Yanimo Respimat 2.5 Microgram / 2.5 Microgram Inhalation Solution
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
Yanimo Respimat 2.5 microgram/2.5 microgram, inhalation solution
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
The delivered dose is 2.5 microgram tiotropium (as bromide monohydrate) and 2.5 microgram olodaterol (as hydrochloride) per puff.
The delivered dose is the dose which is available for the patient after passing the mouthpiece.
For the full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Inhalation solution
Clear, colourless, inhalation solution
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Yanimo Respimat is indicated as a maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD).
4.2 Posology and method of administration
Posology
The medicinal product is intended for inhalation use only. The cartridge can only be inserted and used in the Respimat inhaler.
Two puffs from the Respimat inhaler comprise one medicinal dose.
Adults
The recommended dose is 5 microgram tiotropium and 5 microgram olodaterol given as two puffs from the Respimat inhaler once daily, at the same time of the day.
The recommended dose should not be exceeded.
Elderly population
Elderly patients can use Yanimo Respimat at the recommended dose.
Hepatic impairment and Renal impairment
Yanimo Respimat contains tiotropium which is a predominantly renally excreted drug and olodaterol, which is predominantly metabolized in the liver.
Hepatic impairment
Patients with mild and moderate hepatic impairment can use Yanimo Respimat at the recommended dose.
There are no data available for use of olodaterol in patients with severe hepatic impairment.
Renal impairment
Renally impaired patients can use Yanimo Respimat at the recommended dose.
For patients with moderate to severe impairment (creatinine clearance < 50 ml/min) see 4.4 and 5.2.
Yanimo Respimat contains olodaterol. There is limited experience with the use of olodaterol in patients with severe renal impairment.
Paediatric population
There is no relevant use of Yanimo Respimat in the paediatric population (under 18 years).
Method of administration
To ensure proper administration of the medicinal product, the patient should be shown how to use the inhaler by a physician or other health care professionals.
Instructions For Use Introduction
Yanimo Respimat (tiotropium bromide and olodaterol). Read these Instructions for Use before you start using Yanimo Respimat.
You will need to use this inhaler only ONCE A DAY. Each time you use it take TWO PUFFS.
CAP
MOUTHPIECE AIR VENT
DOSE-
RELEASE
BUTTON
SAFETY CATCH
CLEAR EASE PIERCING ELEMENT

CARTRIDGE
• If Yanimo Respimat has not been used for more than 7 days release one puff
towards the ground.
• If Yanimo Respimat has not been used for more than 21 days repeat steps 4 to 6 under ‘Prepare for first use’ until a cloud is visible. Then repeat steps 4 to 6 three more times.
• Do not touch the piercing element inside the clear base.
How to care for your Yanimo Respimat
Clean the mouthpiece including the metal part inside the mouthpiece with a damp cloth or tissue only, at least once a week.
Any minor discoloration in the mouthpiece does not affect your Yanimo Respimat inhaler performance.
If necessary, wipe the outside of your Yanimo Respimat inhaler with a damp cloth.
When to get a new Yanimo Respimat
• Your Yanimo Respimat inhaler contains 60 puffs (30 doses) if used as indicated (two puffs/once daily).
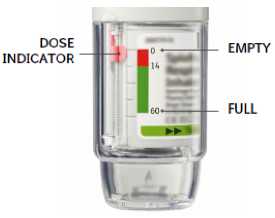
• The dose indicator shows approximately how much medication is left.
• When the dose indicator enters the red area of the scale you need to get a new prescription; there is approximately medication for 7 days left (14 puffs).
• Once the dose indicator reaches the end of the red scale, your Yanimo Respimat locks automatically - no more doses can be released. At this point, the clear base cannot be turned any further.
• Yanimo Respimat should be discarded three months after you have prepared it for first use, even if it has not been fully used or used at all.
Prepare for first use
1. Remove clear base
• Keep the cap closed.
• Press the safety catch while firmly pulling off the clear base with your other hand.
SAFETY CATCH CLEAR BASE

2. Insert cartridge
Insert the narrow end of the cartridge into the inhaler. Place the inhaler on a firm surface and push down firmly until it clicks into place.
Do not remove the cartridge once it has been inserted into the inhaler.

3. Replace clear base
• Put the clear base back into place until it clicks.
• Do not remove the clear base again.
4. Turn
• Keep the cap closed.
• Turn the clear base in the direction of the arrows on the label until it clicks (half a turn).

6. Press
• Point the inhaler toward the
ground.
• Press the dose-release
button.
• Close the cap.
• Repeat steps 4-6 until a cloud is visible.
• After a cloud is visible,
repeat steps 4-6 three more times.
Your inhaler is now ready to use. These steps will not

|
affect the number of doses | |
|
available. | |
|
After preparation your inhaler | |
|
will be able to deliver 60 | |
|
puffs (30 doses). |
Daily use
TURN
• Keep the cap closed.
• TURN the clear base in the direction of the arrows on the label until it clicks (half a turn).

OPEN
• OPEN the cap until it snaps fully open.

PRESS
• Breathe out slowly and fully.
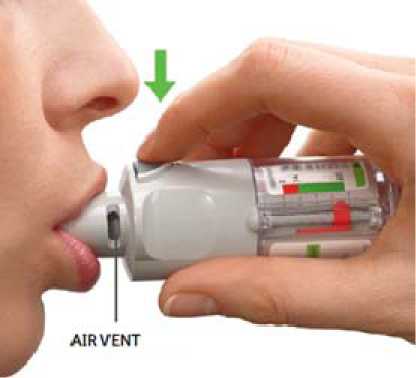
• Close your lips around the mouthpiece without covering the air vents. Point your Inhaler to the back of your throat.
