Tiloket Cr 200Mg Capsules
PATIENT INFORMATION LEAFLET
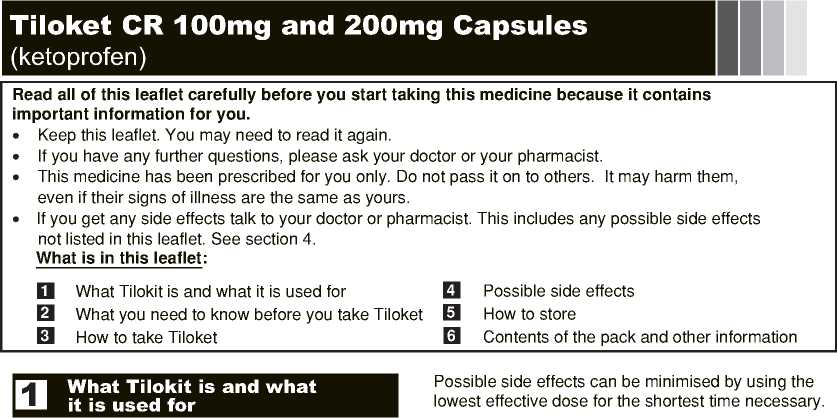
The name of this medicine is: Tiloket CR Capsules (referred to as Tiloket throughout this leaflet). It contains Ketoprofen. These capsules are controlled release capsules, which mean that the ketoprofen is released slowly into the blood. This medicine belongs to the group of medicines known as non-steroidal antiinflammatory drugs (NSAIDs). The capsules are effective against pain, inflammation and fever.
Tiloket can be used in the management of
■ rheumatoid arthritis
■ osteoarthritis
■ ankylosing spondylitis (chronic inflammatory disease of the spine and nearby joints)
■ inflammation of the moving parts of the body (joint space, capsule, lining of the joint, muscle insertion), cervical spondylitis
■ low back pain (strain, lumbago, sciatica, inflammation of the fibrous tissue)
■ painful musculoskeletal conditions
■ severe menstrual pain (dysmenorrhoea)
What you need to know before you take Tiloket
Do not take Tiloket:
■ If you are allergic to ketoprofen or any of the other ingredients of this medicine (see Section 6 "Contents of the pack and other information")
■ If you are allergic to aspirin, ibuprofen or any other non-steroidal anti-inflammatory drug (NSAIDs). Symptoms of an allergic reaction include breathing problems, swelling of the face or throat, runny nose, redness of the skin or an itchy skin rash
■ If you have or have ever had an ulcer, perforation or bleed in your stomach or intestine (gut)
■ If you have a history of stomach bleeding or perforation related to previous NSAID treatment
■ If you have severe liver, kidney or heart problems
■ If you are in the last 3 months of pregnancy (see section 2 'Pregnancy & breast-feeding')
■ If you bruise more easily than usual and have bleeding that lasts a long time
Warnings and precautions
Talk to your doctor before taking Tiloket:
■ If you have kidney or liver problems
■ If you have asthma combined with a chronic runny nose, blocked nose or swellings in the nose, as you have a higher risk of allergy to aspirin or NSAIDs
■ If you have SLE (systemic lupus erythematosis) or any other similar condition with symptoms such as joint pain, skin rash and fever. There may be an increased risk of aseptic meningitis
■ If you have a history of ulcers or you are elderly as there is an increased risk of stomach bleeding and perforation (see Section 2 below 'Please note')
■ If you have a history of suffering from a disease of the bowel or intestine, such as ulcerative colitis or Crohn's disease
■ If you are planning to become pregnant or you have problems becoming pregnant. Tiloket may make it more difficult to become pregnant (see Section 2 "Pregnancy & breast-feeding')
■ If you are taking other medicines, such as hydrocortisone (oral corticosteroids), warfarin (anticoagulants), citalopram (SSRIs), furosemide (diuretics /water tablets), aspirin or other NSAIDs including COX-2 selective NSAIDs e.g. celecoxib (see Section 2 "Other medicines and Tiloket")
■ If you have heart problems (see Section 2 below 'Please note')
■ If you have an infectious disease as this medicine may mask the usual signs of the disease becoming worse e.g. a fever
Please note:
Possible heart problems
Medicines such as Tiloket may be associated with a small increased risk of heart attack ("myocardial infarction") or stroke. Any risk is more likely with high doses and prolonged treatment. Do not exceed the recommended dose or duration of treatment.
If you have heart problems, previous stroke or think that you might be at risk of these conditions (for example if you have high blood pressure, diabetes or high cholesterol or are a smoker) you should discuss your treatment with your doctor or pharmacist.
Possible stomach problems
Some evidence suggests that ketoprofen, the active ingredient of Tiloket, may be associated with a high risk of serious stomach problems, such as bleeding, ulcers or perforation, relative to other NSAIDs. This is more likely if you take a high dose of Tiloket.
Other medicines and Tiloket:
Tell your doctor if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription. This includes herbal medicines.
