Tegretol 250Mg Suppositories
PACKAGE LEAFLET: INFORMATION FOR THE USER
TEGRETOL® 125 and 250 mg Suppositories (carbamazepine)
What you need to know about Tegretol Suppositories
Your doctor has decided that you need this medicine to help treat your condition.
Please read this leaflet carefully before you start to use the suppositories. It contains important information. Keep the leaflet in a safe place because you may want to read it again.
If you have any other questions, or if there is something you don’t understand, please ask your doctor or pharmacist.
This medicine has been prescribed for you. Never give it to someone else. It may not be the right medicine for them even if their symptoms seem to be the same as yours.
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist.
In this leaflet:
1. What Tegretol Suppositories are and what they are used for
2. Things to consider before you are treated with Tegretol Suppositories
3. How to use Tegretol Suppositories
4. Possible side effects
5. How to store Tegretol Suppositories
6. Further information
1. What Tegretol Suppositories are and what they are used for
Carbamazepine, the active ingredient in Tegretol Suppositories is an anti-convulsant medicine (prevents fits).
Tegretol Suppositories are used to treat some forms of epilepsy. They are useful in the short term, (maximum 7 days), for patients who cannot take medicines by mouth, e.g. after surgery or if unconscious.
2. Things to consider before you are treated with Tegretol Suppositories
Some people MUST NOT have Tegretol Suppositories. Make sure your doctor knows if:
• you think you may be hypersensitive (allergic) to carbamazepine or similar drugs such as oxcarbazepine (Trileptal), or to any of a related group of drugs known as tricyclic antidepressants (such as amitriptyline or imipramine). If you are allergic to carbamazepine there is a one in four (25%) chance that you could also have an allergic reaction to oxcarbazepine.
• you think you may be allergic to any of the other ingredients of Tegretol Suppositories (these are listed at the end of the leaflet). Signs of a hypersensitivity reaction include swelling of the face or mouth (angioedema), breathing problems, runny nose, skin rash, blistering or peeling.
• you have any heart problems,
• you have ever had problems with your bone marrow,
• you have a blood disorder called porphyria,
• you have taken drugs called monoamine oxidase inhibitors (MAOIs), used to treat depression, within the last 14 days.
A small number of people being treated with anti-epileptics such as carbamazepine have had thoughts of harming or killing themselves. If at any time you have these thoughts, immediately contact your doctor.
Serious skin rashes (Stevens- Johnson syndrome, toxic epidermal necrolysis) have been reported with the use of carbamazepine. Frequently, the rash can involve ulcers of the mouth, throat, nose, genitals and conjunctivitis (red and swollen eyes). These serious skin rashes are often preceded by influenza-like symptoms fever, headache, body ache (flu-like symptoms). The rash may progress to widespread blistering and peeling of the skin. The highest risk for occurrence of serious skin reactions is within the first months of treatment.
These serious skin reactions can be more common in people from some Asian countries. The risk of these reactions in patients of Han Chinese or Thai origin may be predicted by testing a blood sample of these patients. Your doctor should be able to advise if a blood test is necessary before taking carbamazepine.
If you develop a rash or these skin symptoms, stop taking carbamazepine and contact your doctor immediately.
You should also ask yourself these questions before you have Tegretol Suppositories. If the answer to any of these questions is YES, discuss your treatment with your doctor or pharmacist because Tegretol Suppositories might not be the right medicine for you.
• Are you pregnant or planning to become pregnant?
• Are you breastfeeding?
• Do you suffer from the sort of epilepsy where you get mixed seizures which include absences?
• Do you have any mental illness?
• Are you allergic to an epilepsy medicine called phenytoin?
• Do you have liver problems?
• Do you have kidney problems associated with low sodium blood level or do you have kidney problems and you are taking certain medicines that lower sodium blood levels (diuretics such as hydrochlorothiazide, furosemide)?
• Are you elderly?
• Do you have any eye problems such as glaucoma (increased pressure in the eye) or do you have difficulty retaining your urine?
Are you taking other medicines?
