Tobramycin 300 Mg/5 Ml Nebuliser Solution

Package leaflet: Information for the user
Tobramycin 300 mg/5 ml Nebuliser Solution
Tobramycin
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
• Keep this leaflet. You may need to read it again.
• If you have any further questions, ask your doctor or pharmacist.
• This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
• If you get any side effects talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
What is in this leaflet:
1. What Tobramycin is and what it is used for
2. What you need to know before you use Tobramycin
3. How to use Tobramycin
4. Possible side effects
5. How to store Tobramycin
6. Contents of the pack and other information
1. What Tobramycin is and what it is used for
What is Tobramycin for?
Tobramycin Nebuliser Solution contains a medicine called tobramycin. This is an aminoglycoside antibiotic.
Tobramycin is used in patients aged six years and older who have cystic fibrosis to treat chest infections caused by a bacteria called Pseudomonas aeruginosa.
Tobramycin fights the infection caused by Pseudomonas bacteria in your lungs, and helps to improve your breathing.
When you inhale Tobramycin, the antibiotic can get directly into your lungs to fight against the bacteria causing the infection. For the best results of this medicine, take it as this leaflet instructs you.
What is Pseudomonas aeruginosa?
This is a very common bacteria that infects nearly everyone with cystic fibrosis at some time during their lives. Some people do not get this infection until later on in their lives, while others get it very young.
This is one of the most damaging bacteria for people with cystic fibrosis. If the infection is not properly controlled, it will continue to damage your lungs causing further problems to your breathing.
Tobramycin kills the bacteria that cause infections in the lungs. The infection can be controlled successfully if the problem is tackled early.
2. What you need to know before you use Tobramycin
Do not use Tobramycin:
• if you are allergic to tobramycin, any type of aminoglycoside antibiotic, or any of the other ingredients of this medicine (listed in Section 6).
If any of the above apply to you, do not take this medicine and talk to your doctor. If you think you may be allergic, ask your doctor for advice.
Warnings and precautions
Talk to your doctor before using Tobramycin if you have or if you have ever had any of the following conditions:
• Hearing problems (including ringing in your ears and dizziness)
• Kidney problems
• Unusual difficulty in breathing with wheezing or coughing, chest tightness
• Blood in your sputum (the substance you cough up)
• Muscle weakness that lasts or becomes worse in time, symptom mostly related to condition such as myasthenia or Parkinson’s disease.
If any of these apply to you, tell your doctor before you take Tobramycin.
Inhaling medicines can cause chest tightness and wheezing and this can happen with Tobramycin. Your doctor will supervise your first dose of Tobramycin and check your lung function before and after dosing. If you are not already doing so, your doctor may ask you to use a bronchodilator, (e.g. salbutamol), before taking Tobramycin.
If you are taking Tobramycin, strains of Pseudomonas can become resistant to the treatment over time. This can mean the medicine may not work as well as it should over time. Talk to your doctor if you are concerned about this.
If you have it by an injection, tobramycin can sometimes cause hearing loss, dizziness and kidney damage, and can harm an unborn child.
Children and adolescents
Tobramycin can be taken by children and adolescents aged 6 years and older. Tobramycin should not be given to children less than 6 years old.
Older people
If you are aged 65 years and older, your doctor may perform additional tests to decide if Tobramycin is right for you.
Other medicines and Tobramycin
Please tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription.
You should not take the following medicines while you are taking Tobramycin:
• Furosemide or ethacryric acid, diuretics (“water tablets”)
• Urea or intravenous mannitol
• Other medicines which may harm your nervous system, kidneys or hearing.
The following medicines can increase the chances of harmful effects occurring if they are given to you while you are receiving injections of tobramycin:
• Amphotericin B, cefalotin, ciclosporin, tacrolimus, polymyxins: these medicines may harm your kidneys
• Platinum compounds (such as carboplatin and cisplatin): these medicines may harm your kidneys or hearing
• Anticholinesterases, (such as neostigmine and pyridostigmine), or botulinum toxin: these medicines may cause muscle weakness to appear or become worse.
If you are taking one or more of the above medicines, discuss with your doctor before you take Tobramycin.
You should not mix or dilute Tobramycin with any other medicine in your nebuliser.
If you are taking several different treatments for cystic fibrosis, you should take them in the following order:
1. bronchodilator therapy, such as salbutamol
2. chest physiotherapy
3. other inhaled medicines
4. then Tobramycin.
Please check this order with your doctor as well.
Pregnancy and breast-feeding
If you want to become pregnant or are pregnant, you should talk to your doctor about the possibility of this medicine causing any harm to you or the unborn child.