Medicines which may interact with or be effected by Tiloket
■ salicylates, such as aspirin (high dosage) or other NSAIDs e.g. ibuprofen or celecoxib. You should avoid using these medicines with Tiloket (Tiloket may increase the risk of ulcers or haemorrhages)
■ selective serotonin reuptake inhibitors (SSRIs), used to treat depression e.g. citalopram, paroxetine, fluoxetine or sertraline (Tiloket may increase the risk of stomach bleeding)
■ corticosteroids, used to treat inflammation and allergic conditions e.g. hydrocortisone, betamethasone or prednisolone (Tiloket may increase the risk of stomach bleeding or ulcers)
■ anticoagulants used to stop blood clotting e.g. warfarin, heparin, ticlopidine or clopidogrel (Tiloket may increase the effects of these medicines)
■ probenecid, a medicine used to treat gout
■ methotrexate, used to treat some inflammatory diseases and cancers
■ sulphonamides, used to treat bacterial infections e.g. co-trimoxazole
■ hydantoins, used to treat seizures e.g. phenytoin
■ lithium, used to treat depression
■ ciclosporin, used to treat some inflammatory diseases and after an organ transplantation to help prevent rejection (especially if elderly)
■ pentoxifylline, used to help poor blood circulation in limbs
■ mifepristone, used to terminate a pregnancy
■ cardiac glycosides, used to treat heart failure e.g. digoxin
■ quinolone antibiotics, used to treat bacterial infections e.g. ciprofloxacin
■ medicines used to treat high blood pressure e.g. atenolol (beta-blockers) and, if you have kidney problems, medicines such as captopril (ACE inhibitors) and candesartan (angiotensin II antagonists)
■ water tablets (diuretics) e.g. amiloride
■ medicines used to treat diabetes e.g. gliclazide
■ tacrolimus, used to dampen down the body's immune response and may be used for severe skin complaints and following organ transplantation
■ zidovudine, used to treat viral infections
■ aminoglycosides used to treat bacterial infections e.g. amikacin
■ thrombolytics used to dissolve blood clots such as streptokinase, alteplase or reteplase
Pregnancy and breast-feeding:
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
Pregnancy
You should not take this medicine if you trying to become pregnant, unless told to do so by your doctor. This medicine may make it more difficult to become pregnant.
Tiloket should not be taken during the first and second trimester (first 6 months) of pregnancy or whilst trying to conceive, unless your doctor tells you to. If Tiloket is used, the dose should be low and the length of treatment as short as possible.
Tiloket must not be used during the last three months of pregnancy.
Breast-feeding
If you are breast-feeding, you should not take this medicine, unless told to do so by your doctor.
Driving and using machines:
Tiloket may affect your ability to drive and operate machinery by causing headaches, fatigue, nausea, confusion, blurred vision, dizziness, drowsiness. You may have a fit (convulsion) while taking this medicine.
If you do experience any effects, do not drive or operate machinery.
Tiloket contains micrograins of sugar and sulfar dioxide
These capsules contains micrograins of sugar. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine.
These capsules contains sulphur dioxide, which on rare occasions, may cause severe allergic reactions and difficulty in breathing or wheezing.
continued..
3]
How to take Tiloket
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
■ These capsules are to be taken orally
■ You should take the capsules twice daily with food
■ Swallow the capsule(s) whole with a glass of water The recommended dose is:
The doses stated below are guidelines only. Your doctor will decide on the correct dosage for your condition and symptoms.
Adults:
The usual dose is 100 - 200mg daily, depending on the patient's weight and the severity of the symptoms.
The maximum daily dose is 200mg and this must not be exceeded
Older people:
Your doctor will prescribe the lowest effective dose for you to take. Your doctor may need to monitor you regularly for any bleeding from your stomach during the first four weeks after you start your treatment and may need to carry out blood tests from time to time.
Use in children:
Tiloket is not recommended for children.
If you take more Tiloket than you should
If you accidently take too many capsules, contact your doctor, pharmacist or nearest emergency department immediately for advice. Remember to take the carton and any remaining capsules with you.
The symptoms of an overdose include: lack of energy, feeling or being sick, stomach pain, bleeding in the stomach, diarrhoea (rare), feeling disorientated or excited, coma, drowsiness, dizziness, ringing in your ears, fainting and, occasionally, low blood pressure, difficulty breathing or fits.
If you forget to take Tiloket
If you forget to take a dose, take it as soon as you remember, unless it is almost time for your next dose. Do not take a double dose to make up for a forgotten dose.
