Symbicort 400/12
Page 4 Page 1
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Symbicort Turbohaler
• Keep out of the sight and reach of children.
• Do not store above 30°C.
• Keep the container/ cap tightly closed, in order to protect from moisture.
• Do not use Symbicort Turbohaler after the expiry date printed on the carton or on the label of your Turbohaler. The expiry date refers to the last day of that month.
• Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines that are no longer required. This will help to protect the environment.
• If the medicine become discoloured or show any other signs of deterioration, you should seek the advice of your doctor or pharmacist who will tell you what to do.
6. Further information
What Symbicort Turbohaler contains
The active substances are budesonide and formoterol fumarate dihydrate.
Each inhaled dose (the dose leaving the mouthpiece) delivers 320 micrograms of budesonide and 9 micrograms of formoterol fumarate dihydrate. This corresponds to a dispensed dose of 400 micrograms of budesonide and 12 micrograms of formoterol fumarate dihydrate.
What Symbicort Turbohaler looks like and contents of the pack
Symbicort Turbohaler is a multidose powder plastic inhaler with white body and red turning grip and a dose counter. A braille code '6' is embossed on the red turning grip. The inhalation powder is white in colour.
Symbicort Turbohaler is available in packs of 1 Turbohaler and contains 60 doses.
Manufacturer and Product Licence Holder:
Symbicort Turbohaler is manufactured by either of the following manufacturers.
• AstraZeneca AB, Sodertalje, Sweden.
• AstraZeneca GmbH, Wedel, Germany.
• AstraZeneca UK Limited, Cheshire, United Kingdom.
It is procured from within the EU by the Product Licence Holder: Swinghope Ltd, Brandon House, Marlowe Way, Croydon CR0 4XS UK.
PL No: 10380/1594
Leaflet revision date: 10/12/2015
Symbicort® and Turbohaler® are
trade marks of the AstraZeneca group of companies, Sweden.
T05805 Symbicort® 400/12 Turbohaler®, Inhalation Powder
(budesonide/formoterol fumarate)
Patient Information Leaflet
POM
This medicine is available using the above name but will be referred to as Symbicort Turbohaler throughout the Leaflet. Other strengths of symbicort are available.
Read all of this leaflet carefully before you start using this medicine.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If any of the side effects get serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
What is in this leaflet:
1. What Symbicort Turbohaler is and what it is used for
2. Before you use Symbicort Turbohaler
3. How to use Symbicort Turbohaler
4. Possible side effects
5. How to store Symbicort Turbohaler
6. Further information
1. What Symbicort Turbohaler is and
what it is used for
Symbicort Turbohaler is an inhaler. It contains two different medicines: budesonide and formoterol fumarate dihydrate.
• Budesonide belongs to a group of medicines called ‘corticosteroids'. It works by reducing and preventing swelling and inflammation in your lungs.
• Formoterol fumarate dihydrate belongs to a group of medicines called ‘long-acting beta2 adrenoceptor agonists' or ‘bronchodilators'. It works by relaxing the muscles in your airways. This helps you to breathe more easily.
Your doctor has prescribed this medicine to treat asthma or chronic obstructive pulmonary disease (COPD).
Asthma
For asthma, your doctor will prescribe two asthma inhalers: Symbicort Turbohaler and a separate ‘reliever inhaler'.
• Use Symbicort Turbohaler every day. This helps to prevent asthma symptoms from happening.
• Use your ‘reliever inhaler' when you get asthma symptoms, to make it easier to breathe again.
Do not use Symbicort Turbohaler 400/12 as a ‘reliever inhaler'.
Chronic obstructive pulmonary disease (COPD)
Symbicort Turbohaler can also be used to treat the symptoms of COPD in adults. COPD is a long-term disease of the airways in the lungs, which is often caused by cigarette smoking.
2. Before you use Symbicort
Turbohaler
Do not use Symbicort Turbohaler if:
• You are allergic (hypersensitive) to budesonide, formoterol, or the other ingredient, which is lactose (which contains small amounts of milk proteins).
Take special care with Symbicort Turbohaler
Before you use Symbicort Turbohaler, tell your doctor or pharmacist if:
• You are diabetic.
