Rosemar 150/30 Coated Tablets
Package leaflet: Information for the user
Rosemar 150/30 Coated Tablets
(Levonorgestrel / Ethinylestradiol)
Package leaflet: Information for the user
Rosemar 150/30 Coated Tablets
(Levonorgestrel / Ethinylestradiol)
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet:
1. What Rosemar is and what it is used for
2. What you need to know before you take Rosemar
3. How to take Rosemar
4. Possible side effects
5. How to store Rosemar
6. Contents of the pack and other information
1. What Rosemar is and what it is used for
Rosemar coated tablets are a combined oral contraceptive and belongs to a group of products often referred to as “the Pill”. Rosemar contains two hormones: estrogen (Ethinylestradiol) and progestogen (Levonorgestrel). These hormones prevent you from getting pregnant, just as your natural hormones would prevent you from conceiving again when you are already pregnant.
You must talk to a doctor if you do not feel better or if you feel worse.
2. What you need to know before you use Rosemar General notes
Before you can begin taking Rosemar, your doctor will ask you some questions about your personal health and that of your close relatives. The doctor will also measure your blood pressure and depending upon your personal situation, may also carry out some other tests.
In this leaflet, several situations are described where you should stop using Rosemar, or where the reliability of Rosemar may be decreased. In such situations you should either not have intercourse or you should take extra non-hormonal contraceptive precautions, e.g., use a condom, or another barrier method. Do not use rhythm or temperature methods. These methods can be unreliable because Rosemar alters the monthly changes of the cervical mucus.
Rosemar, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or any other sexually transmitted disease.
Do not take Rosemar
• if you are allergic to Levonorgestrel or Ethinylestradiol or any of the other ingredients of this medicine (listed in section 6).
• If you have (or have had in the past) a blood clot (thrombosis) in a blood vessel of the leg, lung (embolus) or other organs,
• If you have (or have had in the past) a heart attack or stroke
• If you have (or have had in the past) a disease that can be a predictor of a heart attack (for example, angina pectoris, which causes severe pain in the chest) or of a stroke (for example, a transient slight stroke with no residual effects).
• If you have a disease that may increase the risk of a thrombosis in the arteries. This applies to the following diseases:
o Diabetes mellitus with damaged blood vessels o Very high blood pressure
o A very high level of fat in the blood (cholesterol or triglycerides)
• If you have a disturbance of blood clotting (for example, protein C deficiency)
• If you have (had) a certain form of migraine (with so-called focal neurological symptoms).
• If you have (had) an inflammation of the pancreas (pancreatitis)
• If you have or have had in the past a liver disease and your liver function is still
not normal.
• If you have or have had a tumour in the liver.
• If you have (had) or if you are suspected to having breast cancer or cancer of the
genital organs.
• If you have any unexplained bleeding from the vagina.
• If you have absence of menstrual period and the cause is unknown
Warnings and precautions
Talk to your doctor or pharmacist or nurse before using Rosemar. In some situations you need to take special care while using Rosemar or any other combined hormonal contraceptive, and it may be necessary that you are regularly checked by your doctor. If any of the following conditions applies to you, you must inform your doctor before starting to use Rosemar. Also is any of the following conditions develops or worsens during the use of Rosemar you must consult your doctor.
• If a close relative has or has had breast cancer
• If you have a disease of the liver or the gallbladder
• If you have diabetes
• If you have depression
• If you have Crohn’s disease or ulcerative colitis (inflammatory bowel disease)
• If you have HUS (haemolytic uraemic syndrome; a blood disease that causes kidney damage)
• If you have epilepsy (see “Taking other medicines”)
• If you have SLE (systemic lupus erythematosus; a disease of the immune system)
• If you have a disease that first appeared during pregnancy or earlier use of sex hormones (for Example, hearing loss, porphyria (a disease of the blood), gestational herpes (skin rash with vesicles during pregnancy), Sydenham’s chorea (a disease of the nerves in which sudden movements of the body occur)
• If you have or have ever had chloasma (golden brown pigment patches, so called “pregnancy patches”, especially on the face). If this is the case, avoid direct exposure to sunlight or ultraviolet light.
