Voriconazole Teva 200 Mg Powder For Solution For Infusion
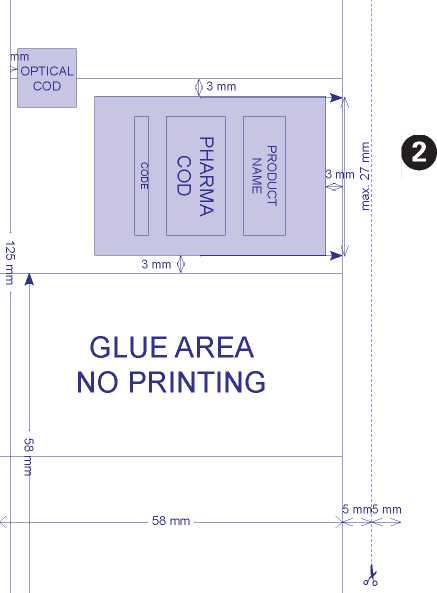
PHARMA
COD
GLUEAREA NO PRINTING
3 mm
OPTICAL ~i COD
v v
HOSPITALS
PACKAGE LEAFLET: INFORMATION FOR THE USER
VORICONAZOLE 200 mg POWDER FOR SOLUTION FOR INFUSION
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor, pharmacist or nurse.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
WHAT IS IN THIS LEAFLET:
1. What Voriconazole is and what it is used for
2. What you need to know before you use Voriconazole
3. How to use Voriconazole
4. Possible side effects
5. How to store Voriconazole
6. Contents of the pack and other information
*1 What Voriconazole is and what it is used for
Voriconazole contains the active substance voriconazole. Voriconazole is an antifungal medicine. It works by killing or stopping the growth of the fungi that cause infections.
It is used for the treatment of patients (adults and children over the age of 2) with:
• invasive aspergillosis (a type of fungal infection due to Aspergillus sp)
• candidaemia (another type of fungal infection due to Candida sp.) in non-neutropenic patients (patients without abnormally low white blood cells count)
• serious invasive Candida sp. infections when the fungus is resistant to fluconazole (another antifungal medicine)
• serious fungal infections caused by Scedosporium sp. or Fusarium sp. (two different species of fungi).
Voriconazole is intended for patients with worsening, possibly life-threatening, fungal infections.
• Prevention of fungal infections in high risk bone marrow transplant recipients.
This product should only be used under the supervision of a doctor.
What you need to know before you use Voriconazole
Do not use Voriconazole:
• If you are allergic to voriconazole or any of the other ingredients of this medicine (listed in section 6)
• If your kidney function is seriously reduced.
It is very important that you inform your doctor, pharmacist or nurse if you are taking or have taken any other medicines, even those that are obtained without a prescription, or herbal medicines.
Do not take the following medicines during your course of treatment with Voriconazole:
• Terfenadine (used for allergy)
• Astemizole (used for allergy)
• Cisapride (used for stomach problems)
• Pimozide (used for treating mental illness)
• Quinidine (used for irregular heart beat)
• Rifampicin (used for treating tuberculosis)
• Efavirenz (used for treating HIV) in doses of 400 mg and above once daily
• Carbamazepine (used to treat seizures)
• Phenobarbital (used for severe insomnia and seizures)
• Ergot alkaloids (e.g. ergotamine, dihydroergotamine; used for migraine)
-575 mm -
• Sirolimus (used in transplant patients)
• Ritonavir (used for treating HIV) in doses of 400 mg and more twice daily
• St John's Wort (herbal supplement).
Warnings and precautions
Talk to your doctor, pharmacist or nurse before using Voriconazole if you:
• have had an allergic reaction to other azoles
• are suffering from, or have ever suffered from liver disease. If you have liver disease, your doctor may prescribe a lower dose of Voriconazole. Your doctor should also monitor your liver function while you are being treated with Voriconazole by doing blood tests
• are known to have cardiomyopathy, irregular heart beat, slow heart rate or an abnormality of electrocardiogram (ECG) called ‘long QTc syndrome'.
You should avoid any sunlight and sun exposure while being treated. It is important to
cover sun exposed areas of skin and use sunscreen with high sun protection factor (SPF),
as an increased sensitivity of skin to the sun's UV rays can occur. These precautions are
also applicable to children.
Tell your doctor immediately if you develop the following symptoms while being treated with Voriconazole:
• sunburn
• severe skin rash or blisters
• bone pain.