• While taking a slow, deep breath through your mouth, PRESS the dose-release button and continue to breathe in slowly for as long as comfortable.
• Hold your breath for 10 seconds or for as long as comfortable.
• Repeat TURN, OPEN, PRESS for a total of 2 puffs.
• Close the cap until you use your
_inhaler again._
4.3 Contraindications
Hypersensitivity to the active substances or to any of the excipients listed in section 6.1.
History of hypersensitivity to atropine or its derivatives, e.g. ipratropium or oxitropium.
4.4 Special warnings and precautions for use
Asthma
Yanimo Respimat should not be used in asthma. The efficacy and safety of Yanimo Respimat in asthma have not been studied.
Not for acute use
Yanimo Respimat is not indicated for the treatment of acute episodes of bronchospasm, i.e. as rescue therapy.
Paradoxical bronchospasm
As with other inhaled medicines Yanimo Respimat may result in paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs Yanimo Respimat should be discontinued immediately and alternative therapy substituted.
Anticholinergic effects related to tiotropium
Narrow-angle glaucoma, prostatic hyperplasia or bladder-neck obstruction
Consistent with the anticholinergic activity of tiotropium, Yanimo Respimat should be used with caution in patients with narrow-angle glaucoma, prostatic hyperplasia or bladder-neck obstruction.
Eye symptoms
Patients should be cautioned to avoid getting the spray into their eyes. They should be advised that this may result in precipitation or worsening of narrow-angle glaucoma, eye pain or discomfort, temporary blurring of vision, visual halos or coloured images in association with red eyes from conjunctival congestion and corneal oedema.
Should any combination of these eye symptoms develop, patients should stop using Yanimo Respimat and consult a specialist immediately.
Dental caries
Dry mouth, which has been observed with anti-cholinergic treatment, may in the long term be associated with dental caries.
Patients with renal impairment
As plasma concentration of tiotropium increases with decreased renal function in patients with moderate to severe renal impairment (creatinine clearance < 50 ml/min) Yanimo Respimat should be used only if the expected benefit outweighs the potential risk. There is no long term experience in patients with severe renal impairment (see 5.2).
Cardiovascular effects
The experience with Yanimo Respimat is limited in patients with a history of myocardial infarction during the previous year, unstable or life-threatening cardiac arrhythmia, hospitalized for heart failure during the previous year or with a diagnosis of paroxysmal tachycardia (>100 beats per minute) because these patients were excluded from the clinical trials. Yanimo Respimat should be used with caution in these patient groups.
Like other beta2-adrenergic agonists, olodaterol may produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, blood pressure, and/or symptoms. In case such effects occur, treatment may need to be discontinued. In addition, beta-adrenergic agonists have been reported to produce electrocardiogram (ECG) changes, such as flattening of the T wave and ST segment depression, although the clinical significance of these observations is unknown.
Long acting beta2-adrenergic agonists should be administered with caution in patients with cardiovascular disorders, especially ischaemic heart disease, severe cardiac decompensation, cardiac arrhythmias, hypertrophic obstructive cardiomyopathy, hypertension, and aneurysm, in patients with convulsive disorders or thyrotoxicosis, in patients with known or suspected prolongation of the QT interval (e.g. QT> 0.44 s), and in patients who are unusually responsive to sympathomimetic amines.
Hypokalaemia
Beta2-adrenergic agonists may produce significant hypokalaemia in some patients, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation. In patients with severe COPD, hypokalaemia may be potentiated by hypoxia and concomitant treatment (see section 4.5), which may increase the susceptibility to cardiac arrhythmias.
Hyperglycaemia
Inhalation of high doses of beta2-adrenergic agonists may produce increases in plasma glucose.
Anaesthesia
Caution needs to be taken in case of a planned operation with halogenated hydrocarbon anaesthetics due to an increased susceptibility to the adverse cardiac effects of beta agonist bronchodilators.
Yanimo Respimat should not be used in conjunction with any other medications containing long-acting beta2-adrenergic agonists.
Patients who have been taking inhaled, short-acting beta2-adrenergic agonists on a regular basis (e.g. four times a day) should be instructed to use them only for symptomatic relief of acute respiratory symptoms.
Yanimo Respimat should not be used more frequently than once daily.
Hypersensitivity
As with all medications, immediate hypersensitivity reactions may occur after administration of Yanimo Respimat.
4.5 Interaction with other medicinal products and other forms of interaction
Although no formal in vivo drug interaction studies have been performed between Yanimo Respimat and other drugs, inhaled Yanimo Respimat has been used concomitantly with other COPD medicinal products, including short acting sympathomimetic bronchodilators and inhaled corticosteroids without clinical evidence of drug interactions.
Anticholinergic agents
The co-administration of tiotropium bromide, one component of Yanimo Respimat, with other anticholinergic containing drugs has not been studied and therefore is not recommended.
Adrenergic agents
Concomitant administration of other adrenergic agents (alone or as part of combination therapy) may potentiate the undesirable effects of Yanimo Respimat.
Xanthine derivatives, steroids or diuretics
Concomitant treatment with xanthine derivatives, steroids, or non-potassium sparing diuretics may potentiate any hypokalemic effect of adrenergic agonists (see section 4.4).
Beta-blockers
Beta-adrenergic blockers may weaken or antagonise the effect of olodaterol. Cardioselective beta-blockers could be considered, although they should be administered with caution.