• You have a lung infection.
• You have high blood pressure or you have ever had a heart problem (including an uneven heart beat, a very fast pulse, narrowing of the arteries or heart failure).
• You have problems with your thyroid or adrenal glands.
• You have low levels of potassium in your blood.
• You have severe liver problems.
Taking other medicines
Please tell your doctor or pharmacist if you are using or have recently used any other medicines. This includes medicines that you buy without a prescription and herbal medicines.
In particular, tell your doctor or pharmacist if you are using any of the following medicines:
• Beta-blocker medicines (such as atenolol or propranolol for high blood pressure), including eyedrops (such as timolol for glaucoma).
• Medicines for a fast or uneven heart beat (such as quinidine).
• Medicines like digoxin, often used to treat heart failure.
• Diuretics, also known as ‘water tablets' (such as furosemide). These are used to treat high blood pressure.
• Steroid medicines that you take by mouth (such as prednisolone).
•Xanthine medicines (such as theophylline or aminophylline). These are often used to treat asthma.
• Other bronchodilators (such as salbutamol).
• Tricyclic anti-depressants (such as amitriptyline) and the anti-depressant nefazodone.
• Mono-Amine Oxidase Inhibitors, also known as MAOIs (such as phenelzine).
• Phenothiazine medicines (such as chlorpromazine and prochlorperazine).
• Medicines called ‘HIV-protease inhibitors' (such as ritonavir) to treat HIV infection.
• Medicines to treat infections (such as ketoconazole, itraconazole, voriconazole, posaconazole, clarithromycin and telithromycin).
•Medicines for Parkinson's disease (such as leva-dopa).
• Medicines for thyroid problems (such as levo-thyroxine).
If any of the above applies to you, or if you are not sure, talk to your doctor or pharmacist before using Symbicort Turbohaler.
Also tell your doctor or pharmacist if you are going to have a general anaesthetic for an operation or for dental work.
Pregnancy, breast-feeding and fertility
• If you are pregnant, or planning to get pregnant, talk to your doctor before using Symbicort Turbohaler - do not use Symbicort Turbohaler unless your doctor tells you to.
• If you get pregnant while using Symbicort Turbohaler, do not stop using Symbicort Turbohaler but talk to your doctor immediately.
• If you are breast-feeding, talk to your doctor before using Symbicort Turbohaler.
Driving and using machines
Symbicort Turbohaler has no or negligible effect on your ability to drive or to use tools or machines.
Important information about some of the ingredients of Symbicort Turbohaler
Symbicort Turbohaler contains lactose, which is a type of sugar. If you have been told by your doctor that you have an intolerance to some sugars, talk to your doctor before using this medicine. The amount of lactose in this medicine does not normally cause problems in people who are lactose intolerant.
The excipient lactose contains small amounts of milk proteins, which may cause an allergic reaction.
3. How to use Symbicort Turbohaler
• Always use Symbicort Turbohaler exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
• It is important to use Symbicort Turbohaler every day, even if you have no asthma or COPD symptoms at the time.
• If you are using Symbicort Turbohaler for asthma, your doctor will want to regularly check your symptoms.
If you have been taking steroid tablets for your asthma or COPD, your doctor may reduce the number of tablets that you take, once you start to use Symbicort Turbohaler. If you have been taking oral steroid tablets for a long time, your doctor may want you to have blood tests from time to time. When reducing oral steroid tablets, you may feel generally unwell even though your chest symptoms may be improving. You might experience symptoms such as a stuffy or runny nose, weakness or joint or muscle pain and rash (eczema). If any of these symptoms bother you, or if symptoms such as headache, tiredness, nausea (feeling sick) or vomiting (being sick) occur, please contact your doctor immediately. You may need to take other medication if you develop allergic or arthritic symptoms. You should speak to your doctor if you are concerned as to whether you should continue to use Symbicort Turbohaler.
Your doctor may consider adding steroid tablets to your usual treatment during periods of stress (for example, when you have a chest infection or before an operation).