If you develop skin disorders as described above, your doctor may refer you to a dermatologist, who after consultation may decide that it is important for you to be seen on a regular basis. There is a small chance that skin cancer could develop with long term use of Voriconazole.
Your doctor should monitor the function of your liver and kidney by doing blood tests. Children and adolescents
Voriconazole should not be given to children younger than 2 years of age.
Other medicines and Voriconazole
Tell your doctor or pharmacist if you are taking/using, have recently taken/used or might take/use any other medicines.
Some medicines, when taken at the same time as Voriconazole, may affect the way Voriconazole works or Voriconazole may affect the way they work.
Tell your doctor if you are taking the following medicine, as treatment with Voriconazole at the same time should be avoided if possible:
• Ritonavir (used for treating HIV) in doses of 100 mg twice daily.
Tell your doctor if you are taking either of the following medicines, as treatment with Voriconazole at the same time should be avoided if possible, and a dose adjustment of voriconazole may be required:
• Rifabutin (used for treating tuberculosis). If you are already being treated with rifabutin your blood counts and side effects to rifabutin will need to be monitored
• Phenytoin (used to treat epilepsy). If you are already being treated with phenytoin your blood concentration of phenytoin will need to be monitored during your treatment with Voriconazole and your dose may be adjusted.
Tell your doctor if you are taking any of the following medicines, as a dose adjustment or monitoring may be required to check that the medicines and/or Voriconazole are still having the desired effect:
• Warfarin and other anticoagulants (e.g. phenprocoumon, acenocoumarol; used to slow down clotting of the blood)
• Ciclosporin (used in transplant patients)
• Tacrolimus (used in transplant patients)
• Sulphonylureas (e.g. tolbutamide, glipizide, and glyburide) (used for diabetes)
• Statins (e.g. atorvastatin, simvastatin) (used for lowering cholesterol)
• Benzodiazepines (e.g. midazolam, triazolam) (used for severe insomnia and stress)
• Omeprazole (used for treating ulcers)
• Oral contraceptives (if you use Voriconazole whilst using oral contraceptives, you may get side effects such as nausea and menstrual disorders)
• Vinca alkaloids (e.g. vincristine and vinblastine) (used in treating cancer)
• Indinavir and other HIV protease inhibitors (used for treating HIV)
• Non-nucleoside reverse transcriptase inhibitors (e.g. efavirenz, delavirdine, nevirapine) (used for treating HIV) (some doses of efavirenz can NOT be taken at the same time as Voriconazole)
• Methadone (used to treat heroin addiction)
• Alfentanil and fentanyl and other short acting opiates such as sufentanil (painkillers used for surgical procedures)
• Oxycodone and other long acting opiates such as hydrocodone (used for moderate to severe pain)
• Non-steroidal anti-inflammatory drugs (e.g. ibuprofen, diclofenac) (used for treating pain and inflammation)
• Fluconazole (used for fungal infections)
• Everolimus (used for treating advanced kidney cancer and in transplant patients). Pregnancy and breast-feeding
Voriconazole must not be used during pregnancy, unless indicated by your doctor. Effective contraception must be used in women of childbearing potential. Contact your doctor immediately if you become pregnant while being treated with Voriconazole.
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Driving and using machines
Voriconazole may cause blurring of vision or uncomfortable sensitivity to light. While affected, do not drive or operate any tools or machines. Tell your doctor if you experience this.
How to use Voriconazole
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
Your doctor will determine your dose depending on your weight and the type of infection you have.
Your doctor may change your dose depending on your condition.
The recommended dose for adults (including elderly patients) is as follows:
|
Intravenous | |
|
Dose for the first 24 hours (Loading Dose) |
6 mg/kg every 12 hours for the first 24 hours |
|
Dose after the first 24 hours (Maintenance Dose) |
4 mg/kg twice a day |
Depending on your response to treatment, your doctor may decrease the dose to 3 mg/kg twice daily.
The doctor may decide to decrease the dose if you have mild to moderate cirrhosis.
Use in children and adolescents
The recommended dose for children and teenagers is as follows:
|
Intravenous | ||
|
Children aged 2 to less than 12 years and teenagers aged 12 to 14 years weighing less than 50 kg |
Teenagers aged 12 to 14 years weighing 50 kg or more; and all teenagers older than 14 | |
|
Dose for the first 24 hours (Loading Dose) |
9 mg/kg every 12 hours for the first 24 hours |
6 mg/kg every 12 hours for the first 24 hours |
|
Dose after the first 24 hours (Maintenance Dose) |
8 mg/kg twice a day |
4 mg/kg twice a day |
Depending on your response to treatment, your doctor may increase or decrease the daily dose.
