Sayana 104 Mg/0.65 Ml Suspension For Injection
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
SAYANA®104mg/0.65mL suspension for injection
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
SAYANA single dose pre-filled syringe containing 104mg medroxyprogesterone acetate (MPA) in 0.65mL suspension for injection.
Excipients with known effect:
Methyl parahydroxybenzoate - 1.04mg per 0.65ml Propyl parahydroxybenzoate - 0.0975mg per 0.65ml Sodium - 2.47mg per 0.65ml
For the full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Suspension for injection
White to off-white homogeneous suspension
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
SAYANA is indicated for long-term female contraception. Each subcutaneous injection prevents ovulation and provides contraception for at least 13 weeks (+/- 1 week). However, it should be taken into consideration that the return to fertility (ovulation) may be delayed for up to one year (see section 4.4).
Since loss of bone mineral density (BMD) may occur in females of all ages who use SAYANA long-term (see section 4.4 Special Warnings and Precautions for Use), a risk/benefit assessment, which also takes into consideration the decrease in BMD that occurs during pregnancy and/or lactation, should be considered.
Use in Adolescents (12-18 years)
In adolescents, use of SAYANA is only indicated when other contraceptive methods are considered unsuitable or unacceptable, due to unknown long-term effects of bone loss associated with SAYANA during the critical period of bone accretion (see section 4.4).
SAYANA has not been studied in women under the age of 18 years but data is available for intramuscular MPA in this population.
4.2 Posology and method of administration
The prefilled syringe of SAYANA should be vigorously shaken just before use to ensure that the dose being given represents a uniform suspension. The treatment should be initiated by a doctor or healthcare assistant and administered as a subcutaneous injection (SC) into the anterior thigh or abdomen. The medication should be injected slowly until the syringe is empty, which should take about 5-7 seconds. For instructions on how to prepare SAYANA before administration, see section 6.6.
Step 1: Choosing and preparing the injection area.
Choose the injection area in either the upper thigh or abdomen, see shaded areas (Diagram 1). Avoid bony areas and the umbilicus.
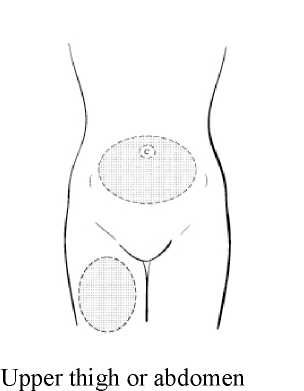
Diagram 1
Use an alcohol pad to wipe the skin in the injection area you have chosen. Allow the skin to dry.
While continuing to hold the syringe barrel firmly, remove the protective plastic needle cover from the needle without twisting, making sure the needle is still firmly attached to the syringe (Diagram 2).

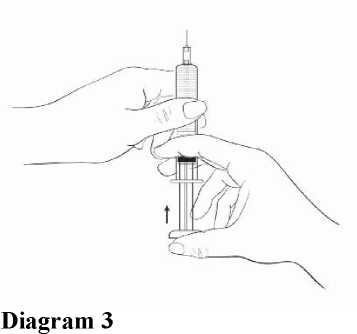
While holding the syringe with the needle pointing upward, gently push in the plunger until the medicine is up to the top of the syringe. There should be no air within the barrel (Diagram 3).
Step 2: Injecting the dose.
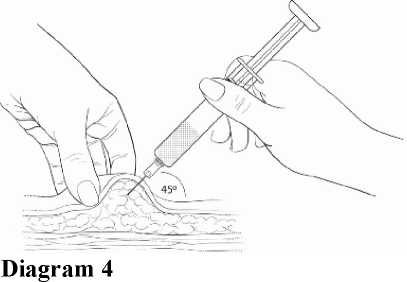
Gently grasp and squeeze a large area of skin in the chosen injection area between the thumb and fore-finger, pulling it away from the body. Insert the needle at a 45 degree angle so that most of the needle is in the fatty tissue. The plastic hub of the needle should be nearly or almost touching the skin (Diagram 4).
Inject the medication slowly until the syringe is empty (Diagram 5).
• This should take about 5-7 seconds.
• It is important that the entire dose of Sayana is given
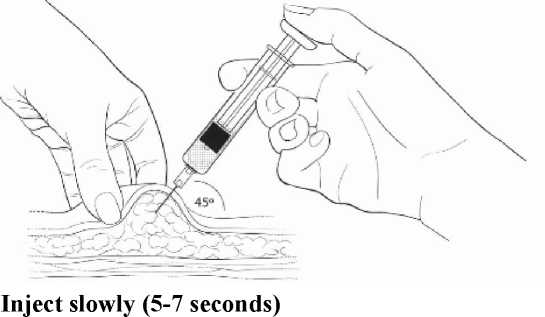
Diagram 5
When the entire dose is completely injected, gently pull the needle out of the skin.