• If you have hereditary angioedema, products containing estrogens may induce or worsen symptoms of angioedema. You should see your doctor immediately if you experience symptoms of angioedema such as swollen face, tongue and/or pharynx and/or difficulty swallowing or hives together with difficulty breathing.
• If a pre-existing high blood pressure condition worsens
• If a pre-existing high level of fat in blood worsens
Rosemar and thrombosis
Venous thrombosis
The use of any combination pill, including Rosemar, increases a woman’s risk of
developing a venous thrombosis (formation of a blood clot in vessels) compared with
a woman who does not take any (contraceptive) pill.
The risk of venous thrombosis in users of combined pills increases:
• with increasing age
• If you are overweight,
• If one of your close relatives has had a blood clot (thrombosis) in the leg, lung, or other organ at a young age,
• If you must have an operation (surgery), any prolonged period of immobilization, or if you have had a serious accident. It is important to tell your doctor in advance that you are using Rosemar as the treatment may have to be stopped. Your doctor will tell you when to start again. This is usually about two weeks after you are back on your feet.
Arterial thrombosis
The use of combination pills has been connected with an increase of the risk of arterial
thrombosis (obstruction of an artery), for example, in the blood vessels of the heart (heart attack) or the brain (stroke).
The risk of arterial thrombosis in users of combined pills increases:
• With increasing age
• If you smoke you are strongly advised to stop smoking when you use Rosemar, especially if you are older than 35 years.
• If you have an increased fat content in your blood (cholesterol or triglycerides)
• If you have high blood pressure
• If you have migraine
• If you have a problem with your heart (valve disorder, a disturbance of the heart rhythm)
Stop taking Rosemar and tell your doctor immediately if after taking Rosemar you notice possible signs of thrombosis, such as
• any unusual, severe or long-lasting headache or worsening of migraine
• partial or complete blindness or double vision
• sudden pain and/or swelling in one of your legs
• sudden breathlessness
• sudden cough without an obvious cause
• sudden severe pain in the chest which may reach the left arm
• difficulty in speaking or inability to speak
• weakness, strange feeling, or numbness in any part of the body
• a feeling of dizziness or spinning
• collapse with or without focal seizure
• motor disturbances
• sudden severe abdominal pain
Rosemar and cancer
Breast cancer has been observed slightly more often in women using combined pills, but it is not known whether this is caused by the treatment. For example it may be that more tumours are detected in women on combined pills because they are examined by their doctor more often. The occurrence of breast tumours becomes gradually less after stopping the combination hormonal contraceptives. It is important to regularly check your breasts and you should contact your doctor if you feel any lump.
In rare cases, benign liver tumours, and in even fewer cases malignant liver tumours have been reported in pill users. Contact your doctor if you have unusual severe abdominal pain.
Bleeding between periods
During the first few months that you are taking Rosemar, you may have unexpected bleeding (bleeding outside the gap week). If this bleeding lasts longer than a few months, or if it begins after some months, your doctor must investigate the cause.
What you must do if no bleeding occurs in the gap week
If you have taken all the tablets correctly, have not had vomiting or severe diarrhoea and you have not taken any other medicines, it is highly unlikely that you are pregnant.
If the expected bleeding does not happen twice in succession, you may be pregnant. Contact your doctor immediately. Do not start the next strip until you are sure that you are not pregnant.
Children and adolescents
There is no data available for use in adolescents below 18 years.
Other medicines and Rosemar
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription and herbal medicines.
Also tell any other doctor or dentist who prescribes another medicine (or the dispensing pharmacist) that you use Rosemar. They can tell you if you need to take additional contraceptive precautions (barrier method) and, if so, for how long.
