Airsalb Cfc-Free Inhaler 100 Microgram/Dose
SUMMARY OF PRODUCT CHARACTERISTICS
1 NAME OF THE MEDICINAL PRODUCT
AirSalb CFC-free inhaler 100 microgram/dose
2 QUALITATIVE AND QUANTITATIVE COMPOSITION
One metered dose contains 100 micrograms of salbutamol (as sulphate). The delivered dose through the mouthpiece is 90 micrograms of salbutamol (as sulphate).
For the full list of excipients, see section 6.1.
3 PHARMACEUTICAL FORM
Pressurised inhalation, suspension
White suspension.
4 CLINICAL PARTICULARS
4.1 Therapeutic indications
Symptomatic treatment of reversible bronchoconstriction due to bronchial asthma and chronic obstructive pulmonary disease (COPD) including chronic bronchitis and emphysema.
Prophylaxis of exercise and allergen induced asthma.
AirSlab is particularly useful for the relief of symptoms of asthma, providing it does not delay the introduction and regular use of inhaled corticosteroid therapy.
AirSlab is indicated in adults, adolescents and children aged 4 to 11 years.
4.2 Posology and method of administration
AirSalb is intended for inhalation only.
Posology
The aim should be individual dosage.
Adults and adolescents aged 12 years and older Relief of attacks: 1-2 inhalations as required.
Maximum dosage: 8 inhalations per day.
To prevent allergen- or exercise-induced symptoms, two inhalations should be taken 10-15 minutes before challenge.
Paediatric population
The effect of salbutamol for children < 4 years has not yet been determined. Available data are described in section 5.1. Dosage recommendations cannot be made.
Children below 12 years of age
Relief of attacks: 1 inhalation as required. The dose may be increased to two inhalations if required.
Maximum dosage: On-demand use of AirSalb should not exceed 2 inhalations four times daily. Reliance on such frequent supplementary use, or a sudden increase in dose, indicates poorly controlled or deteriorating asthma (see section 4.4).
To prevent allergen- or exercise-induced symptoms, one inhalation, or two if necessary, should be taken 10-15 minutes before challenge. The maximum dose is up to two inhalations 4 times daily.
Method of administration Handling
A faulty inhalation technique with pressurised inhalers is very common. It is therefore important that the patient be instructed in the correct inhalation technique. The patient’s inhalation technique should be checked at visits.
AirSalb may be used with a Vortex® or AeroChamber® Plus spacer device by children and patients who find it difficult to synchronise aerosol actuation with inspiration.
For instructions on the use of the Vortex® or AeroChamber® Plus spacer device please refer to the information leaflets of the spacer devices.
Priming/Re-priming the device
Before AirSalb is used for the first time, or if it has not been used for 7 days or more, it is important to check that the spray is functioning. The protective cap should be removed, the inhaler be shaken and sprayed twice into the air.
Instructions for use
The inhalation should be performed sitting or standing, wherever possible.
1. The protective cap should be removed. The inside and outside should be checked to make sure that the mouthpiece is clean.
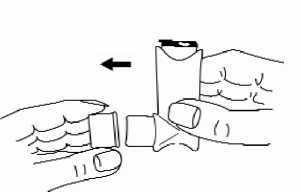
2. The inhaler should be shaken thoroughly for a couple of seconds before use.
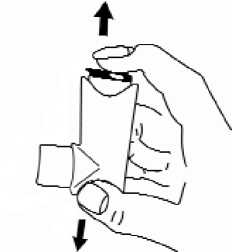
3. The inhaler should be held upright with the bottom of the container upwards. The thumb should be put on the base, below the mouthpiece. The patient should breathe out as far as is comfortable, but he should not breathe into the mouthpiece.
4. The mouthpiece should be placed in the mouth between the teeth and the lips should be closed around it without biting it.
5. Just after starting to breathe in through the mouth, the patient should press down the canister to release a puff while still breathing in steadily and deeply.
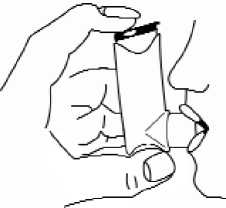
6. The breath should be held, the inhaler taken from the mouth and the finger from the top of the inhaler. The breath should be held for a few seconds, or as long as is comfortable.
7. If another puff is required, the inhaler should be kept upright and the patient should wait about half a minute before repeating steps 2 to 6.
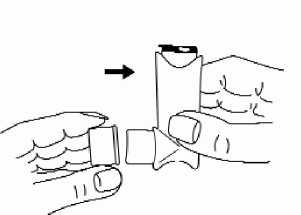
8. After use, the mouthpiece should always be covered to keep out dust and fluff. The mouthpiece cover should be replaced firmly and snapped into
position.