MAO inhibitors and tricyclic antidepressants. QTc Prolonging drugs Monamine oxidase inhibitors or tricyclic antidepressants or other drugs known to prolong the QTc interval may potentiate the action of Yanimo Respimat on the cardiovascular system.
Pharmacokinetic Drug Drug interactions
No relevant effect on systemic exposure to olodaterol has been observed in drug-drug interaction studies with co-administration of fluconazole, used as model inhibitor of CYP2C9.
Co-administration of ketoconazole as potent P-gp and CYP3A4 inhibitor increased systemic exposure to olodaterol by approximately 70%. No dose adjustment of Yanimo Respimat is necessary.
In vitro investigations have shown that olodaterol does not inhibit CYP enzymes or drug transporters at the plasma concentrations achieved in clinical practice.
4.6 Fertility, pregnancy and lactation
Pregnancy
Tiotropium
There is a very limited amount of data from the use of tiotropium in pregnant women. Animal studies do not indicate direct or indirect harmful effects with respect to reproductive toxicity at clinically relevant doses (see 5.3).
Olodaterol
For olodaterol no clinical data on exposed pregnancies are available. Preclinical data for olodaterol revealed effects typical for beta-adrenergic agonists at high multiples of the therapeutic doses (see section 5.3).
As a precautionary measure, it is preferable to avoid the use of Yanimo Respimat during pregnancy.
Like other beta2-adrenergic agonists, olodaterol a component of Yanimo Respimat may inhibit labour due to a relaxant effect on uterine smooth muscle.
Breast-feeding
Clinical data from nursing women exposed to tiotropium and/or olodaterol are not available.
In animal studies for both tiotropium and olodaterol the substances and/or their metabolites have been detected in the milk of lactating rats, but it is not known whether tiotropium and/or olodaterol passes into human breast milk.
A decision on whether to continue/discontinue breast-feeding or to continue/discontinue therapy with Yanimo Respimat should be made taking into account the benefit of breast-feeding to the child and the benefit of Yanimo Respimat therapy to the woman.
Fertility
Clinical data on fertility are not available for tiotropium and olodaterol or the combination of both components. Preclinical studies performed with the individual components tiotropium and olodaterol showed no indication of any adverse effect on fertility (see 5.3).
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed.
However, patients should be advised that dizziness and blurred vision have been reported with the use of Yanimo Respimat. Therefore, caution should be recommended when driving a car or operating machinery. If patients experience such symptoms, they should avoid potentially hazardous tasks such as driving or operating machinery.
4.8 Undesirable effects
a. Summary of the safety profile
Many of the listed undesirable effects can be assigned to the anticholinergic properties of tiotropium bromide or to the b2-adrenergic properties of olodaterol, the components of Yanimo Respimat
b. Tabulated summary of adverse reactions
The frequencies assigned to the undesirable effects listed below are based on the crude incidence rates of adverse drug reactions (i.e. events attributed to Yanimo Respimat) observed in the tiotropium 5 microgram/olodaterol 5 microgram dose group (1302 patients), pooled from 5 active or placebo-controlled, parallel group clinical trials in COPD patients with treatment periods ranging between 4 and 52 weeks.
Adverse reactions reported in all clinical trials with Yanimo Respimat are shown below according to system organ class.
These also include all adverse reactions previously reported with one of the individual components
Frequency is defined using the following convention:
Very common fej/10); common (>1/100 to <1/10); uncommon fid/1,000 to <1/100); rare (>1/10,000 to <1/1,000); very rare (<1/10,000), not known (cannot be estimated from the available data)
|
System Organ Class |
Adverse reaction |
Frequency |
|
Infections and infestations |
Nasopharyngitis |
rare |
|
Metabolism and nutrition disorders |
Dehydration |
not known |
|
Nervous system disorders |
Dizziness |
uncommon |
|
Insomnia |
uncommon | |
|
Headache |
uncommon | |
|
Eye disorders |
Vision blurred |
rare |
|
Glaucoma |
not known | |
|
Intraocular pressure increased |
not known | |
|
Cardiac disorders |
Atrial fibrillation |
uncommon |
|
Palpitations |
uncommon | |
|
Tachycardia |
uncommon | |
|
Supraventricular tachycardia |
rare | |
|
Vascular disorders |
Hypertension |
uncommon |
|
Respiratory, thoracic and mediastinal disorders |
Cough |
uncommon |
|
Dysphonia |
rare | |
|
Epistaxis |
rare | |
|
Laryngitis |
rare | |
|
Pharyngitis |
rare | |
|
Bronchospasm |
not known | |
|
Sinusitis |
not known | |
|
Gastrointestinal disorders |
Dry mouth |
common |
|
Constipation |
uncommon |
Musculoskeletal and connective tissue disorders
Renal and urinary disorders
rare
Gingivitis
Skin and subcutaneous tissue disorders, Immune system disorders
|
Nausea |
rare |
|
Oropharyngeal candidiasis |
rare |
|
Intestinal obstruction Ileus paralytic |
not known |
|
Dental caries |
not known |
|
Dysphagia |
not known |
|
Gastrooesophageal reflux disease |
not known |
|
Glossitis |
not known |
|
Stomatitis |
not known |
|
Angioedema |
rare |
|
Urticaria |
rare |
|
Hypersensitivity |
rare |
|
Pruritus |
rare |
|
Anaphylactic reaction |
not known |
|
Rash |
not known |
|
Dry skin |
not known |
|
Skin infection and skin ulcer |
not known |
|
Back pain1 |
rare |
|
Arthralgia |
rare |
|
Joint swelling |
not known |
|
Urinary retention |
rare |
|
Dysuria |
rare |
|
Urinary tract infection |
not known |
undesirable effects reported with Yanimo Respimat, but not with the individual components
c. Description of selected adverse reactions
Yanimo Respimat combines anticholinergic and B2-adrenergic properties due to its components tiotropium and olodaterol.