Use a clean cotton pad to press lightly on the injection area for a few seconds. Do NOT rub the area.
Adults
First Injection-. To provide contraceptive cover in the first cycle of use, an injection of 104mg SC should be given during the first five days of a normal menstrual cycle. If the injection is carried out according to these instructions, no additional contraceptive measure is required.
Further doses: The second and subsequent injections should be given at 13 week intervals, as long as the injection is given no later than seven days after this time, no additional contraceptive measures (e.g. barrier) are required. If the interval from the preceding injection is greater than 14 weeks (13 weeks plus 7 days) for any reason, then pregnancy should be excluded before the next injection is given. The efficacy of SAYANA depends on adherence to the recommended dosage schedule of administration.
Post-Partum: If the patient is not breast-feeding, the injection should be given within 5 days post-partum (to increase assurance that the patient is not pregnant). If the injection is to be given at another time then pregnancy should be excluded.
If the patient is breast-feeding, the injection should be given no sooner than six weeks post-partum, when the infant's enzyme system is more developed (see section 4.6).
There is evidence that women prescribed SAYANA in the immediate puerperium can experience prolonged and heavy bleeding. Because of this, the drug should be used with caution in the puerperium. Women who are considering use of the product immediately following delivery or termination should be advised that the risk of heavy or prolonged bleeding may be increased. Doctors are reminded that in the non-breast-feeding, post-partum patient, ovulation may occur as early as week 4.
Switching from other Methods of Contraception : When switching from other contraception methods, SAYANA should be given in a manner that ensures continuous contraceptive coverage based upon the mechanism of action of both methods, (e.g. patients switching from oral contraceptives should have their first injection of SAYANA within 7 days after their last active pill).
Patients with hepatic impairment: The effect of hepatic disease on the pharmacokinetics of SAYANA is unknown. As SAYANA largely undergoes hepatic elimination it may be poorly metabolised in patients with severe liver insufficiency (see Section 4.3 - Contraindications).
Patients with renal impairment: The effect of renal disease on the pharmacokinetics of SAYANA is unknown. No dosage adjustment should be necessary in women with renal insufficiency, since SAYANA is almost exclusively eliminated by hepatic metabolism.
Paediatric population
SAYANA is not indicated before menarche (see Section 4.1 Therapeutic Indications). Data in adolescent females (12-18 years) is available for IM administration of MPA (see Section 4.4 Special Warnings and Precautions for Use and Section 5.1 Pharmacodynamic properties). Other than concerns about loss of BMD, the safety and effectiveness of SAYANA is expected to be the same for adolescents after menarche and adult females
4.3 Contraindications
• SAYANA is contra-indicated in patients with a known hypersensitivity to MPA or any of its excipients listed in section 6.1.
• SAYANA is contra-indicated if pregnancy is known or suspected.
• SAYANA is contra-indicated in women with known or suspected malignancy of the breast or genital organs.
• SAYANA is contra-indicated in patients with undiagnosed vaginal bleeding.
• SAYANA is contra-indicated in patients with severe hepatic impairment.
• SAYANA is contra-indicated in patients with metabolic bone disease.
• SAYANA is contra-indicated in patients with active thromboembolic disease and in patients with current or past history of cerebrovascular disease.
4.4 Special warnings and precautions for use
Loss of Bone Mineral Density :
Use of SAYANA reduces serum oestrogen levels and is associated with significant loss of BMD due to the known effect of oestrogen deficiency on the bone remodelling system. Bone loss is greater with increasing duration of use, however BMD appears to increase after SAYANA is discontinued and ovarian oestrogen production increases.
This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. It is unknown if use of SAYANA by younger women will reduce peak bone mass and increase the risk for fracture in later life.
A study to assess the BMD effects of medroxyprogesterone acetate IM (Depo-Provera, DMPA) in adolescent females showed that its use was associated with a significant decline in BMD from baseline. In the small number of women who were followed-up, mean BMD recovered to around baseline values by 1- 3 years after discontinuing treatment. In adolescents, SAYANA may be used, but only after other methods of contraception have been discussed with the patients and considered to be unsuitable or unacceptable.
In women of all ages, careful re-evaluation of the risks and benefits of treatment should be carried out in those who wish to continue use for more than 2 years. In particular, in women with significant lifestyle and/or medical risk factors for osteoporosis, other methods of contraception should be considered prior to use of SAYANA.
