |
acute interstitial nephritis | ||
|
Congenital and familial/ genetic disorders |
attacks of prophyria in patients with prophyria | ||||
|
General disorders and administratio n site conditions |
unsteady gait |
Asthenia Pyrexia Pain (including pain in back, chest, and extremities) |
* postmarketing experience
Except in very rare instances (e.g. isolated cases of smell, taste and hearing disorders) the adverse effects observed subsided after discontinuation of ofloxacin.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard
4.9 Overdose
Symptoms of overdose
The most important signs to be expected following acute overdose are CNS symptoms such as confusion, dizziness, impairment of consciousness and seizures, increases in QT interval as well as gastrointestinal reactions such as nausea and mucosal erosions.
CNS effects including confusional state, convulsion, hallucination, and tremor have been observed in post marketing experience
Treatment of overdose
In the event of overdose symptomatic treatment should be implemented. ECG monitoring should be undertaken, because of the the possibility of QT interval prolongation.
In the case of overdose steps to remove any unabsorbed ofloxacin eg gastric lavage, administration of adsorbants and sodium sulphate, if possible during the first 30 minutes, are recommended; antacids are recommended for protection of the gastric mucosa. A fraction of ofloxacin may be removed from the body with haemodialysis. Peritoneal dialysis and CAPD are not effective in removing ofloxacin from the body. No specific antidote exists.
Elimination of ofloxacin may be increased by forced diuresis.
5. PHARMACOLOGICAL PROPERTIES
5.1. Pharmacodynamic Properties
Mode of action
Pharmacotherapeutic group: fluoroquinolones ATC code: J01 MA 01
Ofloxacin inhibits bacterial DNA replication in a range of gram-positive and gram-negative pathogenic bacteria by inhibiting bacterial topoisomerases, particularly DNA gyrase and topoisomerase IV.
The NCCLS MIC breakpoint recommendations are as follows :
S < 2 mg/l and R > 8 mg/l Intermediate susceptibility at 4 mg/l
Haemophilus influenzae and Neisseria gonorrhoea are exceptions with breakpoints at S < 0.25 mg/l and R > 1 mg/l
The BSAC general recommendations are S < 2 mg/l and R > 4 mg/l
According to DIN 58 940, the following limits apply for ofloxacin;
S < 1 mg/L, I =2 mg/L, R > 4 mg/L.
The prevalence of resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. This information gives only an approximate guidance on probabilities whether micro-organisms will be susceptible to ofloxacin or not.
Only those pathogens relevant to the indications are listed.
|
European range of acquired bacterial resistance to ofloxacin | |
|
Normally susceptible |
|
Aerobic Gram-positive micro | |
|
organisms | |
|
S. aureus - - methicillin-sensitive |
0.3-12.6% |
|
S. pyogenes |
2-5% |
|
Aerobic Gram-negative micro organisms | |
|
Acinetobacter spp |
0.3-7.3% |
|
Citrobacter spp. |
3-15% |
|
Enterobacter spp. |
2-13% |
|
E. coli |
1-8% |
|
H. influenzae |
1% |
|
Klebsiella spp. |
1-10% |
|
Moraxella spp. |
0-0.2% |
|
Morganella morganii |
0-6.9% |
|
N. gonorrhoeae |
25% |
|
Proteus spp. |
1-15% |
|
Serratia marcescens |
2-2.4% |
|
Others | |
|
Chlamydia spp | |
|
L. pneumophila | |
|
Intermediately susceptible | |
|
Aerobic Gram-positive micro | |
|
organisms | |
|
S. pneumoniae |
70% |
|
Providentia |
17.1% |
|
Aerobic Gram-negative micro organisms | |
|
E. faecalis |
50% |
|
P. aeruginosa |
20-30% |
|
Serratia spp. |
20-40% |
|
Stenotrophomonas maltophilia |
5.1-11% |
|
Others | |
|
Mycoplasma spp. |
0-5.3% |
|
Ureaplasma spp. |
0-2.1% |
|
Resistant | |
|
Anaerobic bacteria | |
|
S. aureus - methicillin-resistant |
69.2-85.7% |
|
T. pallidum |
The main mechanism of bacterial resistance to ofloxacin involves one or more mutations in the target enzymes, which generally confer resistance to other active substances in the class. Efflux pump and impermeability mechanisms of resistance have also been described and may confer variable resistance to active substances in other classes.