Cleaning
For instructions on cleaning the inhaler see section 6.6.
Inhaler content:
The inhaler should be shaken to check the remaining amount of medicine in it. AirSalb should not be used if no liquid can be detected in the inhaler while shaking.
Cold temperature use:
If the inhaler has been stored beneath 0 °C, it has to be warmed in the hands of the patient for 2 minutes, be shaken and sprayed twice into the air before use.
4.3 Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
4.4 Special warnings and precautions for use
Treatment of asthma normally follows a gradually adjusted programme, and the patient’s response to therapy must be monitored clinically and with lung function tests. An increased use of beta-2 agonist indicates deterioration of the asthma and the need for reassessment of the treatment.
Bronchodilators should not be the only or main treatment in patients with persistent asthma.
In the following cases AirSalb should only be used with caution and if strictly indicated:
- serious cardiac disorders, in particular recent myocardial infarction
- coronary heart disease, hypertrophic obstructive cardiomyopathy and tachyarrhythmia
- severe and untreated hypertension
- aneurysm
- diabetes which is difficult to control
- pheochromocytoma
- uncontrolled hyperthyroidism
- untreated hypokalaemia.
Cardiovascular effects may be seen with sympathomimetic drugs, including salbutamol. There is some evidence from post-marketing data and published literature of rare occurrences of myocardial ischaemia associated with beta agonists. Patients with underlying severe heart disease (e.g. ischaemic heart disease, arrhythmia or severe heart failure) who are receiving AirSalb should be warned to seek medical advice if they experience chest pain or other symptoms of worsening heart disease. Attention should be paid to assessment of symptoms such as dyspnoea and chest pain, as they may be of either respiratory or cardiac origin.
Hypokalaemia can be potentiated in cases of concomitant treatment with xanthine derivatives, steroids or diuretics, and in hypoxia. The serum potassium level should therefore be monitored in risk patients, especially in the treatment of acute severe asthma with high doses of AirSalb.
When initiating treatment with AirSalb in diabetics, extra checks of blood glucose levels are recommended, as beta2-agonists increase the risk of hyperglycaemia.
Non-selective beta-adrenoreceptor blockers can completely inhibit the effect of salbutamol. In patients with asthma administration of P-receptor blocking medicinal products is associated with a risk of severe bronchoconstriction. Therefore, salbutamol and non-selective P-receptor blocking medicinal products should not usually be prescribed together (see section 4.5).
Sudden and progressive deterioration of asthma control is potentially life-threatening. If the effect of AirSalb becomes less effective, the patient should be warned to seek medical advice, as repeated inhalations must not delay the initiation of other important therapy. Treatment with increased doses of corticosteroids should be considered.
As with other inhalation therapy, paradoxical bronchospasm may occur, with increased wheezing immediately after administration. Should this occur, the preparation should be immediately discontinued and replaced by alternative treatment.
4.5 Interaction with other medicinal products and other forms of interaction
Hypokalaemia may be potentiated in cases of concomitant treatment with xanthine derivatives, steroids or diuretics (see section 4.4).
Salbutamol and non-selective P-receptor blocking medicinal products should not usually be prescribed together. In patients with asthma administration of Preceptor blocking medicinal products is associated with a risk of severe bronchoconstriction.
When administering halogenated anaesthetics, e.g. halothane, methoxyflurane or enflurane, to patients treated with salbutamol an increased risk of severe dysrhythmia and hypotension must be expected. If anaesthesia with halogenated anaesthetics is planned, care should be taken to ensure that salbutamol is not used for at least 6 hours before initiation of the anaesthesia.
Monoamine oxidase inhibitors and tricyclic antidepressants may increase the risk of cardiovascular side-effects
Salbutamol induced hypokalemia may increase susceptibility to digoxin induced arrhythmias
4.6 Fertility, pregnancy and lactation
Pregnancy
Studies in animals have shown reproductive toxicity. Safety in pregnant women has not been established. Salbutamol should not be used during pregnancy unless clearly necessary.
Breastfeeding
As salbutamol is probably secreted in breast milk, its use in breast-feeding mothers requires careful consideration. A risk to the suckling child cannot be excluded. A decision on whether to continue/discontinue breast-feeding or to continue/discontinue therapy with AirSalb should be made taking into account the benefit of breast-feeding to the child and the benefit of salbutamol therapy to the woman.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed.