If you stop taking Tiloket
Do not stop or change your treatment before talking to your doctor. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Stop taking Tiloket and seek medical advice immediately if you develop the following symptoms
■ Pass blood in your stools or black, tarry stools, vomit any blood or dark particles that look like coffee grounds (possible symptoms of stomach bleeding)
■ Indigestion or heartburn, severe abdominal or stomach pain or other abnormal stomach symptoms (possible symptoms of a peptic ulcer or stomach perforation)
■ Allergic reactions: swelling of the hands, face, feet, eyelids, lips, tongue, throat, difficulty breathing, itching, dizziness (anaphylactic reaction)
■ Blistering of the skin (Toxic Epidermal Necrolysis), mouth, eyes or genitals (Stevens-Johnson Syndrome)
■ Swelling of the face or throat (angiodema)
■ Eye problems, such as blurred vision
■ Lack of energy, shortness of breath or weakness (symptoms of kidney failure) or blood in your urine, a change in the amount of urine you produce, swelling, especially of your legs, ankles or feet (symptoms of serious kidney problems)
Common side effects (may affect up to 1 in 10
people)
■ indigestion
■ feeling or being sick
■ stomach pain
Uncommon side effects (may affect up to 1 in 100
people) headache dizziness
tiredness or drowsiness constipation diarrhoea wind (flatulence)
pain or discomfort in the upper abdomen (gastritis) itching with or without a rash (pruritus) swelling of parts of the body (oedema)
Rare side effects (may affect up to 1 in 10,000 people)
pale skin, weakness or breathlessness due to a loss of blood (haemorrhagic anaemia) tingling or numbness in the hands or feet (paraesthesia) ringing in the ears (tinnitus) coughing, wheezing, shortness of breath or tightness of the chest (asthma) inflammation of the mucous lining of the mouth (stomatitis)
tiredness, pains in abdomen, muscle and joint aches , yellowing of skin and eyes (inflammation of the liver [jaundice] hepatitis) increase in liver enzymes or bilirubin (detected through blood tests) increased weight
Not known: frequency cannot be estimated from the available data
■ abnormally low level or decrease of white blood cells in the blood &/or make infections more likely (neutropenia/agranulocytosis)
■ reduction in blood platelets, which increases the risk
of bleeding or bruising (thrombocytopenia) tiredness, prone to infections or easily bruised due to bone marrow failure
severe reduction in blood cells which can cause weakness, bruising or make infections more likely (aplastic anaemia)
reduction in red blood cells which can make the skin pale yellow and cause weakness or breathlessness (haemolytic anaemia) mood change fits
abnormal sense of taste (dysgeusia) visual disturbances
painful inflammation of the optic nerve in your eye (optic neuritis)
shortness of breath or ankle swelling (heart failure) high blood pressure reddening of the face (vasodilatation) worsening of asthma or bronchospasm i.e. coughing, wheezing, shortness of breath or tightness of the chest runny nose (rhinitis)
worsening of abdominal pain or diarrhoea (symptoms of colitis) or diarrhoea and weight loss (symptoms of crohn's disease) increased sensitivity of the skin to sunlight (photosensitivity) loss of hair (alopecia)
skin rash resulting from bleeding into the skin (purpura)
red patches on the skin (erythema multiforme) or scaling of the skin (exfoliative dermatitis) itchy rash
kidney problems or worsening of existing kidney problems
swollen ankles or high blood pressure due to inflammation of the kidney abnormal kidney function tests feeling generally unwell
Medicines such as ketoprofen may be associated with a small increased risk of heart attack ("myocardial infarction") or stroke. Any risk is more likely with high doses and prolonged treatment. Do not exceed the recommended dose or duration of treatment."
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the internet at
www.mhra.gov.uk/yellowcard. By reporting side effects you can help provide more information on the safety of this medicine.
How to Store
Keep this medicine out of the sight and reach of children.
Do not store above 25°C.
Keep the capsules in the original container.
Do not use this medicine after the expiry date which is stated on the carton/blister after "EXP". The expiry date refers to the last day of that month.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer required. These measures will help to protect the environment.
Contents of the pack and further information
What Tiloket contains:
Each Tiloket CR 100mg capsule contains 100mg of ketoprofen
Each Tiloket CR 200mg capsule contains 200mg of ketoprofen
The other ingredients are: povidone, ethylcellulose, talc and micrograins of sugar and starch.
The 100mg capsule shell contains gelatin, sulfur dioxide, titanium dioxide, denatured ethanol and black ink code 1007.
The 200mg capsule shell contains gelatin, sulfur dioxide, titanium dioxide, the colourings E104 (quinoline yellow), E127 (erythrosine BS), E132 (indigo carmine), E172 (yellow iron oxide) and E171 (titanium dioxide) and opacode white (shellac, soya lecithin, IMS and ethoxy ethanol).
What Tiloket looks like and contents of the pack:
Tiloket CR 100mg capsules: white cap, colourless body, size 3 capsules, containing homogeneous creamy white microgranules,printed TILOKET 100mg CR
Tiloket CR 200mg capsules: red cap, transparent green body, size 1 capsules, containing homogeneous creamy white microgranules, printed TILOKET 200mg CR
Tiloket is available in:
Tiloket CR 100mg Capsules are available in packs of 56 capsules.
Tiloket CR 200mg Capsules are available in packs of 28 capsules.
Marketing Authorisation Holder and Manufacturer:
Tillomed Laboratories Ltd.
3 Howard Road, Eaton Socon, St. Neots, Cambridgeshire, PE19 8ET,
United Kingdom.
Product Licence Number:
Tiloket CR 100mg Capsules: PL 11311/0103 Tiloket CR 200mg Capsules: PL 11311/0104
Date of last revision: April 2014
Hard to Read? Phone 0800 970 6115 for help
Till-Ver.4s