Mylafent 75 Microgram/Hour Transdermal Patch
Read all of this leaflet carefully before you start using this
medicine because it contains important information for you
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
• If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
• These patches contain a strong pain killer.
• Ensure that old patches are removed before applying a new one.
• Patches must not be cut.
• Do not expose the patches to a heat source (such as a hot water bottle).
• If you develop a fever tell your doctor immediately.
• Follow the dosage instructions carefully and only change your patch every 72 hours.
• If your breathing becomes shallow and weak take the patch off and seek medical help.
NO PRINTINQ IN THIS AREA
Package leaflet: Information for the patient
MYLAFENT® 12 MICROGRAM/HOUR TRANSDERMAL PATCH MYLAFENT® 25 MICROGRAM/HOUR TRANSDERMAL PATCH MYLAFENT® 50 MICROGRAM/HOUR TRANSDERMAL PATCH MYLAFENT® 75 MICROGRAM/HOUR TRANSDERMAL PATCH MYLAFENT® 100 MICROGRAM/HOUR TRANSDERMAL PATCH
(Fentanyl)
What is in this leaflet:
1. What Mylafent is and what it is used for.
2. What you need to know before you use Mylafent.
3. How to use Mylafent.
4. Possible side effects.
5. How to store Mylafent.
6. Contents of the pack and other information.
1. WHAT MYLAFENT IS AND WHAT IT IS USED FOR
Fentanyl belongs to a group of strong painkillers called opioids. The painkiller, fentanyl, slowly passes from the patch, through the skin and into the body.
Adults:
Mylafent is indicated in severe chronic pain which can be adequately managed only with opioid analgesics.
Children and adolescents:
Mylafent is used for the long term treatment of severe and long lasting pain in children and adolescents aged 2 years or older who have previously been treated with other strong pain relievers and for the long term management of severe chronic pain in children receiving opioid therapy.
2. WHAT YOU NEED TO KNOW BEFORE YOU USE MYLAFENT Do not use Mylafent
• if you are allergic to fentanyl or any of the other ingredients of this medicine (listed in section 6).
• if you suffer from pain which lasts only for a short period (e.g. after a surgical procedure).
• if your central nervous system is severely impaired, e.g. by brain injury.
Do not use this medicine if any of the above apply to you or your child. If you are not sure, talk to your doctor or pharmacist before using Mylafent.
Warnings and precautions
• Mylafent is a medical product that could be life threatening to children. This is also the case with used transdermal patches.
• Bear in mind that the design of this medicinal product could be tempting to a child which in some cases may lead to a fatal outcome.
• Mylafent can have life-threatening side effects in persons that are not using prescribed opioid medicines on a regular basis.
Talk to your doctor or pharmacist before using Mylafent.
Before starting to use Mylafent you should inform your doctor if you suffer from any of the below disorders, because the risk of side effects is higher and/or your doctor may need to prescribe a lower dose of fentanyl:
• asthma, breathing difficulties or any lung disease
• slow irregular heartbeat (bradyarrhythmias)
• low blood pressure
• impaired liver function
• impaired kidney function
• if you have had a head injury or brain disease (e.g. a tumour), signs of increased intracranial pressure (e.g. headache, visual disturbances), changes in your state of consciousness or loss of consciousness or coma
• if you suffer from a condition in which muscles become weak and tire easily (myasthenia gravis).
Like some other strong painkillers, Mylafent may make you unusually drowsy, and breathe more slowly or weakly. Very rarely these breathing difficulties can be life-threatening or even fatal in people who have not used strong morphine-related painkillers (like Mylafent) or morphine before. If you, or your partner or carer, notice that you or your child are breathing much more slowly or weakly then:
* Take the patch off.
* Call a doctor, or go to your nearest hospital, straight away.
* Keep moving and talking as much as possible.
• If you develop a fever while wearing Mylafent, tell your doctor as this may affect the way the medicine passes through your skin.
• Do not expose the patch to a direct heat source such as heating pads, hot-water bottles, electric blankets, heat lamps, saunas and hot whirlpool spa baths. These may affect the way the medicine works.
• You are allowed to stay outside in the sun, but you must protect the patch with some piece of clothing during hot summer days.