Significant risk factors for osteoporosis include:
• Alcohol abuse and/or tobacco use
• Chronic use of drugs that can reduce bone mass, e.g., anticonvulsants or corticosteroids
• Low body mass index or eating disorder, e.g., anorexia nervosa or bulimia
• Previous low trauma fracture
• Family history of osteoporosis
A retrospective cohort study using data from the General Practice Research Database (GPRD) reported that women using MPA injections (DMPA), have a higher risk of fracture compared with contraceptive users with no recorded use of DMPA (incident rate ratio 1.41, 95% CI 1.35-1.47 for the five year followup period); it is not known if this is due to DMPA, or to other related lifestyle factors which have a bearing on fracture rate. By contrast, in women using DMPA, the fracture risk before and after starting DMPA was not increased (relative risk 1.08, 95% CI 0.92-1.26). Importantly, this study could not determine whether use of DMPA has an effect on fracture rate later in life.
For further information on BMD changes in both adult and adolescent females, as reported in recent clinical studies, refer to section 5.1 (Pharmacodynamic Properties). Adequate intake of calcium and Vitamin D, whether from the diet or from supplements, is important for bone health in women of all ages.
Menstrual Irregularities:
Most women using SAYANA experienced alteration of menstrual bleeding patterns. Patients should be appropriately counseled concerning the likelihood of menstrual disturbance and the potential delay in return to ovulation. As women continued using SAYANA, fewer experienced irregular bleeding and more experienced amenorrhea. After receiving the fourth dose, 39% of women experienced amenorrhea during month 6. During month twelve, 56.5% of women experienced amenorrhea. The changes in menstrual patterns from the three contraception trials are presented in Figures 1 and 2. Figure 1 shows the increase in the percentage of women experiencing amenorrhea over the 12 month study. Figure 2 presents the percentage of women experiencing spotting only, bleeding only, and bleeding and spotting over the same time period. In addition to amenorrhea, altered bleeding patterns included intermenstrual bleeding, menorrhagia and metrorrhagia. If abnormal bleeding associated with SAYANA persists or is severe, appropriate investigation and treatment should be instituted.
Figure 1. Percent of SAYANA-Treated Women with Amenorrhea per 30-Day Month Contraception Studies (ITT Population, N=2053)
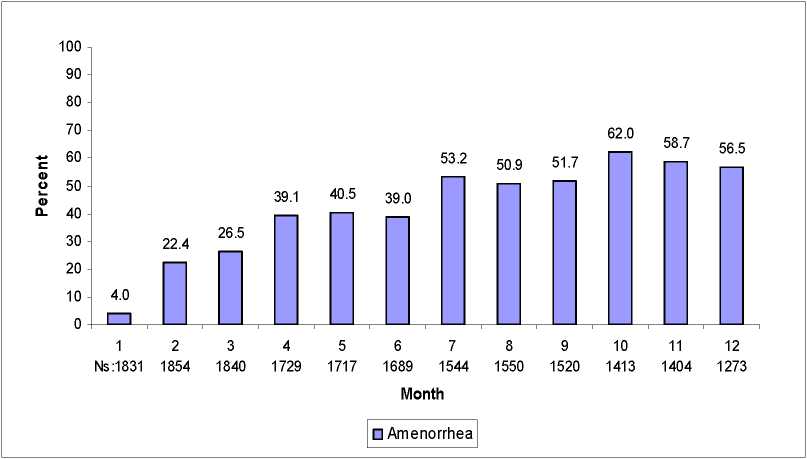
Figure 2. Percent of SAYANA-Treated Women with Bleeding and/or Spotting per 30-Day Month Contraception Studies (ITT Population, N=2053)
100
90
80
70
60
50
40
30
20
10
0
12 Ns:1831 1854
3
1840
4
1729
5
1717
6 7 8
1689 1544 1550
9
1520
10 11 12 1413 1404 1273
Month
□ Spotting Only □ Bleeding Only □ Bleeding and Spotting
Cancer Risks:
Long-term case-controlled surveillance of DMPA-IM 150mg users found no overall increased risk of ovarian, liver, or cervical cancer and a prolonged, protective effect of reducing the risk of endometrial cancer in the population of users.
Breast cancer is rare among women under 40 years of age whether or not they use hormonal contraceptives.
Results from some epidemiological studies suggest a small difference in the risk of having the disease in current and recent users compared with never-users. Any excess risk in current and recent DMPA users is small in relation to the overall risk of breast cancer, particularly in young women (see below), and is not apparent after 10 years since last use. Duration of use does not seem to be important.