5.2 Pharmacokinetic properties
Absorption:
Ofloxacin is absorbed rapidly and almost completely when administered to fasting volunteers. The mean peak plasma concentration following a single oral dose of 200 mg is 2.6 gg/ml and is achieved within an hour. The plasma concentration does not increase significantly with multiple dosing (accumulation factor with twice daily dosage: 1.5).
Distribution:
The apparent volume of distribution is 120 litres. Plasma protein binding is approximately 25%.
Biotransformation:
Ofloxacin is less than 5% biotransformed. The two principal metabolites found in the urine are N-desmethyl-ofloxacin and ofloxacin-N-oxide. Ofloxacin is found as the glucuronide in the bile.
Elimination:
Elimination is primarily by the renal route in that 80 to 90 % of the dose is excreted unchanged in the urine. The plasma elimination half-life is 5.7 to 7.0 hours, irrespective of dose.
Patients with renal impairment:
The plasma elimination half-life is prolonged in individuals with impaired renal function; total and renal clearance decrease in accordance with creatinine clearance.
5.3. Pre-clinical Safety Data
Ofloxacin exhibits a neurotoxic potential and causes reversible testicular alterations at high doses. Aside from this, preclinical studies with single and repeated use in adult animals as well as safety pharmacological investigations, yielded no indications of further specific risks in connection with the administration of ofloxacin.
Like other gyrase inhibitors, ofloxacin can also cause damage to large weightbearing joints of juvenile animals during the growth period. The extent of the cartilage damage caused is dependent on age, species, and dose. In addition, stress relief of the joints considerably reduces cartilage damage.
Ofloxacin has no influence on fertility or perinatal and postnatal development and has no teratogenic or other embryotoxic effects in animal experiments, if administered at therapeutic doses.
Ofloxacin has not been evaluated in long-term carcinogenicity studies. In-vitro and in-vivo studies showed that ofloxacin is not mutagenic. Phototoxicity, photomutagenicity, and photocarcinogenicity data of ofloxacin indicate only slight photomutagenic and phototumorigenic effects in vitro and/or in vivo, as compared to other fluoroquinolones.
There are no indications of cataractogenic or co-cataractogenic effects following exposure to ofloxacin.
Preclinical investigations performed with ofloxacin have, to date, demonstrated only a slight QT-prolonging potential.
6. PHARMACEUTICAL PARTICULARS
6.1. List of Excipients
Lactose monohydrate Pregelatinised starch Hypromellose Croscarmellose sodium Colloidal anhydrous silica Magnesium stearate Titanium dioxide E171 Macrogol 3000 Triacetin.
6.2. Incompatibilities
Not applicable
6.3. Shelf-Life
3 years
6.4. Special Precautions for Storage
Keep container in the outer carton.
6.5. Nature and Content of Container
Transparent PVC/PVdC-aluminium blisters / white opaque PVC/PVdC-aluminium blisters
Blister packs of 5, 10, 20 and 50 tablets
Not all pack sizes may be marketed.
6.6. Instruction for Use, Handling and Disposal
No special requirements
7 MARKETING AUTHORISATION HOLDER
TEVA UK Limited,
Brampton Road, Hampden Park,
Eastbourne, East Sussex,
BN22 9AG
8. MARKETING AUTHORISATION NUMBER
PL 00289/0354
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
02/04/2009
10 DATE OF REVISION OF THE TEXT
08/07/2016
According to indication or dose interval
The serum concentration of ofloxacin should be monitored in patients with severe renal impairment and dialysis patients
Resistance to fluoroquinolones of E. coli - the most common pathogen involved in urinary tract infections - varies across the European Union. Prescribers are advised to take into account the local prevalence of resistance in E. coli to fluoroquinolones.
Tendonitis
Tendonitis, rarely observed with quinolones, may occasionally lead to rupture involving Achilles tendon in particular. Tendonitis and tendon rupture,
Myasthenia gravis
Fluoroquinolones, including ofloxacin, have neuromuscular blocking activity and may exacerbate muscle weakness in patients with myasthenia gravis. Postmarketing serious adverse reactions, including deaths and the requirement for respiratory support, have been associated with fluoroquinolone use in patients with myasthenia gravis. Ofloxacin is not recommended in patients with a known history of myasthenia gravis.