A
The following information is intended for medical or healthcare professionals only:
Reconstitution and Dilution information
• Voriconazole needs to first be reconstituted with either 19 ml of Water for Injections or 19 ml of 9 mg/ml (0.9%) Sodium Chloride for Infusion to obtain an extractable volume of 20 ml of clear concentrate containing 10 mg/ml voriconazole
• Discard the Voriconazole vial if the vacuum does not pull the diluent into the vial
• It is recommended that a standard 20 ml (non-automated) syringe be used to ensure that the exact amount (19.0 ml) of Water for Injections or of 9 mg/ml (0.9%) Sodium Chloride for Infusion is dispensed
• The required volume of the reconstituted concentrate is then added to a recommended compatible infusion solution listed below to obtain a final Voriconazole solution containing 0.5 to 5 mg/ml of voriconazole
• This medicinal product is for single use only and any unused solution should be discarded and only clear solutions without particles should be used
• Not for administration as a bolus injection
• For storage information, please refer to Section 5 ‘How to store Voriconazole'.
Required Volumes of 10 mg/ml Voriconazole Concentrate
|
Body Weight (kg) |
Volume of Voriconazole Concentrate (10 mg/ml) required for: | ||||
|
3 mg/kg dose (number of vials) |
4 mg/kg dose (number of vials) |
6 mg/kg dose (number of vials) |
8 mg/kg dose (number of vials) |
9 mg/kg dose (number of vials) | |
|
10 |
- |
4.0 ml (1) |
- |
8.0 ml (1) |
9.0 ml (1) |
|
15 |
- |
6.0 ml (1) |
- |
12.0 ml (1) |
13.5 ml (1) |
|
20 |
- |
8.0 ml (1) |
- |
16.0 ml (1) |
18.0 ml (1) |
|
25 |
- |
10.0 ml (1) |
- |
20.0 ml (1) |
22.5 ml (2) |
|
30 |
9.0 ml (1) |
12.0 ml (1) |
18.0 ml (1) |
24.0 ml (2) |
27.0 ml (2) |
|
35 |
10.5 ml (1) |
14.0 ml (1) |
21.0 ml (2) |
28.0 ml (2) |
31.5 ml (2) |
|
40 |
12.0 ml (1) |
16.0 ml (1) |
24.0 ml (2) |
32.0 ml (2) |
36.0 ml (2) |
|
45 |
13.5 ml (1) |
18.0 ml (1) |
27.0 ml (2) |
36.0 ml (2) |
40.5 ml (3) |
|
50 |
15.0 ml (1) |
20.0 ml (1) |
30.0 ml (2) |
40.0 ml (2) |
45.0 ml (3) |
|
55 |
16.5 ml (1) |
22.0 ml (2) |
33.0 ml (2) |
44.0 ml (3) |
49.5 ml (3) |
|
60 |
18.0 ml (1) |
24.0 ml (2) |
36.0 ml (2) |
48.0 ml (3) |
54.0 ml (3) |
|
65 |
19.5 ml (1) |
26.0 ml (2) |
39.0 ml (2) |
52.0 ml (3) |
58.5 ml (3) |
|
70 |
21.0 ml (2) |
28.0 ml (2) |
42.0 ml (3) |
- |
- |
|
75 |
22.5 ml (2) |
30.0 ml (2) |
45.0 ml (3) |
- |
- |
|
80 |
24.0 ml (2) |
32.0 ml (2) |
48.0 ml (3) |
- |
- |
|
85 |
25.5 ml (2) |
34.0 ml (2) |
51.0 ml (3) |
- |
- |
|
90 |
27.0 ml (2) |
36.0 ml (2) |
54.0 ml (3) |
- |
- |
|
95 |
28.5 ml (2) |
38.0 ml (2) |
57.0 ml (3) |
- |
- |
|
100 |
30.0 ml (2) |
40.0 ml (2) |
60.0 ml (3) |
- |
- |
Voriconazole is a single dose unpreserved sterile lyophile. Therefore, from a microbiological point of view, the reconstituted solution must be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and would normally not be longer than 24 hours at 2 to 8°C, unless reconstitution has taken place in controlled and validated aseptic conditions.