Possible number of additional cases of breast cancer diagnosed up to 10 years after stopping injectable progestogens*
|
Age at last use of DMPA |
No of cases per 10,000 women who are never-users |
Possible additional cases per 10,000 DMPA users |
|
20 |
Less than 1 |
Much less than 1 |
|
30 |
44 |
2-3 |
|
40 |
160 |
10 |
*based on use for 5 years
Thromboembolic Disorders
Although MPA has not been causally associated with the induction of thrombotic or thromboembolic disorders, any patient who develops such an event, e.g. pulmonary embolism, cerebrovascular disease, retinal thrombosis or deep venous thrombosis, while undergoing therapy with SAYANA should not be readministered the drug. Women with a prior history of thromboembolic disorders have not been studied in clinical trials and no information is available that would support the safety of SAYANA use in this population.
Anaphylaxis and Anaphylactoid Reaction
If an anaphylactic reaction occurs appropriate therapy should be instituted. Serious anaphylactic reactions require emergency medical treatment.
Ocular Disorders
Medication should not be re-administered pending examination if there is a sudden partial or complete loss of vision or if there is a sudden onset of proptosis, diplopia, or migraine. If examination reveals papilledema or retinal vascular lesions, medication should not be re-administered.
Precautions Weight Changes
Weight changes are common but unpredictable. In the phase 3 studies body weight was followed over 12 months. Half (50%) of women remained within 2.2 Kg of their initial body weight. 12% of women lost more than 2.2 Kg, and 38% of women gained more than 2.3 Kg.
Fluid Retention
There is evidence that progestogens may cause some degree of fluid retention, and as a result, caution should be exercised in treating any patient with a preexisting medical condition that might be adversely affected by fluid retention.
Return of Ovulation
Following a single dose of SAYANA, the cumulative rate of return to ovulation as measured by plasma progesterone was 97.4% (38/39 patients) by one year after administration. After the 14-week therapeutic window, the earliest return to ovulation was one week, and the median time to ovulation was 30 weeks. Women should be counselled that there is a potential for delay in return to ovulation following use of the method, regardless of the duration of use. It is recognised, however, that amenorrhoea and/or irregular menstruation upon discontinuation of hormonal contraception may be due to an underlying disorder associated with menstrual irregularity especially polycystic ovarian syndrome.
Psychiatric Disorders
Patients with a history of treatment for clinical depression should be carefully monitored while receiving SAYANA.
Protection Against Sexually Transmitted Diseases
Patients should be counselled that SAYANA does not protect against HIV infection (AIDS) or other sexually transmitted diseases.
Carbohydrate/Metabolism
Some patients receiving progestogens may exhibit a decrease in glucose tolerance. Diabetic patients should be carefully observed while receiving such therapy.
Liver Function
If jaundice develops in any woman receiving SAYANA, consideration should be given to not re-administer the medication. (See section 4.3)
Hypertension and Lipid disorders
Limited evidence suggests that there is a small increased risk of cardiovascular events among women with hypertension or with lipid disorders who used progestogen-only injectables. If hypertension occurs under SAYANA treatment and/or the increase in hypertension cannot adequately be controlled by antihypertensive medication, treatment with SAYANA should be stopped. Additional risk factors for arterial thrombotic disorders include: Hypertension, smoking, age, lipid disorders, migraine, obesity, positive family history, cardiac valve disorders, atrial fibrillation.
SAYANA should be used cautiously in patients with one or more of these risk factors.
Other conditions
The following conditions have been reported both during pregnancy and during sex steroid use, but an association with the use of progestagens has not been established: jaundice and/or pruritus related to cholestasis; gallstone formation; porphyria; systemic lupus erythematosus; hemolytic uraemic syndrome; Sydenham's chorea; herpes gestationis; otosclerosis-related hearing loss.
Laboratory Tests
The pathologist should be advised of progestogen therapy when relevant specimens are submitted. The physician should be informed that certain endocrine and liver function tests, and blood components might be affected by progestogen therapy:
a) Plasma/urinary steroids are decreased (e.g. progesterone, estradiol, pregnanediol, testosterone, cortisol)
b) Plasma and urinary gonadotropin levels are decreased (e.g., LH, FSH).
c) Sex-hormone-binding-globulin (SHBG) concentrations are decreased. Excipients
As this product contains methylparahydroxbenzoate and propylparahydroxbenzoate, it may cause allergic reactions (possibly delayed), and exceptionally, bronchospasm. This medicinal product contains less than 1 mmol sodium (23mg) per 104mg/0.65 mL, i.e. essentially ‘sodium-free’.