• Some medicines that can have an influence on the blood level of Rosemar 150/30 Coated tablets and can make it less effective in preventing pregnancy, or can cause unexpected bleeding. These include medicines used for the treatment of:
- epilepsy (e.g. primidone, phenytoin, phenobarbital, carbamazepine, oxcarbazepine, topiramate, felbamate);
- tuberculosis (e.g. rifampicin);
- HIVand Hepatitis C Virus infections (so-called protease inhibitors and non-nucleoside reverse transcriptase inhibitors such as ritonavir, nevirapine, efavirenz)
- other infections (griseofulvin)- high blood pressure in the blood vessels in the lungs (bosentan).
• The herbal product St. John’s wort may also stop Rosemar 150/30 Coated Tablets from working properly. If you want to use herbal products containing St. John’s wort while you are already using Rosemar you should consult your doctor first.
• Some medicines can increase the levels of the active substances of Rosemar in the blood. The effectiveness of the pill is maintained, but tell your doctor if you are using anti-fungal medicines containing ketoconazole.
• Rosemar may also interfere with the working of other medicines - such as the anti-epileptic lamotrigine.
Effect on laboratory tests
If you need a blood test, tell your doctor or the laboratory staff that you are taking the pill, because oral contraceptives can affect the results of some tests.
Pregnancy, breast feeding and fertility
Preenancv
If you become pregnant while taking Rosemar you must stop immediately and contact your doctor.
Breast feeding
Use of Rosemar is generally not advisable when a woman is breast feeding. If you want to take the pill while you are breast-feeding you should contact your doctor.
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
Rosemar does not have any known effect on your ability to drive or use machines. Rosemar contains lactose and sucrose.
If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine.
3. How to take Rosemar
Always take this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
Take one tablet of Rosemar every day, if necessary with a small amount of water. You may take the tablets with or without food, but you should take the tablets every day around the same time.
The strip contains 21 tablets. Next to each tablet is printed the day of the week that it should be taken. If, for example you start on a Wednesday, take a tablet with “WED” next to it. Follow the direction of the arrow on the strip until all 21 tablets have been taken.
Then take no tablets for 7 days. In the course of these 7 tablet-free days (otherwise called a stop or gap week) bleeding should begin. This so-called “withdrawal bleeding” usually starts on the 2nd or 3rd day of the gap week.
On tlie 8“ day alter the last Rosemar tablet (that is, alter the 7-day gap week), start the following strip, even if the bleeding has not stopped. This means that you should start the following strip on the same day of the week and that the withdrawal bleed should occur on the same days each month.
If you use Rosemar in this maimer, you are also protected against pregnancy during tire 7 days that you are not taking a tablet.
Starting the first pack of Rosemar
• If you have not used a contraceptive with hormones in the previous month.
Begin with Rosemar tablet on the first day of the cycle (that is the first day of your menstruation). If you start Rosemar tablet on the first day of your menstruation you are immediately protected against pregnancy. You may also begin on day 2-5 of the cycle, but then you must use extra protective measures (for example, a condom) for tire first 7 days.
• Changing from another combined hormonal contraceptive, or combined contraceptive, vaginal ring or patch.
You can start Rosemar preferably on the day after the last active tablet (tire last tablet containing the active substance) of your previous pill, but at the latest on the day after tire tablet-free days of your previous pill finish (or after the last inactive tablet of your previous pill). When changing from a combined contraceptive vaginal ring or patch, follow the advice of your doctor.
• Changing from a progestogen-only-method (progestogen-only pill, injection, implant or a progestogen-releasing IUD).
You may switch any day from the progestogen-only pill (from an implant or the IUD on the day of its removal, from an injectable when the next injection would be due) but in all of these cases you must use extra protective measures (for example, a condom) for the first 7 days of tablet-taking.
• After a miscarriage.
Follow the advice of your doctor.
• After having a baby.
After having a baby, you can start Rosemar between 21 and 28 days later. If you start later than day 28, you must use a so-called barrier method (for example, a condom) during the first seven days of Rosemar use.