Anticholinergic adverse reaction profile
In the long term 52-weeks clinical trials with Yanimo Respimat, the most frequently observed undesirable anticholinergic effect was dry mouth which occurred in approximately 1.7% of patients treated with Yanimo Respimat and in 2.7% and 1% in
the tiotropium 5 microgram and olodaterol 5 microgram arms, respectively. Dry mouth led to discontinuation in 1 of 1,029 patients (0.1 %) treated with Yanimo Respimat.
Serious undesirable effects consistent with anticholinergic effects include glaucoma, constipation, intestinal obstruction including ileus paralytic and urinary retention.
B-adrenergic adverse reaction profile
In the long term 52-weeks clinical trials with Yanimo Respimat, the most frequently observed B-adrenergic undesirable effects were palpitations, tachycardia and hypertension.
Olodaterol, one component of Yanimo Respimat is a member of the therapeutic class of long-acting beta2-adrenergic agonists. Therefore the occurrence of other undesirable effects related to the beta-adrenergic agonist class, which are not listed above, should be taken into consideration, such as, arrhythmia, myocardial ischaemia, angina pectoris, hypotension, tremor, nervousness, muscle spasms, fatigue, malaise, hypokalemia, hyperglycemia, and metabolic acidosis.
d. Other special populations
An increase in anticholinergic effect may occur with increasing age.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard
4.9 Overdose
There is limited information on overdosing with Yanimo Respimat. Yanimo Respimat has been studied up to 5 microgram / 10 microgram (tiotropium/olodaterol) in COPD patients and up to 10 microgram / 40 microgram (tiotropium/olodaterol) in healthy subjects; no clinically relevant effects were observed. An overdose could lead to exaggerated anti-muscarinic effects of tiotropium and/or exaggerated f>2 agonists effects of olodaterol.
Symptoms
Overdose of anticholinergic tiotropium
High doses of tiotropium may lead to anticholinergic signs and symptoms.
However, there were no systemic anticholinergic adverse effects following a single inhaled dose of up to 340 microgram tiotropium bromide in healthy volunteers.
Additionally, no relevant adverse events, beyond dry mouth/throat and dry nasal mucosa were observed following 14-day dosing of up to 40 microgram tiotropium inhalation solution in healthy volunteers with the exception of pronounced reduction in salivary flow from day 7 onwards.
Overdose of fi2-agonist olodaterol
An overdose of olodaterol is likely to lead to exaggerated effects typical of beta2-adrenergic agonists, e.g. myocardial ischaemia, hypertension or hypotension, tachycardia, arrhythmias, palpitation, dizziness, nervousness, insomnia, anxiety, headache, tremor, dry mouth, muscle spasms, nausea, fatigue, malaise, hypokalemia, hyperglycemia, and metabolic acidosis.
Treatment of overdose
Treatment with Yanimo Respimat should be discontinued. Supportive and symptomatic treatment is indicated. Serious cases should be hospitalised. Use of cardioselective beta-blockers may be considered, but only subject to extreme caution since the use of beta-adrenergic blocker medication may provoke bronchospasm.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group:
Drugs for obstructive airway diseases, adrenergics in combination with
anticholinergics
ATC code: R03AL06
Mechanism of action Yanimo Respimat
Yanimo Respimat is a fixed dose combination inhalation solution containing a long acting muscarinic receptor antagonist, tiotropium and a long acting beta2-adrenergic agonist, olodaterol (LAMA/LABA) which is delivered via the Yanimo Respimat soft mist inhaler device.
The two active ingredients provide additive bronchodilation due to their different mode of action. Since muscarinic receptors appear to be more prominent in the central airways while B2 adrenoceptors have a higher expression level in the peripheral airways, a combination of tiotropium and olodaterol should provide optimal bronchodilatation in all regions of the lungs.
Tiotropium
Tiotropium bromide is a long-acting, specific antagonist at muscarinic receptors. It has similar affinity to the subtypes, M1 to M5. In the airways, tiotropium bromide competitively and reversibly binds to the M3 receptors in the bronchial smooth musculature, antagonising the cholinergic (bronchoconstrictive) effects of acetylcholine, resulting in bronchial smooth muscle relaxation. The effect was dose dependent and lasted longer than 24h. As an N-quaternary anticholinergic, tiotropium bromide is topically (broncho-) selective when administered by inhalation, demonstrating an acceptable therapeutic range before systemic anticholinergic effects may occur.
Olodaterol
Olodaterol has a high affinity and high selectivity to the human beta2-adrenoceptor.
In vitro studies have shown that olodaterol has 241-fold greater agonist activity at beta2-adrenoceptors compared to betai-adrenoceptors and 2299-fold greater agonist activity compared to beta3-adrenoceptors.
The compound exerts its pharmacological effects by binding and activation of beta2-adrenoceptors after topical administration by inhalation.
Activation of these receptors in the airways results in a stimulation of intracellular adenyl cyclase, an enzyme that mediates the synthesis of cyclic-3’,5’ adenosine monophosphate (cAMP). Elevated levels of cAMP induce bronchodilation by relaxation of airway smooth muscle cells.
Olodaterol has the pre-clinical profile of a long-acting selective beta2-adrenoceptor agonist (LABA) with a fast onset of action and a duration of action of at least 24 hours.