If any of the conditions/risk factors mentioned is present, the benefits of SAYANA use should be weighed against the possible risks for each individual woman and discussed with the woman before she decides to start using it. In the event of aggravation, exacerbation or first appearance of any of these conditions or risk factors, the woman should contact her physician. The physician should then decide on whether SAYANA use should be discontinued.
4.5 Interaction with other medicinal products and other forms of interaction
No interaction studies have been performed with SAYANA.
Interactions with other medical treatments (including oral anticoagulants) have rarely been reported, but causality has not been determined. The possibility of interactions should be borne in mind in patients receiving concurrent treatment with other drugs.
The clearance of medroxyprogesterone acetate is approximately equal to the rate of hepatic blood flow. Because of this fact, it is unlikely that drugs which induce hepatic enzymes will significantly affect kinetics of medroxyprogesterone acetate. Therefore, no dose adjustment is recommended in patients receiving drugs known to affect hepatic metabolizing enzymes.
4.6 Fertility, pregnancy and lactation
Fertility
SAYANA is indicated for the prevention of pregnancy.
Women may experience a delay in return to fertility (conception) following discontinuation of SAYANA (see section 4.4).
Pregnancy
SAYANA is contraindicated in women who are pregnant. Some reports suggest an association between intrauterine exposure to progestational drugs in the first trimester of pregnancy and genital abnormalities in male and female foetuses. If SAYANA is used during pregnancy, or if the patient becomes pregnant while using this drug, the patient should be warned of the potential hazard to the foetus.
One study found that infants from unintentional pregnancies that occurred 1 to 2 months after injection of medroxyprogesterone acetate Injection 150mg IM were at an increased risk of low birth weight; this, in turn, has been associated with an increased risk of neonatal death. However, the overall risk of this is very low because pregnancies while on medroxyprogesterone acetate Injection 150mg IM are uncommon.
Children exposed to MPA in utero and followed to adolescence showed no evidence of any adverse effects on their health including their physical, intellectual, sexual or social development.
Lactation
Low detectable amounts of drug have been identified in the milk of mothers receiving MPA. In nursing mothers treated with medroxyprogesterone acetate injection 150mg IM, milk composition, quality, and amount are not adversely affected. Neonates and infants exposed to MPA from breast milk have been studied for developmental and behavioural effects through puberty. No adverse effects have been noted. However, due to limitations of the data regarding the effects of MPA in breastfed infants less than six weeks old, SAYANA should be given no sooner than six weeks post-partum when the infant’s enzyme system is more developed.
4.7 Effects on ability to drive and use machines
SAYANA has no influence on the ability to drive and use machines.
4.8 Undesirable effects
Events from clinical trials:
The table below provides a listing of adverse drug reactions with frequency based on all-causality data from clinical studies that enrolled 2053 women
who received DMPA-SC for contraception. The most frequently (>5%) reported adverse drug reactions were headache (8.9%), metrorrhagia (7.1%), weight increased (6.9%), amenorrhoea (6.3%) and injection site reactions (any type, 6.1%).
Adverse reactions are listed according to the following categories. These are as follows:
Very Common(>1/10)
Common (>1/100 to <1/10)
Uncommon (>1/1,000 to <1/100)
Rare (>1/10,000 to <1/1,000)
Frequency not known (cannot be estimated from the available data)
Events from post-marketing surveillance:
In addition, adverse events of medical significance obtained from postmarketing data with the use of injectable DMPA (IM or SC) are also included in the list below:
|
System organ class |
Very Common |
Common |
Uncommon |
Rare |
Not known |
|
Neoplasms benign, malignant and unspecified (including cysts and polyps) |
Breast cancer (see Section 4.4) | ||||
|
Immune system disorders |
Drug hypersensitivity (see Section 4.4) |
Anaphylactic reaction, Anaphylactoid reaction, Angioedema (see Section 4.4) | |||
|
Metabolism and nutrition disorders |
Fluid retention (see Section 4.4), Increased appetite, Decreased appetite | ||||
|
Pyschiatric disorders |
Depression, Insomnia, Anxiety, Libido decreased, Affective disorder, Irritability |
Nervousness, Emotional disorder, Anorgasmia | |||
|
Nervous system disorders |
Dizziness, Headache |