V
Compatible Infusion Solutions:
The reconstituted solution can be diluted with:
Sodium Chloride 9 mg/ml (0.9%) Solution for Injection Compound Sodium Lactate Intravenous Infusion 5 % Glucose and Lactated Ringer's Intravenous Infusion 5 % Glucose and 0.45 % Sodium Chloride Intravenous Infusion 5 % Glucose Intravenous Infusion
5 % Glucose in 20 mEq Potassium Chloride Intravenous Infusion 0.45 % Sodium Chloride Intravenous Infusion 5 % Glucose and 0.9 % Sodium Chloride Intravenous Infusion
The compatibility of Voriconazole with diluents other than listed above (or listed below under ‘Incompatibilities') is unknown.
Incompatibilities:
Voriconazole must not be infused into the same line or cannula concomitantly with other drug infusions, including parenteral nutrition (e.g. Aminofusin 10 % Plus).
Infusions of blood products must not occur simultaneously with Voriconazole.
Infusion of total parenteral nutrition can occur simultaneously with Voriconazole but not in the same line or cannula.
3 Voriconazole must not be diluted with 4.2 % Sodium Bicarbonate Infusion.
245 mm
40029-A . 575 x 245
Voriconazole will be reconstituted and diluted to the correct concentration by your hospital pharmacist or nurse. (Please refer to section 5 and the end of this leaflet for further information).
This will be given to you by intravenous infusion (into a vein) at a maximum rate of 3 mg/kg per hour over 1 to 3 hours.
If you or your child is using Voriconazole for prevention of fungal infections, your doctor may stop giving Voriconazole if you or your child develops treatment related side effects.
If a dose of Voriconazole has been forgotten:
As you will be given this medicine under close medical supervision, it is unlikely that a dose would be missed. However tell your doctor, pharmacist or nurse if you think that a dose has been forgotten.
If you stop using Voriconazole:
Voriconazole treatment will continue for as long as your doctor advises, however duration of treatment with Voriconazole should be no more than 6 months.
Patients with a weakened immune system or those with difficult infections may require long-term treatment to prevent the infection from returning. You may be switched from the intravenous infusion to tablets once your condition improves.
When Voriconazole treatment is stopped by your doctor you should not experience any effects.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
^ Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If any side effects occur, most are likely to be minor and temporary. However, some may be serious and need medical attention.
Serious side effects - Stop using Voriconazole and see a doctor immediately
• Rash
• Jaundice; Changes in blood tests of liver function
• Pancreatitis.
Other side effects
Very common side effects (may affect more than 1 in 10 people) are:
• Visual impairment (change in vision)
• Fever
• Rash
• Nausea, vomiting, diarrhoea
• Headache
• Swelling of the extremities
• Stomach pains
• Breathing difficulties.
Common side effects (may affect up to 1 in 10 people) are:
• Flu-like symptoms, irritation and inflammation of the gastrointestinal tract, inflammation of the sinuses, inflammation of the gums, chills, weakness
• Low numbers of some types of red or white blood cells, low numbers of cells called platelets that help the blood to clot
• Allergic reaction or exaggerated immune response
• Low blood sugar, low blood potassium, low sodium in the blood
• Anxiety, depression, confusion, agitation, inability to sleep, hallucinations
• Seizures, tremors or uncontrolled muscle movements, tingling or abnormal skin sensations, increase in muscle tone, sleepiness, dizziness
• Bleeding in the eye
• Heart rhythm problems including very fast heartbeat, very slow heartbeat, fainting
• Low blood pressure, inflammation of a vein (which may be associated with the formation of a blood clot)
• Breathing difficulty, chest pain, swelling of the face, fluid accumulation in the lungs
• Constipation, indigestion, inflammation of the lips
Jaundice, inflammation of the liver, redness of the skin
Skin rashes which may lead to severe blistering and peeling of the skin characterized by
a flat, red area on the skin that is covered with small confluent bumps
Itchiness
Hair loss
Back pain
Kidney failure, blood in the urine, changes in kidney function tests.