Beta-adrenoceptors are divided into three subtypes, beta1-adrenoceptors predominantly expressed on cardiac muscle, beta2-adrenoceptors predominantly expressed on airway smooth muscle and beta3-adrenoceptors predominantly expressed on adipose tissue. Beta2-agonists cause bronchodilation. Although the beta2-adrenoceptor is the predominant adrenergic receptor in the airway smooth muscle it is also present on the surface of a variety of other cells, including lung epithelial and endothelial cells and in the heart. The precise function of beta2-receptors in the heart is not known, but their presence raises the possibility that even highly selective beta2-adrenergic agonists may have cardiac effects.
Effects on cardiac electrophysiology
Tiotropium
In a dedicated QT study involving 53 healthy volunteers, tiotropium inhalation powder 18 microgram and 54 microgram (i.e. three times the therapeutic dose) over 12 days did not significantly prolong QT intervals of the ECG.
Olodaterol
The effect of olodaterol on the QT/QTc interval of the ECG was investigated in 24 healthy male and female volunteers in a double-blind, randomised, placebo- and active (moxifloxacin) controlled study. Olodaterol at single doses of 10, 20, 30 and 50 microgram, demonstrated that compared with placebo, the mean changes from baseline in QT interval over 20 minutes to 2 hours after dosing increased dose-dependently from 1.6 (10 microgram olodaterol) to 6.5 ms (50 microgram olodaterol), with the upper limit of the two-sided 90% confidence intervals being less than 10 ms at all dose levels for individually corrected QT (QTcI).
The effect of 5 microgram and 10 microgram olodaterol on heart rate and rhythm was assessed using continuous 24-hour ECG recording (Holter monitoring) in a subset of 772 patients in the 48-week, placebo-controlled Phase 3 trials. There were no dose- or time-related trends or patterns observed for the magnitudes of mean changes in heart rate or premature beats. Shifts from baseline to the end of treatment in premature beats did not indicate meaningful differences between olodaterol 5 microgram, 10 microgram and placebo.
Yanimo Respimat
Two 52-week randomized, double-blind trials using Yanimo Respimat enrolled 5162 patients with COPD. In a pooled analysis the number of subjects with changes from baseline-corrected QTcF (Fridericia correction) interval of >30 msec at 40 minutes post-dose on day 85, 169, and 365, ranged from 3.1%, 4.7%, and 3.6% for the Yanimo Respimat group compared to 4.1%, 4.4%, and 3.6% for olodaterol 5 microgram and 3.4%, 2.3%, and 4.6% for the tiotropium 5 microgram group, respectively.
Clinical efficacy and safety
The Phase III clinical development program for Yanimo Respimat included three randomised, double-blind trials:
(i) two replicate, 52 week parallel group trials comparing Yanimo Respimat with tiotropium 5 microgram and olodaterol 5 microgram (1029 received Yanimo Respimat) [Trials 1 and 2]
(ii) one 6 week cross-over trial comparing Yanimo Respimat with tiotropium 5 microgram and olodaterol 5 microgram and placebo (139 received Yanimo Respimat) [Trial 3]
In these trials, the comparator products, tiotropium 5 microgram, olodaterol 5 microgram and placebo were administered via the Respimat inhaler.
Patient characteristics
The majority of the 5162 patients recruited in the global, 52 week trials [Trials 1 and 2] were male (73%), white (71%) or Asian (25%), with a mean age of 64.0 years. Mean post-bronchodilator FEV1 was 1.37 L (GOLD 2 [50%], GOLD 3 [39%], GOLD 4 [11%]). Mean p2-agonist responsiveness was 16.6% of baseline (0.171 L). Pulmonary medications allowed as concomitant therapy included inhaled steroids [47%] and xanthines [10%].
The 6 week trial [Trial 3] was conducted in Europe and North America. The majority of the 219 recruited patients were male (59%) and white (99%), with a mean age of 61.1 years. Mean post-bronchodilator FEVi was 1.55 L (GOLD 2 [64%], GOLD 3 [34%], GOLD 4 [2%]). Mean p2-agonist responsiveness was 15.9% of baseline (0.193 L). Pulmonary medications allowed as concomitant therapy included inhaled steroids [41%] and xanthines [4%].
Effects on lung_function
In the 52 week trials, Yanimo Respimat administered once daily in the morning, provided clear improvement in lung function within 5 minutes after the first dose compared to tiotropium 5 microgram (mean increase in FEV1 of 0.137 L for Yanimo Respimat vs. 0.058 L for tiotropium 5 microgram [p<0.0001] and 0.125 L for olodaterol 5 microgram [p=0.16]).
In both studies, significant improvements were observed in FEV1 AUC0-3h response and trough FEV1 response after 24 weeks (lung function primary endpoints) for Yanimo Respimat compared to tiotropium 5 microgram and olodaterol 5 microgram (Table 1).
Table 1 Difference in FEV1 AUC0_3h and trough FEV1 response for Yanimo Respimat compared to tiotropium 5 microgram, olodaterol 5 microgram after 24 weeks (Trials 1 and 2)
|
FEV1 AUC0-3h response |
Trough FEV1 response | |||||||
|
Trial 1 |
Trial 2 |
Trial 1 |
Trial 2 | |||||
|
n |
Mean |
n |
Mean |
n |
Mean |
n |
Mean | |
|
Yanimo Respimat versus |
522 |
-- |
502 |
-- |
521 |
497 |
-- | |
|
Tiotropium 5 microgram |
526 |
0.117 L |
500 |
0.103 L |
520 |
0.071 L |
498 |
0.050 L |
|
Olodaterol 5 microgram |
525 |
0.123 L |
507 |
0.132 L |
519 |
0.082 L |
503 |
0.088 L |
pre-treatment baseline FEVp Trial 1 = 1. p<0.0001 for all comparisons n= number of patients
6 L; Trial 2 = 1.15 L
Patients with a higher degree of reversibility at baseline generally exhibited a higher bronchodilator response with Yanimo Respimat than patients with a lower degree of reversibility at baseline.