Migraine, Somnolence |
Seizure | ||
|
Ear and labyrinth disorders |
Vertigo | ||||
|
Cardiac disorders |
Tachycardia | ||||
|
Vascular disorders |
Varicose vein, Hypertension (see Section 4.4), |
Pulmonary embolism, Embolism and thrombosis (see |
|
Hot flush |
Section 4.4), Thrombophlebitis | ||||
|
Gastrointestinal disorders |
Abdominal pain, Nausea |
Abdominal distension | |||
|
Hepatobiliary disorders |
Jaundice, Hepatic function abnormal (see Section 4.4) | ||||
|
Skin and subcutaneous tissue disorders |
Acne |
Alopecia, Hirsutism Dermatitis, Ecchymosis, Chloasma, Rash, Pruritus, Urticaria, |
Lipodystrophy acquired |
Skin striae | |
|
Musculoskeletal and connective tissue disorders |
Back pain, Pain in extremity |
Arthralgia, Muscle spasms |
Osteoporosis, Osteoporotic fractures | ||
|
Reproductive system & breast Disorders |
Menometrorrhagia, Metrorrhagia, Menorrhagia (see Section 4.4), Dysmenorrhoea, Amenorrhea, Vaginitis, Breast pain |
Ovarian cyst, Uterine haemorrhage (irregular, increase, decrease), Vaginal discharge, Dyspareunia, Galactorrhoea, Pelvic pain, Vulvovaginal dryness, Premenstrual syndrome, Breast tenderness, Breast enlargement | |||
|
General disorders and administration site conditions |
Fatigue, Injection site reaction, Injection site persistent atrophy/ Indentation/ dimpling, Injection site nodule/ lump, Injection site pain/tenderness |
Pyrexia |
Asthenia | ||
|
Investigations |
Weight increased (see Section 4.4), Smear cervix abnormal |
Bone density decreased (see Section 4.4), Glucose tolerance decreased (see Section 4.4), Hepatic enzyme abnormal |
Weight decreased (see Section 4.4) |
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance
of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via Yellow Card Scheme Website: www.mhra.gov.uk/yellowcard
4.9 Overdose
No positive action is required other than cessation of therapy.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
ATC Code: G03AC06
MPA is an analogue of 17 a-hydroxyprogesterone with anti-estrogenic, antiandrogenic and antigonadotrophic effects.
SAYANA MPA injectable suspension inhibits the secretion of gonadotropins which, in turn, prevents follicular maturation and ovulation and causes thickening of cervical mucus which inhibits sperm entry into the uterus. These actions produce its contraceptive effect.
BMD Changes in Adult Women
A study comparing changes in BMD in women using SAYANA with women using medroxyprogesterone acetate injection (150 mg IM) showed no significant differences in BMD loss between the two groups after two years of treatment. Mean percent changes in BMD in the SAYANA group are listed in Table 1.
Table 1. Mean Percent Change from Baseline in BMD in Women Using SAYANA by Skeletal Site
|
Time on Treatment |
Lum |
bar Spine |
Tota |
Hip |
Femoral Neck | |
|
N |
Mean % Change (95% CI) |
N |
Mean % Change (95% CI) |
N |
Mean % Change (95% CI) | |
|
1 year |
166 |
-2.7 (-3.1 to -2.3) |
166 |
-1.7 (-2.1 to -1.3) |
166 |
-1.9 (-2.5 to -1.4) |
|
2 year |
106 |
- 4.1 (-4.6 to -3.5) |
106 |
-3.5 (-4.2 to -2.7) |
106 |
-3.5 (-4.3 to -2.6) |
In another controlled, clinical study adult women using medroxyprogesterone acetate injection (150 mg IM) for up to 5 years showed spine and hip mean BMD decreases of 5-6%, compared to no significant change in BMD in the control group. The decline in BMD was more pronounced during the first two years of use, with smaller declines in subsequent years. Mean changes in lumbar spine BMD of -2.86%, -4.11%, -4.89%, -4.93% and -5.38% after 1, 2, 3, 4 and 5 years, respectively, were observed. Mean decreases in BMD of the total hip and femoral neck were similar. Please refer to Table 2 below for further details.
After stopping use of medroxyprogesterone acetate injection (150 mg IM), BMD increased towards baseline values during the post-therapy period. A longer duration of treatment was associated with a slower rate of BMD recovery.
Table 2. Mean Percent Change from Baseline in BMD in Adults by Skeletal Site and Cohort after 5 Years of Therapy with Medroxyprogesterone acetate 150 mg IM and after 2 Years Post-Therapy or 7 Years of Observation (Control)
|
Time in Study |
Spine |
Total Hip |
Femoral Neck | |||
|
Medroxy progesterone acetate |
Control |
Medroxy progesterone acetate |
Control |
Medroxy progesterone acetate |
Control | |
|
5 years* |
n=33 -5.38% |
n=105 0.43% |
n=21 -5.16% |
n=65 0.19% |
n=34 -6.12% |
n=106 -0.27% |
|
7 years** |
n=12 -3.13% |
n=60 0.53% |
n=7 -1.34% |
n=39 0.94% |
n=13 -5.38% |
n=63 -0.11% |
*The treatment group consisted of women who received medroxyprogesterone acetate injection (150 mg IM) for 5 years and the control group consisted of women who did not use hormonal contraception for this time period.