Uncommon side effects (may affect up to 1 in 100 people) are:
• Inflammation of the gastrointestinal tract causing antibiotic associated diarrhoea, inflammation of the lymphatic vessels
• Inflammation of the thin tissue that lines the inner wall of the abdomen and covers the abdominal organ
• Enlarged lymph glands (sometimes painful), disorder of blood clotting system, failure of bone marrow, other blood cell changes (increased eosinophil and low white blood cells in blood)
• Depressed function of the adrenal gland, underactive thyroid gland
• Abnormal brain function, Parkinson-like symptoms, nerve injury resulting in numbness, pain, tingling or burning in the hands or feet
• Problems with balance or coordination
• Swelling of the brain
• Double vision, serious conditions of the eye including: pain and inflammation of the eyes and eyelids, involuntary movement of the eye, abnormal eye movement, damage to the optic nerve resulting in vision impairment, optic disc swelling
• Decreased sensitivity to touch
• Abnormal sense of taste
• Hearing difficulties, ringing in the ears, vertigo
• Inflammation of certain internal organs - pancreas and duodenum, swelling and inflammation of the tongue
• Enlarged liver, liver failure, gallbladder disease, gallstones
• Joint inflammation, inflammation of the veins under the skin (which may be associated with the formation of a blood clot)
• Inflammation of the kidney, proteins in the urine
• Very fast heart rate or skipped heartbeats
• Abnormal electrocardiogram (ECG)
• Blood cholesterol increased, blood urea increased
• Allergic skin reactions (sometimes severe), including widespread blistering rash and skin peeling, inflammation of the skin, the rapid swelling (edema) of the dermis, subcutaneous tissue, mucosa and submucosal tissues, itchy or sore patches of thick, red skin with silvery scales of skin, hives, sunburn or severe skin reaction following exposure to light or sun, skin redness and irritation, red or purple discolouration of the skin which may be caused by low platelet count, eczema
• Injection site reaction
• Life-threatening allergic reaction.
Rare side effects (may affect up to 1 in 1000 people) are:
• Overactive thyroid gland
• Deterioration of brain function that is a serious complication of liver disease
• Damage to the optic nerve resulting in vision impairment, clouding of the cornea
• Bullous photosensitivity
• A disorder in which the body's immune system attacks part of the peripheral nervous system
• Severe heart rhythm problems that may be life-threatening.
Other significant side effects whose frequency is not known, but should be reported to your doctor immediately:
• Skin cancer
• Inflammation of the tissue surrounding the bone
• Red, scaly patches or ring-shaped skin lesions that may be a symptom of an autoimmune disease called cutaneous lupus erythematosus.
Reactions during the infusion have occurred uncommonly with Voriconazole (including flushing, fever, sweating, increased heart rate and shortness of breath). Your doctor may stop the infusion if this occurs.
As Voriconazole has been known to affect the liver and the kidney, your doctor should monitor the function of your liver and kidney by doing blood tests. Please advise your doctor if you have any stomach pains or if your stools have a different consistency.
There have been reports of skin cancer in patients treated with Voriconazole for long periods of time.
Sunburn or severe skin reaction following exposure to light or sun was experienced more frequently in children. If you or your child develops skin disorders, your doctor may refer you to a dermatologist, who after consultation may decide that it is important for you or your child to be seen on a regular basis.
If any of these side effects persist or are troublesome, please tell your doctor.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard
By reporting side effects you can help provide more information on the safety of this medicine.
How to store Voriconazole
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the label or carton after EXP. The expiry date refers to the last day of that month.
Do not store above 30°C.
Once reconstituted, Voriconazole should be used immediately, but if necessary may be stored for up to 24 hours at 2°C - 8°C (in a refrigerator). Reconstituted Voriconazole needs to be diluted with a compatible infusion solution first before it is infused. (Please refer to the end of this leaflet for further information).
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
Contents of the pack and other information
What Voriconazole contains
The active substance is voriconazole.
The other ingredients are hydroxypropylbetadex and hydrochloric acid (for pH adjustment).
Each vial contains 200 mg voriconazole, equivalent to a 10 mg/ml solution when reconstituted as directed by your hospital pharmacist or nurse (see the information at the end of this leaflet).
What Voriconazole looks like and contents of the pack
Voriconazole is presented in one single use glass vial as a powder for solution for infusion.
Marketing Authorisation Holder
TEVA UK Limited, Eastbourne, BN22 9AG, UK
Manufacturer
PLIVA Hrvatska d.o.o. (PLIVA Croatia Ltd.), Prilaz baruna Filipovica 25, Zagreb, 10000, Croatia
This leaflet was last revised in 01/2015.
PL 00289/1872
5 mm5 mm
< >
40029-A 575 x 245
PHARMA
COD
58 mm
O p
"0 <= 33 m
z > H 33

i.