Decreasing relief of pain (tolerance), physical or psychological dependence may develop if you use Mylafent for a longer period. However, this is rarely seen during treatment of pain due to cancer.
If you are an elderly patient or if you are in a very bad physical condition (cachectic) your doctor will monitor you more carefully, because it may be necessary to prescribe a lower dose.
The patches should not be cut in to smaller parts, because the quality, efficacy and safety of such divided patches have not been demonstrated.
Patch sticking to another person The patch should be used only on the skin of the person for whom it was ordered by the doctor. Cases have been reported where a patch was accidentally stuck to a family member while in close physical contact or sharing the same bed as the patch wearer. A patch sticking to another person (particularly a child) may result in an overdose. In case the patch sticks to the skin of another person, take the patch off immediately and seek medical attention.
Children and adolescents
Mylafent can be used in children and adolescents aged 2 to 16 years who have previously used opioid painkillers.
Mylafent should not be administered to children under 2 years of age because there is limited experience of use in children under that age. An exception can be made if the doctor has expressly prescribed Mylafent.
Other medicines and Mylafent Please tell your doctor or pharmacist if you are taking barbiturates (used for treating sleep disorders), buprenorphine, nalbuphine or pentazocine (other strong painkillers). It is not recommended to use these together with Mylafent.
Please tell your doctor if you are taking MAO inhibitors (e.g. moclobemide against depression or selegiline against Parkinson’s disease) or have taken them within the last 14 days. If these medicines are taken together this may enhance their toxicity.
|
Apply your patch on day |
Change your patch at the same time on | |
|
Monday |
—► |
Thursday |
|
Tuesday |
Friday | |
|
Wednesday |
Saturday | |
|
Thursday |
Sunday | |
|
Friday |
—► |
Monday |
|
Saturday |
—► |
Tuesday |
|
Sunday |
Wednesday |
If you use medicines that affect brain function it is more likely that you will have side effects, especially difficulty during breathing. This applies, for example, to:
• medicines used to treat anxiety (tranquilisers)
• some medicines used to treat depression (antidepressants)
• medicines used for treating psychological disorders (neuroleptics)
• anaesthetics. If you think you are going to have an anaesthetic, tell your doctor or dentist that you are using Mylafent
• medicines used for treating sleep disorders (hypnotics, sedatives)
• some medicines used for treating allergies or travel sickness, especially ones that make you sleepy (antihistamines/antiemetics)
• other strong-acting painkillers
• alcohol.
You should not take the medicines listed below at the same time as using Mylafent unless you are closely monitored by your doctor.
These medicines may increase the effects and side effects of Mylafent. This applies, for example to:
• Ritonavir or nelfinavir (used to treat HIV infection)
• Ketoconazole, itraconazole, fluconazole or voriconazole (used to treat fungal infections)
• Some macrolide antibiotics e.g. erythromycin, troleandomycin and clarithromycin (used to treat infections)
• Cimetidine (used to treat gastrointestinal diseases)
• Diltiazem, verapamil or amiodarone (used to treat heart disease)
Tell your doctor or pharmacist if you are using, or have recently used or might use any other medicines, including medicines obtained without a prescription.
Mylafent with food, drink and alcohol
Simultaneous use of Mylafent and alcoholic beverages increases the risk of severe adverse reactions, and may cause breathing difficulties, a fall of blood pressure, profound sedation and coma.
Pregnancy, breast-feeding and fertility
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
It is advised not to use Mylafent during labour and delivery (including caesarean section) because fentanyl may cause breathing problems in the newborn child. If you get pregnant during treatment with Mylafent consult your doctor. Do not use Mylafent if you are pregnant or breast-feeding unless your doctor considers the treatment necessary. Fentanyl passes into breast milk and may cause side effects such as sedation and severe breathing difficulties in the breast-fed infant. Any breast milk produced during treatment or within 72 hours after the removal of the last patch should be discarded.
Driving and using machines
Mylafent has major influence on the ability to drive and use machines. This has to be expected especially at the beginning of the treatment, at any change of dosage as well as in connection with alcohol or tranquilizers. If you have been using the same dose of Mylafent for a longer period of time, your doctor may decide that you are permitted to drive and use dangerous machines. Do not drive or operate dangerous machines while using Mylafent, unless your doctor has told you that such is permitted.