If, after having a baby, you have had intercourse before starting Rosemar (again), you must first be sure that you are not pregnant or you must wait until the next menstrual bleed.
Let your doctor advice you in case you are not sure when to start.
• If you are breastfeeding and want to start Rosemar after having a baby, Read the section on “Breast feeding”.
Use in children and adolescents
There is no data available for use in adolescents below 18 years.
If you take more Rosemar than you should
There are no reports of serious harmful results of taking too many Rosemar tablets.
If you take several tablets at once then you may have symptoms of nausea or vomiting. Young girls may have bleeding from the vagina.
If you have taken too many Rosemar tablets, or you discover that a child has taken some, ask your doctor or pharmacist for advice.
If you forget to take Rosemar
If you are less than 12 hours late in taking your pill, the protection from pregnancy is not reduced. Take the tablet as soon as you remember, and further pills again at the usual time. If you are more than 12 hours late taking a tablet, the protection from pregnancy may be reduced. The greater the number of tablets that you have forgotten, the greater is the risk that the protection from pregnancy is reduced.
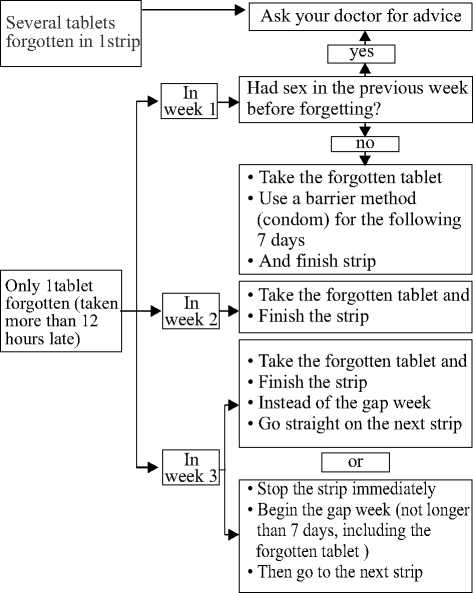
The rrsk of incomplete protectron agarnst pregnancy rs greatest rf you torget a tabiet at the beginning or the end of the strip. Therefore, you should adhere to the following rules:
• More than one tablet forgotten in this strip
Contact your doctor.
• One tablet forgotten in week 1
Take the forgotten tablet as soon as you remember, even if that means that you have to take two tablets at the same time. Take the tablets again at the usual time and use extra precautions for the next 7 days, for example, a condom. If you have had intercourse in the week before the oversight or you have forgotten to start a new strip after the tablet-free period, you must realize that there is a risk of pregnancy. In that case, contact your doctor.
• One tablet forgotten in week 2
Take the forgotten tablet as soon as you remember, even if that means that you have to take two tablets at the same time. Take the tablets again at the usual time. The protection from pregnancy is not reduced, given that you have taken the tablets correctly in the previous 7 days, otherwise extra precaution should be used for the next 7 days.
• One tablet forgotten in week 3
You can choose between two possibilities:
1. Take the forgotten tablet as soon as you remember, even if that means that you have to take two tablets at the same time. Take the tablets again at the usual time. Instead of the tablet-free period go straight on to the next strip.
Most likely, you will have a period (withdrawal bleed) at the end of the second strip but you may also have spotting or breakthrough bleeding during the second strip.
2. You can also stop the strip and go directly to the tablet-free period of 7 days (record the day on which you forgot your tablet). If you want to start a new strip on your fixed start day, make the tablet-free period less than 7 days.
If you follow either of these two recommendations, you will remain protected against pregnancy.
If you have forgotten any of the tablets in a strip, and you do not have bleeding in the first tablet-free period, this may mean that you are pregnant. You must contact your doctor before you go on to the next strip.