**The treatment group consisted of women who received medroxyprogesterone acetate Injection (150 mg IM) for 5 years and were then followed up for 2 years post-use and the control group consisted of women who did not use hormonal contraceptive for 7 years.
BMD Changes in Adolescent Females (12-18 years)
Results from an open-label, non-randomised, clinical study of medroxyprogesterone acetate Injection (150 mg IM every 12 weeks for up to 240 weeks (4.6 years), followed by post-treatment measurements) in adolescent females (12-18 years) also showed that medroxyprogesterone acetate IM use was associated with a significant decline in BMD from baseline. Among subjects who received >4 injections/60-week period, the mean decrease in lumbar spine BMD was - 2.1 % after 240 weeks (4.6 years); mean decreases for the total hip and femoral neck were -6.4 % and -5.4 %, respectively. Post-treatment follow-up showed that, based on mean values, lumbar spine BMD recovered to baseline levels approximately 1 year after treatment was discontinued and that hip BMD recovered to baseline levels approximately 3 years after treatment was discontinued. However, it is important to note that a large number of subjects discontinued from the study, therefore these results are based on a small number of subjects (n=71 at 60 weeks and n=25 at 240 weeks after treatment discontinuation). In contrast, a non-comparable cohort of unmatched, untreated subjects, with different baseline bone parameters from the DMPA users, showed mean BMD increases at 240 weeks of 6.4%, 1.7% and 1.9% for lumbar spine, total hip and femoral neck, respectively.
5.2 Pharmacokinetic properties
The pharmacokinetic parameters of MPA following a single SC injection of SAYANA are shown in Table 1.
Table 1. Pharmacokinetic Parameters of MPA
After a Single SC Injection of SAYANA in Healthy Women (n = 42)
|
(ng/mL) |
(day) |
(ng/mL) |
(ngday/mL) |
(ngday/mL) |
(day) | |
|
Mean Min Max Cmax = pea |
1.56 |
8.8 |
0.402 |
66.98 |
92.84 |
43 |
|
0.53 |
2.0 |
0.133 |
20.63 |
31.36 |
16 | |
|
3.08 c serum coi |
80.0 centratio |
0.733 n; Tmax = ti |
139.79 me when Cmax is |
162.29 observed; AUC0 |
114 _9i = area | |
under the concentration-time curve over 91 days; tl = terminal half-life; 1 nanogram = 103 picogram.
General Characteristics Absorption
MPA absorption from the SC injection site to achieve therapeutic levels is relatively prompt. The mean Tmax attained approximately one week after injection. The peak MPA concentrations (Cmax) generally range from 0.5 to 3.0ng/mL with a mean Cmax of 1.5ng/mL after a single SC injection.
Effect of Injection Site
SAYANA was administered into the anterior thigh or the abdomen to evaluate effects on MPA concentration-time profile. MPA trough concentrations (Cmin; Day 91) were similar for the two injection locations, suggesting that injection site does not negatively affect the contraceptive efficacy.
Distribution
Plasma protein binding of MPA averages 86%. MPA binding occurs primarily to serum albumin; no binding of MPA occurs with SHBG.
Biotransformation
MPA is extensively metabolised in the liver by P450 enzymes. Its metabolism primarily involves ring A and/or side-chain reduction, loss of the acetyl group, hydroxylation in the 2-, 6-, and 21-positions or a combination of these positions, resulting in more than 10 metabolites.
Elimination
Residual MPA concentrations at the end of the dosing interval (3 months) of SAYANA are generally below 0.5ng/mL, consistent with its apparent terminal half-life of ~40 days after SC administration. Most MPA metabolites are excreted in the urine as glucuronide conjugates with only small amounts excreted as sulfates.
Linearity/non-linearity
Based on single dose data, there was no evidence of non-linearity over the dose range of 50 to 150mg after SC administration. The relationship between the AUC or the Cmin and the SC dose of MPA appeared to be linear. The mean Cmax did not change substantially with increasing dose
Special populations
Race
There were no apparent differences in the pharmacokinetics and/or dynamics of MPA after SC administration of SAYANA among women of all ethnic backgrounds studied. The pharmacokinetics/dynamics of MPA has been evaluated in Asian women in a separate study.