4.8 Undesirable effects
Undesirable effects are classified according to organ system and frequency. The frequency range is defined as very common (>1/10), common (>1/100 to <1/10), uncommon (>1/1000 to <1/100), rare (>1/10,000 to <1/1000), very rare (<1/10,000) and not known (cannot be estimated from the available data). Very common, common and uncommon undesirable effects have been obtained from clinical trials. Rare, very rare and unknown undesirable effects were generally determined from spontaneous post-marketing reports.
Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness.
|
Organ system |
Adverse reactions |
Frequency |
|
Immune system |
Hypersensitivity reactions incl. angioedema, |
Very rare |
|
disorders |
collapse, bronchospasm, hypotension, urticaria | |
|
Metabolism and nutrition disorders |
Hypokalaemia |
Rare |
|
Nervous system disorders |
Tremor, headache |
Common |
|
Hyperactivity, sleep disturbances, hyperexcitability, hallucinations |
Very rare | |
|
Cardiac disorders |
Tachycardia |
Common |
|
Palpitations |
Uncommon | |
|
Cardiac arrhythmia (e.g. atrial fibrillation, supraventricular tachycardia and extrasystoles) |
Very rare | |
|
Myocardial ischaemia* (see section 4.4) |
Not known | |
|
Vascular disorders |
Peripheral vasodilatation |
Rare |
|
Respiratory, thoracic and mediastinal disorders |
Paradoxical bronchospasm |
Very rare |
|
Gastrointestinal disorders |
Irritation in mouth and throat |
Uncommon |
|
Musculoskeletal and connective tissue disorders |
Muscle cramps |
Common |
* reported spontaneously in post-marketing data therefore frequency regarded as unknown
Undesirable effects typical of beta2-agonists, such as skeletal muscle tremor and palpitations, can occur especially at the beginning of treatment, and are often dose-dependent.
As with other inhalation therapy, paradoxical bronchospasm may occur with an immediate increase in wheezing after dosing. This should be treated immediately with an alternative presentation or a different fast-acting inhaled bronchodilator.Sabumalin should be discontinued immediately, the patient assessed, and, if necessary, alternative therapy instituted.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme (www.mhra.gov.uk/yellowcard).
4.9 Overdose
Symptoms of an overdose
In case of overdose, the adverse reactions already named may appear very rapidly and possibly to an increased extent.
Typical symptoms are:
tachycardia, palpitations, arrhythmias, agitation, dyssomnia, chest pain and severe tremor, particularly affecting hands, but also the whole body.
Gastrointestinal complaints including nausea can occur, particularly after oral intoxication.
Psychotic reactions have uncommonly been observed after excessive salbutamol doses.
In association with overdose of salbutamol, displacements of potassium into the intracellular space may occur with the consequence of hypokalaemia as well as hyperglycaemia.
Therapeutic measures in case of an overdose
Treatment of overdoses with beta-sympathomimetics is mainly symptomatic. The following measures can be recommended:
- Gastric lavage should be considered if large quantities of the medicinal product have been swallowed inadvertently. Activated charcoal and laxatives may have a positive influence on undesired absorption.
- Cardiac symptoms may be treated with a cardioselective beta-blocker, but an elevated risk that bronchospasticity occurs in patients with bronchial asthma is to be borne in mind.
- ECG monitoring is indicated for cardiac supervision.
- In case of more pronounced hypotension, volume substitution (e.g. plasma substitutes) is recommended.
The development of hypokalaemia must be expected, hence appropriate monitoring of the electrolyte balance and, if necessary, substitutions are to be recommended while heeding a possible preceding treatment with other medicinal products that can induce hypokalaemia, hyperlipidemia, ketonemia.
5 PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: selective beta-2-adrenoreceptor agonists.
ATC code: R03AC02
Salbutamol is an adrenergic beta-receptor stimulant with a selective effect on the beta2- receptors of the bronchi, which produces bronchodilatation. The bronchodilator effect occurs within a few minutes after inhalation and reaches its maximum after 30-60 minutes. It generally lasts at least 4 hours. With inhalation the bronchodilator effect is not related to the serum concentration. Adrenergic beta2-stimulants have also been shown to increase the reduced mucociliary clearance that occurs in obstructive pulmonary disease, and thus facilitate the coughing up of viscous secretion.
The active substance in AirSalb is micronised salbutamol sulphate suspended in liquid non-freon-based propellant (norflurane).
Special Populations Children < 4 years of age
Paediatric clinical studies conducted in patients < 4 years with bronchospasm associated with reversible obstructive airway disease, showed that salbutamol pressurised inhalation, suspension was well tolerated and had a safety profile comparable to that in children over 4 years, adolescents and adults.