What must you do in the case of vomiting or severe diarrhoea
[f you vomit within 3-4 hours of taking a tablet or you have severe diarrhoea, there is a risk that the active substances in the pill are not fully adsorbed into your body. The situation is similar to if you forget a tablet. After vomiting or diarrhoea, you must take another tablet from a reserve strip as soon as possible. If possible take it within 12 hours of when you normally take your pill. If this is not possible or 12 hours have passed, you should follow the advice given under ‘if you forget to take Rosemar.
Delay of menstrual period: what must you know
Even if not recommended, delay of your menstrual period (withdrawal bleed) is possible by going straight on to a new strip of Rosemar instead of the tablet-free period, to the end of the second strip. You may experience spotting (drops or flecks of blood) or breakthrough bleeding while using the second strip. After the usual tablet-free period of 7 days, continue with the following strip.
You might ask your doctor for advice before deciding to delay your menstrual period
Change of the first day of your menstrual period: what you must know
If you take the tablets according to the instructions, then your menstrual period/ withdrawal bleed will begin in the tablet-free week. If you have to change this day, do this by making the tablet-free period shorter (but never longer!) For example, if yoiu tablet-free period begins on a Friday, and you want to change this to a Tuesday (3 days earlier) you must start a new strip 3 days earlier than usual. If you make the tablet-free period very short (for example, 3 days or less) then it may be that you do not have any bleeding during this tablet-free period. You may then experience spotting (droplets oi flecks of blood) or breakthrough bleeding.
If you are not sure how to proceed, contact your doctor for advice.
If you stop taking Rosemar
You can stop taking Rosemar whenever you want. If you do not want to become pregnant, ask you doctor for advice about other reliable methods of birth control.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Common side effects (affecting more than 1 in 100, but less than 1 in 10 women): Mood swings, headache, abdominal pain (stomach ache), acne, breast pain, weight gain, nausea
Uncommon side effects (affecting more than 1 in 1000 but less than 1 in 100 women): Vomiting, diarrhoea, fluid retention, migraine, decreased libido (interest in sex), breast enlargement, itchy red rush of the skin (urticaria)
Rare side effects (affecting less than 1 in 1000 women):
Contact lens intolerance, allergic reactions, weight loss, increased libido (interest in sex, breast discharge, vaginal discharge, allergic reactions which can sometimes be severe with swelling of the skin and/or mucous membranes (erythema nodosum & eruthema multifonne)
Other serious side effects you should be aware off are also mentioned in section 2 of this leaflet (Do not take Rosemar if you & Take special care with Rosemar).
These include:
Blood clot disorders High blood pressure;
Liver tumours;
Swelling of the skin (angioedema)
Occurrence or deterioration of conditions such as: Crohn’s disease, epilepsy, migraine Etc
If any of the side effects gets serious, or if you notice any side eliects not listed m this leaflet, please tell your doctor or pharmacist
Additional side effects in children and adolescents
Not relevant
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mlira.gov.uk/yellowcard By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Rosemar
Keep this medicine out of the sight and reach of children.
Store below 25° C
Do not use this medicine after the expiry date which is stated on the carton.
The expiry date refers to the last day of that month.
Do not use this medicine if you notice description of the visible signs of deterioration.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information What Rosemar contains
The active substances are Levonorgestrel (150 meg) and Ethinylestradiol (30 meg)
The other ingredients are Lactose Monohydrate, Maize Starch, Povidone K-25, Sucrose, Talc, Calcium carbonate, Povidone K-90, Glycerin, Macrogol 6000, Titanium dioxide, Magnesium Stearate, Camauba Wax.
What Rosemar looks like and contents of the pack
Rosemar tablets are white, circular, biconvex and sugar coated.
Each blister pack contains 21 tablets.
Rosemar is sold in cartons of 1, 3, 6 or 13 blister packs.
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer
Famy Care Europe Ltd.
One Wood Street London, EC2V 7WS United Kingdom
Rosemar is manufactured by:
Accord Healthcare Limited Sage House, 319 Pinner Road,
North Harrow, Middlesex HA1 4HF,
United Kingdom