The increased bronchodilator effects of Yanimo Respimat compared to tiotropium 5 microgram and olodaterol 5 microgram were maintained throughout the 52 week treatment period. Yanimo Respimat also improved morning and evening PEFR (peak expiratory flow rate) compared to tiotropium 5 microgram and olodaterol 5 microgram as measured by patient's daily recordings.
In the 6 week trial, Yanimo Respimat showed a significantly greater FEVi response compared to tiotropium 5 microgram, olodaterol 5 microgram and placebo (p<0.0001) over the full 24 hour dosing interval (Table 2).
Table 2 Average difference in FEV1 (L) over 3 hr, 12 hr and 24 hr and
difference in trough FEV1 (L) for Yanimo Respimat compared to
tiotropium 5 microgram, olodaterol 5 microgram and placebo after 6 weeks (Trial 3)
|
n |
3 hr average |
n |
12 hr average |
24 hr average1 |
Trough | |
|
Yanimo Respimat versus |
138 |
138 | ||||
|
Tiotropium 5 microgram |
137 |
0.109 |
135 |
0.119 |
0.110 |
0.079 |
|
Olodaterol 5 microgram |
138 |
0.109 |
136 |
0.126 |
0.115 |
0.092 |
|
Placebo |
135 |
0.325 |
132 |
0.319 |
0.280 |
0.207 |
pre-treatment baseline FEVj = 1.30 L
1 primary endpoint p<0.0001 for all comparisons
n= number of patients
Health-related Quality of Life
Yanimo Respimat showed improvement in health-related quality of life as indicated by a reduction in St. George Respiratory Questionnaire ( SGRQ) total score. After 24 weeks, there was a statistically significant improvement in mean SGRQ total score for Yanimo Respimat compared to tiotropium 5 microgram and olodaterol 5 microgram (Table 3); improvements were seen in all SGRQ domains. More patients treated with Yanimo Respimat had a clinically meaningful improvement in SGRQ total score (MCID, defined as a decrease of at least 4 units from baseline) compared to tiotropium 5 microgram (57.5% vs. 48.7%, p=0.0001) and olodaterol 5 microgram (57.5% vs. 44.8%, p<0.0001).
Table 3: SGRQ total score after 24 weeks of treatment
|
n |
Treatment Mean |
Difference to Yanimo Respimat | ||
|
(change from baseline) |
Mean (p-value) | |||
|
Total score |
Baseline |
43.5 | ||
|
Yanimo Respimat |
979 |
36.7 (-6.8) | ||
|
Tiotropium 5 microgram |
954 |
37.9 (-5.6) |
-1.23 (p=0.025) | |
|
Olodaterol 5 microgram |
954 |
38.4 (-5.1) |
-1.69 (p=0.002) | |
n= number of patients
Dyspnea
After 24 weeks, mean TDI focal score was 1.98 units for Yanimo Respimat, with a significant improvement compared to tiotropium 5 microgram (mean difference 0.36, p=0.008) and olodaterol 5 microgram (mean difference 0.42 (p=0.002).
More patients treated with Yanimo Respimat had a clinically meaningful improvement in TDI focal score (MCID, defined as a value of at least 1 unit) compared to tiotropium 5 microgram (54.9% vs. 50.6%, p=0.0546) and olodaterol 5 microgram (54.9% vs. 48.2%, p=0.0026).
Rescue Medication Use
Patients treated with Yanimo Respimat used less daytime and nighttime rescue salbutamol compared to patients treated with tiotropium 5 microgram and olodaterol 5 microgram (mean daytime rescue use for Yanimo Respimat of 0.76 occasions per day compared to 0.97 occasions per day for tiotropium 5 microgram and 0.87 occasions per day for olodaterol 5 microgram, p<0.0001; mean nighttime rescue use for Yanimo Respimat of 1.24 occasions per day compared to 1.69 occasions per day for tiotropium 5 microgram and 1.52 occasions per day for olodaterol 5 microgram,
p<0.0001).
Patient Global Rating
Patients treated with Yanimo Respimat perceived a greater improvement in their respiratory condition compared to tiotropium 5 microgram and olodaterol 5 microgram, as measured by a Patients Global Rating (PGR) scale.
Exacerbations
Tiotropium 5 microgram has previously demonstrated a statistically significant reduction in risk of a COPD exacerbation compared to placebo. COPD exacerbations was included as an additional endpoint in the 52 week pivotal trials (Trials 1 and 2).
In the combined dataset, the proportion of patients experiencing at least one moderate/severe COPD exacerbation was 27.7% for Yanimo Respimat and 28.8% for tiotropium 5 microgram (p=0.39). These studies were not specifically designed to evaluate the effect of treatments on COPD exacerbations.
Inspiratory capacity, breathing discomfort and exercise endurance
The effect of Yanimo Respimat on inspiratory capacity, breathing discomfort and symptom-limited exercise endurance was investigated in three randomised, doubleblind trials in COPD patients:
(i) two replicate, 6 week cross-over trials comparing Yanimo Respimat with tiotropium 5 microgram, olodaterol 5 microgram and placebo during constant work rate cycling (450 received Yanimo Respimat) [Trials 4 and 5]
(ii) one 12 week parallel group trial comparing Yanimo Respimat with placebo during constant work rate cycling (139 received Yanimo Respimat) and constant speed walking (sub-set of patients) [Trial 6]
Yanimo Respimat significantly improved inspiratory capacity at rest two hours postdose compared to tiotropium 5 microgram (0.114 L, p<0.0001; Trial 4, 0.088 L, p=0.0005; Trial 5), olodaterol 5 microgram (0.119 L, p<0.0001; Trial 4, 0.080 L, p=0.0015; Trial 5) and placebo (0.244 L, p<0.0001; Trial 4, 0.265 L, p<0.0001; Trial 5) after 6 weeks.