It is not known whether inhaling this medicine when you are pregnant causes side effects.
When they are given by an injection, tobramycin and other aminoglycoside antibiotics can cause harm to an unborn child, such as deafness.
If you are breast feeding your child, you should talk to your doctor before using your medicine.
Driving and using machines
Tobramycin should not affect your ability to drive and use machines.
3. How to use Tobramycin
Always use this medicine exactly as your doctor has told you. Check with your
doctor if you are not sure.
How much of this medicine you should take and how often you should take it
• The recommended dose is the same for all persons aged 6 years and older.
• Use two ampoules each day, for 28 days. Inhale the full contents of one ampoule in the morning, and one in the evening. Ideally, there should be a 12 hour gap between the doses.
• You must leave at least 6 hours between two Tobramycin inhalations.
• After taking your medicine for 28 days, you then have a 28 day break, where you don’t inhale any Tobramycin, before starting another course.
• It is important that you keep using the product twice each day during your 28 days on treatment and that you keep to the 28-day on, 28-day off cycle.
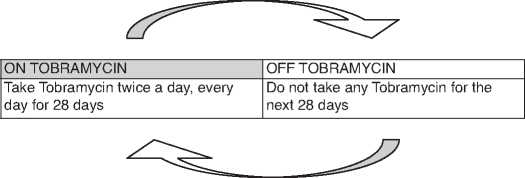
Repeat cycle
If you take more Tobramycin than you should
If you inhale too much Tobramycin you may get a very hoarse voice. Make sure you tell your doctor as soon as possible. If Tobramycin is swallowed, tell your doctor as soon as possible.
If you forget to take Tobramycin
If you forget to take Tobramycin and there are at least 6 hours to your next dose, take your dose as soon as you can. Otherwise, wait for your next dose. Do not double the dose to make up for the missed dose.
Instructions for use of Tobramycin
This part of the leaflet explains how to use, care and handle Tobramycin. Please read carefully and follow these instructions.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
The equipment you need for inhaling Tobramycin
Tobramycin should be used with a clean and dry reusable nebuliser.
The LC PLUS nebuliser (manufactured by PARI GmbH) is suitable for use with Tobramycin.

Your doctor or physiotherapist can advise you on the proper use of Tobramycin
and the equipment you need. You may need different nebulisers for your other
inhaled medicines for cystic fibrosis.
Preparing to inhale Tobramycin
• Wash your hands thoroughly with soap and water
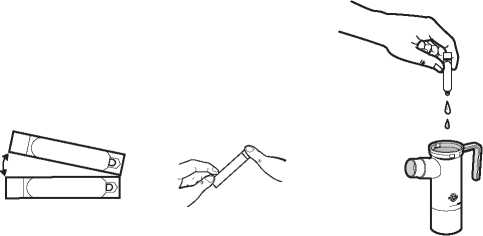
• Each Tobramycin foil pouch contains a tray with 14 ampoules. Cut or tear open the pouch. Remove one Tobramycin ampoule from the tray by gently pulling apart from any attached ampoules at the bottom tabs. Put the tray back in the foil pouch and keep it in the refrigerator.
• Lay out all the pieces of your nebuliser on a clean, dry paper or cloth towel
• Make sure you have the suitable compressor, and tubing to connect the nebuliser and compressor
• Be careful to follow the appropriate instructions for use for your type of nebuliser, you must read the leaflet provided with the nebuliser by the manufacturer. Check that your nebuliser and compressor are working properly according to the manufacturer's instructions before you start to take your medicine.
Use of Tobramycin with LC PLUS (PARI GmbH)
For more detailed instructions on the use and care of the nebuliser, please read
the leaflet provided with the PARI LC PLUS.
1. Remove the nebuliser top from the nebuliser bottom by twisting the top anticlockwise and then lifting it. Place the top on the towel and stand the nebuliser bottom upright on the towel
2. Connect one end of the tubing to the compressor air outlet. Make sure that the tubing fits snugly. Plug the compressor into the electrical outlet
3. Open the Tobramycin ampoule by holding the bottom tab with one hand and twisting off the top with your other hand. Squeeze all the contents of the ampoule into the nebuliser bottom
4. Replace the nebuliser top, put the mouthpiece and the inspiratory valve cap in place on the nebuliser, then connect the compressor as indicated in your PARI LC PLUS nebuliser leaflet
5. Turn on the compressor. Check that there is a steady mist coming from the mouthpiece. If there is no mist, check all tubing connections and that the compressor is working properly
6. Sit or stand in an upright position so that you can breathe normally
7. Place the mouthpiece between your teeth and on top of your tongue.
Breathe normally, but only through your mouth (you may use a nose clip if your doctor agrees). Try not to block the airflow with your tongue
8. Continue until all of the Tobramycin is gone and there is no longer any mist being produced. It should take about 15 minutes to take all the treatment. You may hear a spluttering sound when the nebuliser cup is empty
9. Please remember to clean and disinfect your nebuliser after treatment according to the manufacturer’s instructions. You should never use a dirty or clogged nebuliser. You should not share your nebuliser with other people.