Important information about your asthma or COPD symptoms
If you feel you are getting breathless or wheezy while using Symbicort Turbohaler, you should continue to use Symbicort Turbohaler but go to see your doctor as soon as possible, as you may need additional treatment.
Contact your doctor immediately if:
• Your breathing is getting worse or you often wake up at night with asthma.
• Your chest starts to feel tight in the morning or your chest tightness lasts longer than usual.
These signs could mean that your asthma or COPD is not being properly controlled and you may need different or additional treatment immediately.
Asthma
Use your Symbicort Turbohaler 400/12
every day. This helps to prevent asthma symptoms from happening.
Adults (18 years and above)
• The usual dose is 1 inhalation, twice a day.
• Your doctor may increase this to 2 inhalations, twice a day.
• If your symptoms are well controlled, your doctor may ask you to take your medicine once a day.
Adolescents (12 to 17 years)
• The usual dose is 1 inhalation, twice a day.
• If your symptoms are well controlled, your doctor may ask you to take your medicine once a day.
A lower strength of Symbicort Turbohaler is available for children aged from 6 to 11 years.
Symbicort Turbohaler is not recommended to be used in children who are younger than 6 years.
Your doctor (or asthma nurse) will help you to manage your asthma. They will adjust the dose of this medicine to the lowest dose that controls your asthma. However, do not adjust the dose without talking to your doctor (or asthma nurse) first.
Use your separate ‘reliever inhaler’ to treat asthma symptoms when they happen.
Always keep your ‘reliever inhaler’ with you to use when you need it. Do not use Symbicort Turbohaler 400/12 to treat asthma symptoms - use your separate ‘reliever inhaler’.
Chronic Obstructive Pulmonary Disease (COPD)
• Only to be used by adults (aged 18 years and above).
• The usual dose is 1 inhalation twice a day.
Your doctor may also prescribe other bronchodilator drugs, for example anticholinergics (such as tiotropium or ipratropium bromide) for your COPD disease.
Preparing your new Symbicort Turbohaler
Before using your new Symbicort Turbohaler for the first time, you need to prepare it for use as follows:
• Unscrew the cover and lift it off. You may hear a rattling sound.

• Hold your Turbohaler upright with the red grip at the bottom.
• Turn the red grip as far as it will go in one direction. Then turn it as far as it will go in the other direction (it does not matter which way you turn it first). You should hear a click sound.

• Do this again, turning the red grip in both directions.
• Your Turbohaler is now ready for use.
How to take an inhalation
Every time you need to take an inhalation, follow the instructions below.
1. Unscrew the cover and lift it off. You may hear a rattling sound.
2. Hold your Turbohaler upright with the red grip at the bottom.
3. Do not hold the mouthpiece when you load your Turbohaler. To load your Turbohaler with a dose, turn the red grip as far as it will go in one direction. Then turn it as far as it will go in the other direction (it does not matter which way you turn it first). You should hear a click sound. Your Turbohaler is now loaded and ready to use. Only load your Turbohaler when you need to use it.
4. Hold your Turbohaler away from your mouth. Breathe out gently (as far as is comfortable). Do not breathe out through your Turbohaler.
5. Place the mouthpiece gently between your teeth. Close your lips.
Breathe in as deeply and as hard as you can through your mouth.
Do not chew or bite on the mouthpiece.
6. Remove your Turbohaler from your mouth. Then breathe out gently.
The amount of medicine that is inhaled is very small. This means you may not be able to taste it after inhalation. If you have followed the instructions, you can still be confident that you have inhaled the dose and the medicine is now in your lungs.
7. If you are to take a second inhalation, repeat steps 2 to 6.
8. Replace the cover tightly after use.

9. Rinse your mouth with water after your daily morning and/or evening doses, and spit it out.
Do not try to remove or twist the mouthpiece. It is fixed to your Turbohaler and must not be taken off. Do not use your Turbohaler if it has been damaged or if the mouthpiece has come apart from your Turbohaler.
As with all inhalers, caregivers should ensure that children prescribed Symbicort Turbohaler use correct inhalation technique, as described above.
Cleaning your Turbohaler
Wipe the outside of the mouthpiece once a week with a dry tissue. Do not use water or liquids.