Because of the way that Carbamazepine works, it can affect, and be affected by, lots of other things that you might be eating or medicines that you are taking. It is very important to make sure that your doctor knows all about what else you are taking, including anything that you have bought from a chemist or health food shop. It may be necessary to change the dose of some medicines, or stop taking something altogether.
Tell the doctor if you are taking:
• Hormone contraceptives, e.g. pills, patches, injections or implants. Tegretol affects the way the contraceptive works in your body, and you may get breakthrough bleeding or spotting. It may also make the contraceptive less effective and there will be a risk of getting pregnant. Your doctor will be able to advise you about this, and you should think about using other contraceptives.
• Hormone Replacement Therapy (HRT). Tegretol can make HRT less effective.
• Any medicines for depression or anxiety.
• Corticosteroids (‘steroids’). You might be taking these for inflammatory conditions such as asthma, inflammatory bowel disease, muscle and joint pains.
• Anticoagulants to stop your blood clotting.
• Antibiotics to treat infections including skin infections and TB (e.g. ciprofloxacillin).
• Antifungals to treat fungal infections.
• Painkillers containing paracetamol, dextropropoxyphene, tramadol, methadone or buprenorphine.
• Other medicines to treat epilepsy.
• Medicines for high blood pressure or heart problems.
• Antihistamines (medicines to treat allergy such as hayfever, itch, etc).
• Diuretics (water tablets).
• Cimetidine or omeprazole (medicines to treat gastric ulcers).
• Isotretinoin (a medicine for the treatment of acne).
• Metoclopramide or aprepitant (anti-sickness medications).
• Acetazolamide (a medicine to treat glaucoma - increased pressure in the eye).
• Danazol or gestrinone (treatments for endometriosis).
• Theophylline or aminophylline (used in the treatment of asthma).
• Ciclosporin, tacrolimus or sirolimus (immunosuppressants, used after transplant operations, but also sometimes in the treatment of arthritis or psoriasis).
• Drugs to treat schizophrenia (e.g. paliperidone, aripiprazole).
• Cancer drugs (e.g. temsirolimus, cyclophasphamide, lapatinib).
• The anti-malarial drug, mefloquine.
• Drugs to treat HIV.
• Levothyroxine (used to treat hypothyroidism).
• Tadalafil (used to treat impotence).
• Albendazole (used to treat worms).
• Bupropion (used to help stop smoking).
• A herbal remedy called St John’s Wort or Hypericum.
• Drugs or supplements containing Vitamin B (nicotinamide).
Pregnancy and breastfeeding
You must discuss your epilepsy treatment with your doctor well before you become pregnant. If you do get pregnant you must tell the doctor straightaway. It is important that your epilepsy remains well controlled, but, as with other anti-epilepsy treatments, there is a risk of harm to the foetus. Make sure you are very clear about the risks and the benefits of being treated with Tegretol Suppositories.
Mothers being treated with Tegretol Suppositories can breastfeed their babies, but you must tell the doctor as soon as possible if you think that the baby is suffering side effects such as excessive sleepiness, skin reaction or yellow skin and eyes, dark urine or pale stools.
Will there be any problems with driving or using machinery?
Tegretol Suppositories can make you feel dizzy or drowsy, or may cause blurred vision, double vision, or you may have a lack of muscular coordination, especially at the start of treatment or when the dose is changed. If you are affected in this way, or if your eyesight is affected, you should not drive or operate machinery.
Other special warnings
• Drinking alcohol may affect you more than usual. Discuss whether you should stop drinking with your doctor.
• Eating grapefruit, or drinking grapefruit juice, may increase your chance of experiencing side effects.
• Your doctor may want you to have a number of blood tests before you are treated with Tegretol and sometimes during your treatment. This is quite usual and nothing to worry about.
3. How to use Tegretol Suppositories
The doctor will tell you the dose you need. Always follow his/her instructions carefully. The dose will be on the pharmacist’s label. Check the label carefully. It is important to use the suppositories at the right times. If you are not sure, ask your doctor or pharmacist. Keep using the suppositories for as long as you have been told, unless you have any problems. In that case, check with your doctor.