If you are interrupted, or need to cough or rest during your treatment, turn off the compressor to save your medicine.
Turn the compressor on again when you are ready to restart your treatment. Leave out this dose if your next dose is due in less than 6 hours.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Some side effects can be serious
If you experience any of the following, stop taking Tobramycin and tell your doctor straight away:
• Unusual difficulty in breathing with wheezing or coughing and chest tightness
• Allergic reactions including hives and itching.
If you experience any of the following, tell your doctor straight away:
• Loss of hearing (ringing in the ears is a potential warning sign of hearing loss), noises (such as hissing) in the ears.
Your underlying lung disease may worsen while you are taking Tobramycin. This may be due to a lack of efficacy. Tell your doctor straight away if this happens.
Some side effects are very common
These side effects may affect more than 1 in 10 people.
• Runny or stuffy nose, sneezing
• Voice alteration (hoarseness)
• Discolouration of the substance you cough up (sputum)
• Worsening of lung function test results
If any of these affects you severely, tell your doctor.
Some side effects are common
These side effects may affect up to 1 in 10 people.
• Generally feeling unwell
• Muscle pain
• Voice alteration with sore throat and difficulty swallowing (laryngitis)
If any of these affects you severely, tell your doctor.
Other side effects:
• Itching
• Itchy rash
• Rash
• Loss of the voice
• Disturbed sense of taste
• Sore throat
If any of these affects you severely, tell your doctor.
If you have had Tobramycin at the same time as or following repeated courses of tobramycin or another aminoglycoside antibiotic by injection, hearing loss has been reported as a side effect.
Injections of tobramycin or other aminoglycosides can cause allergic reactions, hearing problems and kidney problems.
People with cystic fibrosis have many symptoms of the disease. These may still happen while taking Tobramycin, but should not be any more frequent or seem worse than before.
Reporting of side effects
If you get any side effects talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the Yellow Card Scheme: www.mhra.gov.uk/yellowcard.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Tobramycin
• Keep this medicine out of the sight and reach of children.
• Do not use this medicine after the expiry date which is stated on the box or pouch, or stamped on the ampoule
• Do not use this medicine if you notice that it has gone cloudy, or if there are bits in the solution
• Store at 2-8°C (in a refrigerator). If you don't have a refrigerator available (such as when you are transporting your medicine) you can store the foil pouches (opened or unopened) at room temperature (not above 25°C) for up to 28 days
• Do not use Tobramycin ampoules which have been stored at room
temperature for more than 28 days
• Store your ampoules in the original packaging as this medicine is sensitive to very strong light. This medicine is normally a slightly yellow colour but this can vary and sometimes it can be a darker yellow. This does not change the way this medicine works provided that the storage instructions have been followed. Never store an opened ampoule. Once opened an ampoule should be used immediately, and any remaining product should be discarded.
6. Contents of the pack and other information
What Tobramycin Nebuliser Solution contains
• The active ingredient is tobramycin. One ampoule contains 300 mg of tobramycin as a single dose
• The other ingredients are sodium chloride, water for injections, sodium hydroxide and sulphuric acid (for adjusting the level of acidity).
What Tobramycin Nebuliser Solution looks like and contents of the pack
Tobramycin Nebuliser Solution is a clear, slightly yellow solution that comes in a ready-to-use ampoule.
Ampoules are packed in foil pouches, one foil pouch contains 14 ampoules which corresponds to 7 days of treatment.
Tobramycin Nebuliser Solution is available in packs of 56, 112 or 168 ampoules, which is enough to last one, two or three cycles of treatment, respectively.
Not all pack sizes may be available.
Marketing Authorisation Holder and Manufacturer
The Marketing Authorisation Holder is:
Novartis Pharmaceuticals UK Limited,
Frimley Business Park, Frimley,
Camberley, Surrey, GU16 7SR, UK.
Manufacturered by:
Novartis Pharma GmbH Roonstrasse 25, 90429,
Nurnberg, Germany
Distributed by:
Sandoz Ltd,
Frimley Business Park, Frimley,
Camberley, Surrey, GU16 7SR, UK.
For further information please call
01276 698370 (UK only)
This leaflet was last revised in March 2016
SZ00000LT000