When to start using a new Turbohaler
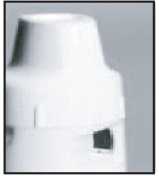
• The dose indicator tells you how many doses (inhalations) are left in your Turbohaler, starting with 60 doses when it is full.
• The dose indicator is marked in intervals of 10 doses. Therefore it does not show every dose.
• When you first see a red mark at the edge of the indicator window, there are approximately 20 doses left. For the last 10 doses, the background of the dose indicator is red. When the ‘0’ on the red background has reached the middle of the window, you must start using your new Turbohaler.
Note:
• The grip will still twist and ‘click’ even when your Turbohaler is empty.
• The sound that you hear as you shake your Turbohaler is produced by a drying agent and not the medicine. Therefore the sound does not tell you how much medicine is left in your Turbohaler.
• If you load your Turbohaler more than once by mistake before taking your dose, you will still only receive one dose. However, the dose indicator will register all the loaded doses.
If you use more Symbicort Turbohaler than you should
It is important that you take your dose as stated on the pharmacist’s label or as advised by your doctor. You should not exceed your prescribed dose without seeking medical advice.
The most common symptoms that may occur if you use more Symbicort Turbohaler than you should are trembling, headache or a rapid heart beat.
If you forget to use Symbicort Turbohaler
• If you forget to take a dose, take it as soon as you remember. However, if it is nearly time for your next dose, skip the missed dose.
• Do not take a double dose to make up for a forgotten dose.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, Symbicort Turbohaler can cause side effects, although not everybody gets them.
If either of the following happen to you, stop using Symbicort Turbohaler and talk to your doctor immediately:
• Swelling of your face, particularly around your mouth (tongue and/or throat and/or difficulty swallowing) or hives together with difficulty breathing (angioedema) and/or sudden feeling of faintness. This may mean that you are having an allergic reaction. This happens rarely, affecting less than 1 in 1,000 people.
• Sudden acute wheezing or shortness of breath immediately after using your inhaler. If either of these symptoms occur, stop using your Symbicort Turbohaler straightaway and use your ‘reliever’ inhaler. Contact your doctor immediately as you may need to have your treatment changed. This happens very rarely, affecting less than 1 in 10,000 people.
Other possible side effects:
Common (affects less than 1 in 10 people)
• Palpitations (awareness of your heart beating), trembling or shaking. If these effects occur, they are usually mild and usually disappear as you continue to use Symbicort Turbohaler.
• Thrush (a fungal infection) in the mouth. This is less likely if you rinse your mouth out with water after using your Symbicort Turbohaler.
• Mild sore throat, coughing and a hoarse voice.
• Headache.
Uncommon (affects less than 1 in 100 people)
• Feeling restless, nervous or agitated.
• Disturbed sleep.
• Feeling dizzy.
• Nausea (feeling sick).
• Fast heart beat.
• Bruising of the skin.
• Muscle cramps.
Rare (affects less than 1 in 1,000 people)
• Rash, itching.
• Bronchospasm (tightening of the muscles in the airways which causes wheezing). If the wheezing comes on suddenly after using Symbicort Turbohaler stop using Symbicort Turbohaler and talk to your doctor immediately.
• Low levels of potassium in your blood.
• Uneven heart beat.
Very rare (affects less than 1 in 10,000 people)
• Depression.
• Changes in behaviour, especially in children.
• Chest pain or tightness in the chest (angina pectoris).
• An increase in the amount of sugar (glucose) in your blood.
• Taste changes, such as an unpleasant taste in the mouth.
• Changes in your blood pressure.
Inhaled corticosteroids can affect the normal production of steroid hormones in your body, particularly if you use high doses for a long time. The effects include:
• changes in bone mineral density (thinning of the bones)
• cataract (clouding of the lens in the eye)
• glaucoma (increased pressure in the eye)
• a slowing of the rate of growth of children and adolescents
• an effect on the adrenal gland (a small gland next to the kidney).
These effects are much less likely to happen with inhaled corticosteroids than with corticosteroid tablets.
T05805
T3
O