In Trials 4 and 5, Yanimo Respimat significantly improved endurance time during constant work rate cycling compared to placebo after 6 weeks (Trial 4: geometric mean endurance time of 454 s for Yanimo Respimat compared to 375 seconds for placebo (20.9% improvement, p<0.0001); Trial 5: geometric mean endurance time of 466 seconds for Yanimo Respimat compared to 411 seconds for placebo (13.4% improvement, p<0.0001).
In Trial 6, Yanimo Respimat significantly improved endurance time during constant work rate cycling compared to placebo after 12 weeks (geometric endurance time of 528 seconds for Yanimo Respimat compared to 464 seconds for placebo (13.8% improvement, p=0.021).
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with Yanimo Respimat in all subsets of the paediatric population in chronic obstructive pulmonary disease (COPD) as per decision on class waivers (see section 4.2 for information on paediatric use).
5.2 Pharmacokinetic properties
a. General Introduction
When tiotropium and olodaterol were administered in combination by the inhaled route, the pharmacokinetic parameters for each component were similar to those observed when each active substance was administered separately.
Tiotropium and olodaterol demonstrate linear pharmacokinetics in the therapeutic range. On repeated once-daily inhalation administration, steady state of tiotropium is reached by day 7. Steady state of olodaterol is achieved after 8 days of once-daily inhalation, and accumulation is up to 1.8-fold as compared to a single dose.
b. General Characteristics of the Active Substance after Administration of the Medicinal Product
Absorption
Tiotropium: Urinary excretion data from young healthy volunteers suggests that approximately 33% of the dose inhaled via the RESPIMAT inhaler reaches the systemic circulation. The absolute bioavailability from an orally administered
solution was found to be 2-3%. Maximum tiotropium plasma concentrations are observed 5-7 minutes after the inhalation via RESPIMAT.
Olodaterol: In healthy volunteers the absolute bioavailability of olodaterol following inhalation was estimated to be approximately 30%, whereas the absolute bioavailability was below 1% when given as an oral solution. Maximum olodaterol plasma concentrations generally are reached within 10 to 20 minutes following drug inhalation via RESPIMAT.
Distribution
Tiotropium has a plasma protein binding of 72% and shows a volume of distribution of 32 L/kg. Studies in rats have shown that tiotropium does not penetrate the blood-brain barrier to any relevant extent.
Olodaterol has a plasma protein binding of approximately 60% and shows a volume of distribution of 1110 L. Olodaterol is a substrate for the P-gp, OAT1, OAT3 and OCT1 transporter. Olodaterol is not a substrate for the following transporters: BCRP, MRP, OATP2, OATP8, OATP-B, OCT2 and OCT3.
Biotransformation
Tiotropium: The extent of metabolism is small. This is evident from 74% of an intravenous dose being excreted in the urine as unchanged drug. The ester tiotropium is nonenzymatically cleaved into its alcohol and acid component (N-methylscopine and dithienylglycolic acid, respectively), both not binding to muscarinic receptors. In vitro experiments with human liver microsomes and human hepatocytes suggest that some further drug (<20% of the dose after intravenous administration) is metabolised by cytochrome P450 (CYP) 2D6 and 3A4 dependent oxidation and subsequent glutathion conjugation to a variety of Phase II-metabolites.
Olodaterol is substantially metabolized by direct glucuronidation and by O-demethylation at the methoxy moiety followed by conjugation. Of the six metabolites identified, only the unconjugated demethylation product binds to b2-receptors; this metabolite however is not detectable in plasma after chronic inhalation of the recommended therapeutic dose or doses of up to 4-fold higher. Cytochrome P450 isozymes CYP2C9 and CYP2C8, with negligible contribution of CYP3A4, are involved in the O-demethylation of olodaterol, while uridine diphosphate glycosyl transferase isoforms UGT2B7, UGT1A1, 1A7 and 1A9 were shown to be involved in the formation of olodaterol glucuronides.
Elimination
Tiotropium: The total clearance in healthy volunteers is 880 mL/min. Intravenously administered tiotropium is mainly excreted unchanged in urine (74%). After inhalation by COPD patients to steady-state, urinary excretion is 18.6% of the dose, the remainder being mainly non-absorbed drug in gut that is eliminated via the faeces. The renal clearance of tiotropium exceeds the glomerular filtration rate, indicating active secretion into the urine. The effective half-life of tiotropium following inhalation by COPD patients ranges between 27 and 45 h.
Olodaterol: Total clearance of olodaterol in healthy volunteers is 872 mL/min, and renal clearance is 173 mL/min. Following intravenous administration of [14C]-labelled olodaterol, 38% of the radioactive dose was recovered in the urine and 53% was recovered in faeces. The amount of unchanged olodaterol recovered in the urine after intravenous administration was 19%. Following oral administration, only 9% of the radioactivity (0.7% unchanged olodaterol) was recovered in urine, while the major portion was recovered in faeces (84%). More than 90% of the dose was excreted within 6 and 5 days following intravenous and oral administration, respectively. Following inhalation, excretion of unchanged olodaterol in urine within the dosing interval in healthy volunteers at steady state accounted for 5-7% of the dose. Olodaterol plasma concentrations after inhalation decline in a multiphasic manner with a terminal half-life of approximately 45 hours.
c. Characteristics in Patients
Tiotropium: As expected for all predominantly renally excreted drugs, advancing age was associated with a decrease of tiotropium renal clearance from 347 mL/min in COPD patients <65 years to 275 mL/min in COPD patients >65 years. This did not result in a corresponding increase in AUC0-6,ss or Cmax,ss values.