Suppositories are designed to be inserted into the back passage (rectum). Never take them by mouth.
For how to insert the suppositories see the end of the leaflet.
Your doctor will work out the dose that you need. It varies from person to person.
The maximum dose is 1,000 mg per day. Elderly people might need a lower dose.
What if you forget a dose?
If you forget to take a dose, take one as soon as you remember. If it is nearly time for your next dose, though, just take the next dose and forget about the one you missed.
Using too many suppositories
If you accidentally insert too many suppositories, or if anyone swallows any suppositories, tell your doctor or your nearest hospital casualty department. Take your pack with you so that people can see what medicine you are having.
4. Possible side effects
Tegretol Suppositories do not usually cause problems, but like all medicines, they can sometimes cause side effects.
Some side effects can be serious
Stop using the suppositories and tell your doctor straight away if you notice:
• Serious skin reactions such as rash, red skin, blistering of the lips, eyes or mouth, or skin peeling accompanied by fever. These reactions may be more frequent in patients of Chinese or Thai origin
• Mouth ulcers or unexplained bruising or bleeding
• Sore throat or high temperature, or both
• Yellowing of your skin or the whites of your eyes
• Swollen ankles, feet or lower legs
• Any signs of nervous illness or confusion
• Pain in your joints and muscles, a rash across the bridge of the nose and cheeks and problems with breathing (these may be the signs of a rare reaction known as lupus erythematosus)
• Fever, skin rash, joint pain, and abnormalities in blood and liver function tests (these may be the signs of a multi-organ sensitivity disorder)
• Bronchospasm with wheezing and coughing, difficulty in breathing, feeling faint, rash, itching or facial swelling (these may be the signs of a severe allergic reaction)
• Pain in the area near the stomach.
The side effects listed below have also been reported.
More than 1 in 10 people have experienced:
Leucopenia (a reduced number of the cells which fight infection making it easier to catch infections); dizziness and tiredness; feeling unsteady or finding it difficult to control movements; feeling or being sick; changes in liver enzyme levels (usually without any symptoms); skin reactions which may be severe.
Up to 1 in 10 people have experienced:
Changes in the blood including an increased tendency to bruise or bleed; fluid retention and swelling; weight increase; low sodium in the blood which might result in confusion; headache; double or blurred vision; dry mouth; rectal irritation.
Up to 1 in 100 people have reported:
Abnormal involuntary movements including tremor or tics; abnormal eye movements; diarrhoea; constipation.
Up to 1 in 1,000 people have reported:
Disease of the lymph glands; folic acid deficiency; a generalised allergic reaction including rash, joint pain, fever, problems with the liver, kidneys and other organs; hallucinations; depression; loss of appetite; restlessness; aggression; agitation; confusion; speech disorders; numbness or tingling in the hands and feet; muscle weakness; high blood pressure (which may make you feel dizzy, with a flushed face, headache, fatigue and nervousness); low blood pressure (the symptoms of which are feeling faint, light headed, dizzy, confused, having blurred vision); changes to heart beat; stomach pain; liver problems including jaundice; symptoms of lupus.
Up to 1 in 10,000 people have reported:
Changes to the composition of the blood including anaemia; porphyria; meningitis; swelling of the breasts and discharge of milk which may occur in both male and females; abnormal thyroid function tests; osteomalacia (which may be noticed as pain on walking and bowing of the long bones in the legs); osteoporosis; increased blood fat levels; taste disturbances; conjunctivitis; glaucoma; cataracts; hearing disorders; heart and circulatory problems including deep vein thrombosis (DVT), the symptoms of which could include tenderness, pain, swelling, warmth, skin discoloration and prominent superficial veins; lung or breathing problems; severe skin reactions including Stevens-Johnson syndrome (These reactions may be more frequent in patients of Chinese or Thai origin); sore mouth or tongue; liver failure; increased sensitivity of the skin to sunlight; alterations in skin pigmentation; acne; excessive sweating; hair loss; increased hair growth on the body and face; muscle pain or spasm; sexual difficulties which may include reduced male fertility, loss of libido or impotence; kidney failure; blood spots in the urine; increased or decreased desire to pass urine or difficulty in passing urine.