The medicine can affect your ability to drive as it may make you sleepy or dizzy.
• Do not drive while taking this medicine until you know how it affects you.
• It is an offence to drive if this medicine affects your ability to drive.
• However, you would not be committing an offence if:
- The medicine has been prescribed to treat a medical or dental problem and
- You have taken it according to the instructions given by the prescriber or in the information provided with the medicine and
- It was not affecting your ability to drive safely.
Talk to your doctor or pharmacist if you are not sure whether it is safe for you to drive while taking this medicine.
3. HOW TO USE MYLAFENT
Always use Mylafent exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
Your doctor will decide which strength of Mylafent is most suitable for you. Your doctor will base his judgement on: the severity of pain, your general condition and the type of pain treatment that you have received so far.
Using and changing the patches
• There is enough medicine in each patch to last 3 days (72 hours)
• You should change your patch every third day, unless your doctor has told you otherwise.
• Always remove the old patch before applying the new one.
• Always change your patch at the same time of day every 3 days (72 hours)
• Make a note of the day, date and time you apply a patch, to remind you when you need to change your patch.
• The following table shows you which day of the week to change your patch.
Where to apply the patch Adults
• Apply the patch on a flat part of your upper body or arm
Children
• Always apply the patch to the upper back to make it difficult for your child to reach it or take it off.
• Every so often check that the patch remains stuck to the skin.
• It is important your child does not remove the patch and put it in their mouth as this could be life-threatening or even fatal.
• It may take some time before the patch becomes fully effective. Therefore, your child might need additional painkillers until the patches become effective. Your doctor will advise you on this if it is needed.
• Children need to be monitored very closely for 48 hours after:
o The first patch has been put on o A higher dose patch has been put on
For you or your child, do not apply the patch on:
• The same place twice in a row
• Sensitive areas that you move a lot, cuts, spots or other skin blemishes
• Skin that is very hairy. If there is hair, do not shave it (shaving irritates the skin). Instead, clip the hair as close to the skin as possible
You should allow several days to pass before you put a
new patch on the same area of skin.
Putting a patch on
Step 1: Preparing the skin
• Make sure your skin is completely clean, dry and cool before you put the patch on.
• If you need to clean the skin, just use cold water.
• Do not use soap or any other cleansers, creams, moisturisers, oils or talc before applying the patch.
• Do not stick patch on straight after a hot bath or shower.
Step 2: Open the sachet
• Each patch is sealed in its own pouch
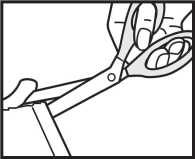
• Tear or cut off the edge of the pouch completely (if you use scissors, cut close to the sealed edge of the pouch to avoid damaging the patch) (figure 1 & figure 2).
Figure 1:
Figure 2:

Figure 3:
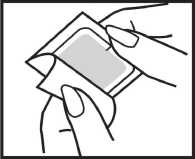
Figure 8:

Figure 4:
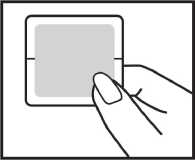
Figure 5:

Figure 6:
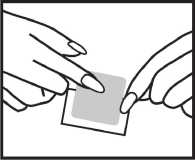
Figure 7:
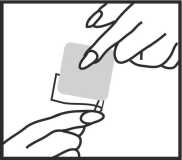
• Grasp both sides of the opened pouch and pull apart (figure 3).
• Take the patch out and use straight away (figure 4).
• Keep the empty pouch to dispose of the used patch later.
• Use each patch once only.
• Do not take the patch out of its pouch until you are ready to use it.
• Inspect the patch for any damage.
• Do not use the patch if it has been divided, cut or looks damaged.
• Never divide or cut the patch.
Step 3: Peel and press
• Make sure that the patch will be covered by loose clothing and not stuck under a tight or elasticated band.
• Carefully peel one half of the shiny plastic backing away from the centre of the patch. Try not to touch the sticky side of the patch (figure 5).
• Press this sticky part of the patch onto the skin (figure 6).
• Remove the other part of the backing and press the whole patch onto the skin with the palm of your hand (figure 7).