Effect of Body Weight
No dosage adjustment of SAYANA is necessary based on body weight. The effect of body weight on the pharmacokinetics of MPA was assessed in a subset of women (n = 42, body mass index [BMI] ranged from 18.2 to 46.0kg/m2). The AUC0-9i values for MPA were 68.5, 74.8, and 61.8ng -day/mL in women with BMI categories of <25kg/m2, >25 to <30kg/m2, and >30kg/m , respectively. The mean MPA Cmax was 1.65ng/mL in women with BMI <25kg/m2, 1.76ng/mL in women with BMI >25 to <30kg/m2, and 1.40ng/mL in women with BMI >30kg/m , respectively. The range of MPA trough (Cmin) concentrations and the half-lives were comparable for the 3 BMI groups.
Pharmacokinetic/Pharmacodynamic Relationship( s)
From a pharmacodynamic perspective, the duration of ovulation suppression depends upon maintaining therapeutic MPA concentrations throughout the 13 week dosing interval.
5.3 Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity and carcinogenic potential. Medroxyprogesterone acetate has been shown to have adverse effects on reproduction in animals and is contraindicated for use during pregnancy.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Macrogol 3350
Methyl parahydroxybenzoate (E 218)
Propyl parahydroxybenzoate (E 216)
Sodium Chloride Polysorbate 80
Monobasic Sodium Phosphate Monohydrate Disodium Phosphate Dodecahydrate Methionine Povidone
Hydrochloric Acid and/or Sodium Hydroxide for pH adjustment Water for Injection
6.2 Incompatibilities
Not applicable
6.3 Shelf life
Unopened: 5 years
Once opened: use immediately. Discard any unused portion.
6.4 Special precautions for storage
Do not refrigerate or freeze.
6.5 Nature and contents of container
SAYANA suspension for injection is supplied as a disposable pre-filled syringe (type 1 glass Ph.Eur.) containing 0.65ml with plunger stopper and tip cap (bromobutyl rubber).
The pack sizes are one pre-filled syringe with one 26G, 3/82” needle and six pre-filled syringes with six 26G, 3/8” needles.
Not all pack sizes may be marketed.
6.6
Special precautions for disposal
For single use only.
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
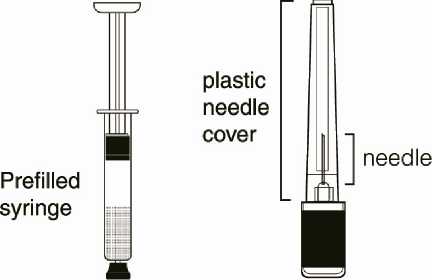
Instructions for Use and Handling Getting ready
Do not refrigerate. Ensure that the medication is at room temperature prior to injection (to ensure appropriate viscosity of the suspension). Make sure the following components (Diagrams 6 and 7) are available.
M
Diagram 6
Diagram 7
SAYANA, as with other parenteral drug products, should be inspected visually for particulate matter and discoloration prior to administration.
Syringe preparation
Gently twist off the protective end cap from the needle to break the seal (Diagram 8). Set aside.

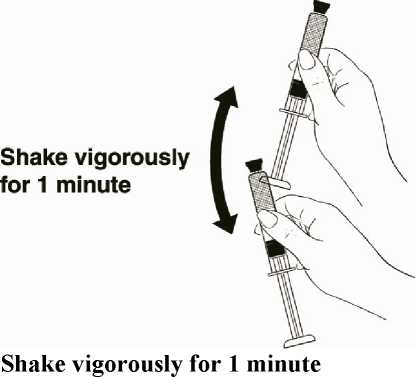
While holding the syringe firmly by the barrel pointing upward, shake it vigorously for at least 1 minute to thoroughly mix the medication (Diagram 9).
Then remove the protective cap from the tip of the syringe barrel.
Diagram 9
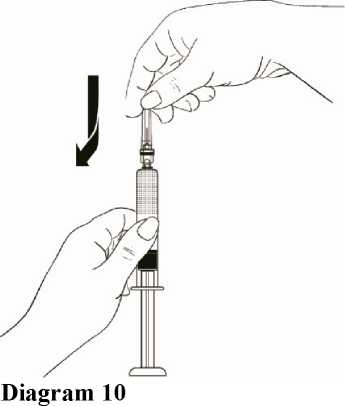
While holding the syringe barrel, attach the needle to the barrel of the syringe firmly by pushing the plastic needle cover down fully with a slight twisting movement (Diagram 10).
7 MARKETING AUTHORISATION HOLDER
Pfizer Limited
Sandwich
Kent
CT13 9NJ United Kingdom
8 MARKETING AUTHORISATION NUMBER(S)
PL 00057/0589
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
26/10/2005 / 30/07/2010
10 DATE OF REVISION OF THE TEXT
05/09/2016