The following have also been reported, but the frequency cannot be estimated from the available information:
Severe skin reactions, accompanied by feeling unwell and changes in blood results. Diarrhoea, abdominal pain, and fever (signs of inflammation of the colon), reactivation of herpes virus infection (can be serious when immune system is depressed), complete loss of nails, fracture, decrease in the measure of the bone density, drowsiness, memory loss, purple or reddish-purple bumps that may be itchy.
Do not be alarmed by this list. Most people use Tegretol Suppositories without any problems.
If any of the symptoms become troublesome, or if you notice anything else not mentioned here, please go and see your doctor. He/she may want to give you a different medicine.
There have been reports of bone disorders including osteopenia and osteoporosis (thinning of the bone) and fractures. Check with your doctor or pharmacist if you are on long-term antiepileptic medication, have a history of osteoporosis, or take steroids.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
5. How to store Tegretol Suppositories
Protect from heat (store below 30°C).
Keep out of the reach and sight of children.
Do not use the suppositories after the expiry date which is printed on the outside of the pack.
If your doctor tells you to stop using the suppositories, please take any left over back to your pharmacist to be destroyed. Do not throw them away with your normal household water or waste. This will help to protect the environment.
6. Further information
The suppositories are white or off-white in colour and come in two strengths. The active ingredient is carbamazepine, and they also contain the inactive ingredients hydroxypropyl methylcellulose and suppository mass 15. The lower dose contains 125 mg of carbamazepine and the suppository weighs about 1 gram. The higher dose contains 250 mg of carbamazepine and the suppository weighs about 2 grams.
There are 5 suppositories in each pack.
Marketing Authorisation Holder:
Essential Pharma Ltd., 7 Egham Business Village, Crabtree Road, Egham, Surrey, TW20 8RB, United Kingdom.
Manufacturer
Novartis Pharmaceuticals UK Ltd, Wimblehurst Road, Horsham, West Sussex, RH12 5AB, England, United Kingdom and Frimley Business Park, Frimley, Camberley, Surrey, GU16 7SR, England, United Kingdom.
How to insert the suppositories
• Empty your bowels before inserting a suppository.
• Wash your hands.
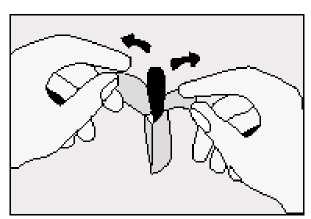
• Take out the strip of suppositories and tear off one along the perforation.
• Tear the foil wrapping apart at the notch and take out the suppository.
• Lie on one side with your knees pulled up towards your chest.
• Gently push the suppository pointed end first into your back passage (rectum) with your finger.
Push the suppository in as far as possible as shown in the diagram.
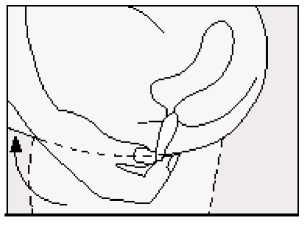
• Lower your legs and, if possible, stay still for a few minutes.
• If you feel as if you need to push the suppository out, try to resist this by lying still with your buttocks pressed together. It is important to keep the suppository in the rectum to allow it to melt and the medicine to be absorbed. Pushing the suppository high into the rectum with your finger will help to reduce this feeling.
• Wash your hands.
The procedure is the same for a child. Once they have emptied their bowels, get them to lie down on their front or side. Gently push the suppository into the child’s back passage until it disappears. Try and stop the child moving around for a few minutes to reduce the risk of the suppository coming out.
If a doctor or nurse is giving the suppository to an unconscious patient, the procedure will be similar to that described above.
This leaflet was revised in June 2016.
8/8 T eg 125-250mgSupp-PL-UK-1