5.2 Pharmacokinetic properties
Salbutamol administered intravenously has a half life of 4 to 6 hours and is cleared partly renally and partly by metabolism to the inactive 4'-O-sulphate (phenolic sulphate) which is also excreted primarily in the urine. The faeces are a minor route of excretion.
After administration by the inhaled route between 10 and 20% of the dose reaches the lower airways. The remainder is retained in the delivery system or is deposited in the oropharynx from where it is swallowed. The fraction deposited in the airways is absorbed into the pulmonary tissues and circulation, but is not metabolised by the lung. On reaching the systemic circulation it becomes accessible to hepatic metabolism and is excreted, primarily in the urine, as unchanged substance and as the phenolic sulphate. The swallowed portion of an inhaled dose is absorbed from the gastrointestinal tract and undergoes considerable first-pass metabolism to the phenolic sulphate. Both unchanged substance and conjugate are excreted primarily in the urine. Most of a dose of salbutamol given intravenously, orally or by inhalation is excreted within 72 hours. Salbutamol is bound to plasma proteins to the extent of 10%.
5.3 Preclinical safety data
Preclinical data revealed no special hazard for humans based on conventional studies of safety, pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential and toxicity to reproduction. The observed effects in the preclinical studies were related to the beta-adrenergic activity of salbutamol.
In common with other potent selective p2-receptor agonists, salbutamol has been shown to be teratogenic in mice when given subcutaneously. In a reproductive study, 9.3% of fetuses were found to have cleft palate at 2.5mg/kg, 4 times the maximum human oral dose. In rats, treatment at the levels of 0.5, 2.32, 10.75 and 50mg/kg/day orally throughout pregnancy resulted in no significant fetal abnormalities. The only toxic effect was an increase in neonatal mortality at the highest dose level as the result of lack of maternal care. Reproductive studies in the rabbit at doses of 50mg/kg/day orally (i.e. 78 times the maximum human oral dose) have shown fetuses with treatment related changes; these included open eyelids (ablepharia), secondary palate clefts (palatoschisis), changes in ossification of the frontal bones of the cranium (cranioschisis) and limb flexure.
The non-chlorofluorocarbon propellant, HFA 134a, has been shown to have no toxic effect at very high vapour concentrations, far in excess of those likely to be experienced by patients, in a wide range of animal species exposed daily for periods of two years.
6 PHARMACEUTICAL PARTICULARS
6.1 List of excipients
Norflurane (HFA 134a)
Anhydrous Ethanol Oleic acid
6.2 Incompatibilities
Not applicable.
6.3 Shelf life
3 years
6.4 Special precautions for storage
Do not store above 30 °C.
Store the inhaler lying flat or in an inverted position, with the mouthpiece pointing downwards.
The canister contains a pressurised liquid. Do not expose to temperatures higher than 50°C, even for a short period of time.
Protect from heat, direct sunlight and frost!
Do not pierce the container, even when empty.
6.5 Nature and contents of container
Aluminium containers with metering valve polypropylene actuator Packs containing
200 metered actuations (equivalent to 8.5 g pressurized inhalation, suspension)
2 x 200 metered actuations (equivalent to 2 x 8.5 g pressurized inhalation, suspension)
3 x 200 metered actuations (equivalent to 3 x 8.5 g pressurized inhalation, suspension)
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
Any unused medicinal product or waste material should be disposed of in accordance with local requirements.
To prevent the inhaler blocking up, it is important to clean it at least once a week, following the instructions below. If the inhaler does block up, the same cleaning instructions should be followed.
To clean the inhaler:
1 The metal canister should be pulled out of the plastic case of the inhaler and the mouthpiece cover should be removed.
2 The plastic case and the mouthpiece cover should be rinsed in warm water. If a build up of medicine is noticed around the mouthpiece, the patient should not attempt to unblock it with a sharp object, such as a pin. A mild detergent may be added to the water, then the mouthpiece should be rinsed thoroughly with clean water before drying. The metal canister should not be put into water.
3 The plastic case and the mouthpiece cover should be left to dry in a warm place. Excessive heat should be avoided.
4 The canister and mouthpiece cover should be replaced.
7 MARKETING AUTHORISATION HOLDER
Sandoz Limited Frimley Business Park,
Frimley,
Camberley,
Surrey,
GU16 7SR.
United Kingdom
8 MARKETING AUTHORISATION NUMBER(S)
PL 04416/0785
9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
03/03/2013
10 DATE OF REVISION OF THE TEXT
28/10/2015