• Hold for at least 30 seconds. Make sure it sticks well, especially the edges, (figure 8).
Step 4: Disposing of the patch
• As soon as you take the patch off, fold it firmly in half so that the sticky side sticks to itself.
• Put it back in its original pouch and put the pouch in the bin with your household rubbish.
• Even used patches contain some medicine which may harm children, so keep your used patches out of the reach and sight of children.
Step 5: Wash
• Wash your hands afterwards with clean water.
More about using Mylafent patches
How quickly will the patches work?
• It may take up to a day before your first patch is working completely.
• Your doctor may give you extra painkillers for your first day or so.
• After this, the patch should help to relieve pain continuously so that you can stop taking other painkillers. However, your doctor may still prescribe extra painkillers from time to time.
If you forget to change the patch
• If you forget, change your patch as soon as you remember and make a note of the day and time. Change the patch again after 3 days (72 hours) as usual.
• If you are very late changing your patch, you should talk to your doctor because you might need some extra painkillers, but do not apply an extra patch.
If you use too many patches or the wrong strength patch
• If you have stuck on too many patches or the wrong strength patch, take the patches off and contact a doctor or the nearest hospital straight away.
Signs of an overdose include trouble breathing or shallow breathing, tiredness, extreme sleepiness, being unable to think clearly, walk or talk normally and feeling faint, dizzy or confused.
If the patch falls off
• If the patch falls off before it needs changing, stick a new one on straight away and make a note of the day and time. Use a new area on:
- Your upper body or arm
- Your child’s upper back
• Leave another 3 days (72 hours) before changing the patch as usual.
• If your patches keep falling off, talk to your doctor, nurse or pharmacist.
If your pain gets worse
• If your pain gets worse while you are using these patches, your doctor may try a higher strength patch, or give you extra painkillers (or both).
• If increasing the strength of the patch does not help, your doctor may stop the patches.
If you want to stop using the patches
• Talk to your doctor before you stop using these patches.
• If you have been using them for some time your body may have got used to them. Stopping suddenly may make you feel unwell.
• If you stop using the patches, don’t start again without asking your doctor first. You might need a different strength patch when you restart.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. POSSIBLE SIDE EFFECTS
Like all medicines, Mylafent can cause side effects, although not everybody gets them.
Take the patch off and tell your doctor or go to your nearest hospital straight away if you notice or suspect any of the following. You may need urgent medical treatment:
• Feeling unusually drowsy, breathing more slowly or weakly than expected. Very rarely these breathing difficulties can be life-threatening or even fatal, especially in people who have not used strong opioid painkillers before. If you notice any of the above, follow the guidance above and keep moving as much as possible.
• Complete block of the digestion channel (convulsive pain, vomiting, flatulence).
• Sudden signs of allergy such as rash, itching or hives on the skin, swelling of the face, lips, tongue or other parts of the body, shortness of breath, wheezing or trouble breathing.
• Fits.
Other side effects
Very common: may affect more than 1 in 10 people:
Drowsiness, dizziness, headache, feeling sick (nausea), being sick (vomiting), constipation.
Common: may affect up to 1 in 10 people:
Allergic reactions, awareness of unusual heart beats (also called palpitations), fast heart rate, high blood pressure, feeling unusually drowsy, weak or tired, nervousness, confused, depressed, not being able to sleep, loss of appetite, dry mouth, stomach pain, indigestion, difficulty passing urine, diarrhoea, difficulty in breathing, seeing, feeling or hearing things that are not there (hallucinations), sense of pins and needles, shaking, feeling giddy, spinning sensation, muscle spasms, swelling of hands, ankles or feet, feeling cold, excessive sweating, itchy skin, rashes or redness of skin.
Uncommon: may affect up to 1 in 100 people:
Unnatural feeling of happiness, loss of memory, agitation, disorientation, muscle twitching, decreased feeling of sensitivity especially in the skin, bluish colouration of the skin, speech disturbances, low blood pressure, slow heart beat, complete obstruction of the intestine, disorders of sexual function, body temperature changes, flu-like symptoms, drug withdrawal effects (e.g. sickness, feeling sick, anxiety, shivering, diarrhoea), a skin condition with itching, redness and a burning feeling (eczema) or other skin disorders including dermatitis.