Olodaterol: A pharmacokinetic meta-analysis utilizing data from 2 controlled clinical trials that included 405 patients with COPD and 296 patients with asthma showed that no dose adjustment is necessary due to effects of age, gender and weight on systemic exposure to olodaterol.
Race
Olodaterol: Comparison of pharmacokinetic data within and across studies with olodaterol revealed a trend for higher systemic exposure in Japanese and other Asians than in Caucasians.
No safety concerns were identified in clinical studies with olodaterol in Caucasians and Asians of up to one year with olodaterol Respimat at doses up to twice the recommended therapeutic dose.
Renal Insufficiency
Tiotropium: Following once daily inhaled administration of tiotropium to steady-state in COPD patients with mild renal impairment (CLcr 50-80 mL/min) resulted in slightly higher AUC0-6ss (between 1.8 to 30% higher) and similar Cmaxss compared to patients with normal renal function (CLcr >80 mL/min). In subjects with moderate to severe renal impairment (CLcr <50 ml/min) intravenous administration of tiotropium resulted in twofold higher total exposure (82% higher AUC0-4h and 52% higher Cmax) compared to subjects with normal renal function, which was confirmed by observations after dry powder inhalation.
Olodaterol: There were no clinically relevant increases of systemic exposure in patients with renal impairment.
Hepatic Insufficiency
Tiotropium: Liver insufficiency is not expected to have any relevant influence on tiotropium pharmacokinetics. Tiotropium is predominantly cleared by renal elimination (74% in young healthy volunteers) and simple non-enzymatic ester cleavage to pharmacologically inactive products.
Olodaterol: There was no evidence for differences in elimination of olodaterol, nor did protein binding differ, between subjects with mild or moderate hepatic impairment and their healthy controls. A study in subjects with severe hepatic impairment was not performed.
5.3 Preclinical safety data
Tiotropium + olodaterol
Effects in non-clinical studies with the combination tiotropium/olodaterol were observed only at exposures considered sufficiently in excess of the maximum human exposure indicating little relevance to clinical use.
Tiotropium
Studies on genotoxicity and carcinogenic potential revealed no special hazard for humans.
Harmful effects with respect to pregnancy, embryonal/foetal development, parturition or postnatal development could only be demonstrated at maternally toxic dose levels. Tiotropium bromide was not teratogenic in rats or rabbits. The respiratory (irritation) and urogenital (prostatitis) changes and reproductive toxicity were observed at local or systemic exposures more than five-fold the therapeutic exposure.
Olodaterol
Studies on genotoxicity and carcinogenic potential revealed no special hazard for humans.
Increased incidences were observed of mesovarian leiomyoma in rats and of uterus leiomyoma and leiomyosarcoma in mice. This is considered a class effect which is observed in rodents after long-term exposure to high doses of p2-agonists. Up to now, p2-agonists have not been associated with cancer in humans.
In rats, no teratogenic effects occurred after inhalation at doses of 1054 microgram/kg/day (> 2600 times the human exposure (AUC(0_24h)) at the dose of 5 mcg). In pregnant NZW rabbits, an inhalation dose of 2489 microgram/kg/day (approximately 7130 times the human exposure at 5 microgram based on AUC(0-24h)) of olodaterol exhibited fetal toxicity characteristically resulting from beta-adrenoceptor stimulation; these included patchy ossifications, short/bent bones, partially open eye, cleft palate, cardiovascular abnormalities. No significant effects occurred at an inhalation dose of 974 microgram/kg/day (approximately 1353 times the 5 microgram dose based on AUC(0-24h)).
6 PHARMACEUTICAL PARTICULARS
List of excipients
6.1
Benzalkonium chloride Disodium edetate Water, purified
1M Hydrochloric acid (for pH adjustment)
6.2 Incompatibilities
Not applicable.
6.3 Shelf life
3 years
In-use shelf life: 3 months
6.4 Special precautions for storage
Do not freeze.
6.5 Nature and contents of container
Type and material of the container in contact with the medicinal product:
Solution filled into a polyethylene/polypropylene cartridge with a polypropylene cap with integrated silicone sealing ring. The cartridge is enclosed within an aluminium cylinder.
Each cartridge contains 4 ml inhalation solution.
Pack sizes and devices supplied:
Single pack: 1 Respimat inhaler and 1 cartridge, providing 60 puffs (30 medicinal doses)
Double pack: 2 single packages, each containing 1 Respimat inhaler and 1 cartridge, providing 60 puffs (30 medicinal doses)
Triple pack: 3 single packages, each containing 1 Respimat inhaler and 1 cartridge, providing 60 puffs (30 medicinal doses)
Eight pack: 8 single packages, each containing 1 Respimat inhaler and one 1 cartridge, providing 60 puffs (30 medicinal doses)
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
7 MARKETING AUTHORISATION HOLDER
Boehringer Ingelheim International GmbH
Binger Strasse 173 D-55216 Ingelheim am Rhein
Germany
8 MARKETING AUTHORISATION NUMBER(S)
PL 14598/0102
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
16/06/2015
10 DATE OF REVISION OF THE TEXT
11/03/2016