Rare: may affect up to 1 in 1,000 people:
Small pupils, temporarily stopping breathing, slow breathing, incomplete obstruction of the small or large intestine, eczema or other skin disorders including dermatitis where the patch is placed. Skin rash and skin reddening will usually disappear within one day after the patch has been removed.
Not known: frequency cannot be estimated from the available data:
There have been reports of newborn infants experiencing withdrawal effects after their mothers have used fentanyl patches for a long time during pregnancy.
If you have been using Mylafent for some time, it might happen that Mylafent will become less effective for you so that a dose adjustment will be necessary (tolerance may develop).
Physical dependence may develop as well and you might experience withdrawal symptoms, if you do suddenly stop using the patches. Withdrawal symptoms may be nausea, vomiting, diarrhoea, anxiety and shivering.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard By reporting side effects you can help provide more information on the safety of this medicine.
5. HOW TO STORE MYLAFENT
Keep this medicine out of sight and reach of children, even after use. Significant quantities of the fentanyl remain in the transdermal patches even after use.
Do not use Mylafent after the expiry date stated on the carton and sachet. The expiry date refers to the last day of the month.
This medicinal product does not require any special storage conditions
For environmental and safety reasons, used as well as unused and out of date patches must be discarded safely or returned to the pharmacy for disposal. High quantities of fentanyl remain in the transdermal patch even after use. Retain the outer package after removing the patch for use.
Handling the patch
Used patches should be folded so that the adhesive side of the patch adheres to itself and kept in the outer package and then they should be safely discarded or delivered to the pharmacy. Accidental exposure to used and unused patches particularly in children may lead to a fatal outcome. Unused patches should be returned to the hospital pharmacy.
6. CONTENTS OF THE PACK AND OTHER INFORMATION
What Mylafent contains The active substance is fentanyl.
Each Mylafent 12 microgram/hour transdermal patch contains 2.1 mg of fentanyl in a patch size 5.25 cm2, releasing 12.5 micrograms of fentanyl per hour (the strength is described as 12 microgram/hour but the release rate of the patch is 12.5 microgram/hour).
Each Mylafent 25 microgram/hour transdermal patch contains 4.2 mg of fentanyl in a patch size 10.5 cm2, releasing 25 micrograms of fentanyl per hour.
Each Mylafent 50 microgram/hour transdermal patch contains 8.4 mg of fentanyl in a patch size 21.0 cm2, releasing 50 micrograms of fentanyl per hour.
Each Mylafent 75 microgram/hour transdermal patch contains 12.6 mg of fentanyl in a patch size 31.5 cm2, releasing 75 micrograms of fentanyl per hour.
Each Mylafent 100 microgram/hour transdermal patch contains 16.8 mg of fentanyl in a patch size 42.0 cm2, releasing 100 micrograms of fentanyl per hour.
The other ingredients are:
Polyacrylate adhesive, siliconised polyester film (protective liner), polyethylene terephthalate/ethyl vinyl acetate film (backing film) and white imprinting ink.
What Mylafent looks like and contents of the pack Mylafent is a translucent rectangular patch printed with white ink on a removable liner.
The following is printed on each patch:
Fentanyl 12 pg/h, Fentanyl 25 pg/h, Fentanyl 50 pg/h, Fentanyl 75 pg/h or Fentanyl 100 pg/h
The patch is covered by a transparent protective liner, which is removed prior to application to expose the sticky back so that it can be stuck onto the skin.
The patches come in individually heat-sealed sachets that are packaged in to a carton.
Mylafent is available in packs of 3, 4, 5, 8,10,16 and 20 transdermal patches. Not all pack sizes may be marketed.
Marketing Authorisation Holder
Mylan, Potters Bar, Hertfordshire, EN6 1TL, United Kingdom Manufacturer
Gerard Laboratories, 35/36 Baldoyle Industrial Estate,
Grange Road, Dublin 13, Ireland
and
Generics [UK] Limited, Station Close, Potters Bar, Hertfordshire, EN6 1TL, United Kingdom
Mylafent is a registered trademark.
This leaflet was last revised in September 2014
436228